Abstract
Context
A recently updated Community Guide systematic review of the effectiveness of school sealant programs (SSPs) still found strong evidence that SSPs reduced dental caries among schoolchildren. This follow-up systematic review updates SSP cost and benefit information from the original 2002 review.
Evidence acquisition
Using Community Guide economic review methods, the authors searched the literature from January 2000 to November 20, 2014. The final body of evidence included 14 studies—ten from the current search and four with cost information from the 2002 review. Nine studies had information on SSP costs; six on sealant benefit (averted treatment costs and productivity losses); four on SSP net cost (cost minus benefit); and three on net cost to Medicaid of clinically delivered sealants. The authors imputed productivity losses and discounted costs/outcomes when this information was missing. The analysis, conducted in 2015, reported all values in 2014 U.S. dollars.
Evidence synthesis
The median one-time SSP cost per tooth sealed was $11.64. Labor accounted for two thirds of costs, and time to provide sealants was a major cost driver. The median annual economic benefit was $6.29, suggesting that over 4 years the SSP benefit ($23.37 at a 3% discount rate) would exceed costs by $11.73 per sealed tooth. In addition, two of four economic models and all three analyses of Medicaid claims data found that SSP benefit to society exceeded SSP cost.
Conclusions
Recent evidence indicates the benefits of SSPs exceed their costs when SSPs target schools attended by a large number of high-risk children.
CONTEXT
About 20% of U.S. children, aged 6–11 years, and 60% of adolescents, aged 12–19 years, have experienced dental caries (cavities) in a permanent tooth.1 Children aged 5–19 years living in poverty are about twice as likely to have untreated dental caries as are children from families with income >200% of the federal poverty level (25% vs 12%).2 Dental caries, if not treated, can cause pain and infection and ultimately lead to problems in eating, speaking, and learning.3
About 90% of dental caries in the permanent teeth of children occurs in the pits and fissures of posterior teeth.4 Dental sealants are clear or opaque plastic resinous materials applied to the chewing surfaces of the back teeth to prevent dental caries.5 A Cochrane review found that after 2 years, sealants prevent 80% of cavities occurring in the permanent molars compared with molars not receiving sealants.6 There is also evidence that sealants prevent early caries from progressing into a cavity.7,8
Despite strong evidence of effectiveness, sealants are underutilized, especially among children at higher risk for dental caries.4 Less than 20% of children living in poverty have received sealants compared with 32% of higher-income children.2 Increasing sealant prevalence among children is a national health objective.9 In addition, both the Centers for Medicare and Medicaid Services10 and the National Quality Forum11 have endorsed performance measures related to increased sealant prevalence among Medicaid-enrolled and privately insured children deemed to be at risk for caries, respectively.
School sealant programs (SSPs) are an effective way to deliver sealants to children who likely would not receive them otherwise. An Ohio study compared sealant prevalence among high-risk (e.g., attended school where >50% children participated in free/reduced-price meal program) and low-risk third-graders.12 Sealant prevalence among children attending schools with an SSP did not vary by risk status whereas, in schools without an SSP, sealant prevalence among low-risk children (43%) was notably higher than among high-risk children (29%). In both the 2002 and updated 2013 review, the Community Preventive Services Task Force (Task Force) issued a recommendation for use of SSPs based on strong evidence of effectiveness in preventing dental caries and evidence indicating SSPs increase the number of children receiving sealants at school.5
A 2002 Community Guide systematic review of economic evaluations of SSPs (referred to here as the 2002 economic review) found wide variation in reported costs ($18.50–$59.83 per child, 1997 U.S. dollars) and cost effectiveness (<$0 to $487 per averted cavity). The economic review included six studies conducted from the early 1970s to 1999.13 Many factors that can influence the cost and benefit of SSPs have changed since this earlier economic review. These include:
decrease in caries prevalence14;
increase in number of states allowing dental hygienists working in SSPs to assess a child’s need for sealants and to place sealants without a dentist being present15; and
increased prevalence of sealants among children14,16 and SSPs that target high-risk schools.17
In light of these changes and the updated review of the evidence of SSP effectiveness by the Task Force, it is important to conduct this systematic review5 of more recent evidence on the costs and benefits of SSPs.
This current review focuses on economic evaluations of SSPs published after 1999. Specifically, the following questions are addressed:
What is the per-child cost of SSPs and what factors influence these costs?
What is the economic benefit of sealants?
What is the cost effectiveness of SSPs?
Because many SSPs bill Medicaid for sealant placement, what are the costs and benefits of sealants delivered to Medicaid-enrolled children estimated from two perspectives, Medicaid and society?
To estimate the economic benefit of sealants, economic evaluations of sealants delivered in dental offices as well as schools were included because the evidence base for the Task Force recommendation5 included sealants delivered in both settings (i.e., assumed similar effectiveness). If effectiveness does not vary between delivery settings, the economic benefit of sealants (averted treatment costs plus averted productivity losses) also will not differ because all children, regardless of where they received sealants, will receive restorative care in a clinical setting.
EVIDENCE ACQUISITION
The team followed the general methods for economic evaluations established by the Community Guide, available at www.thecommunityguide.org/about/economics.html.
The inclusion criteria followed the standards for economic evaluation studies adopted by the Community Guide.18 Included studies met both the intervention description of the systematic review used to assess SSP effectiveness5 and the following criteria:
provided information on SSP resource costs or averted treatment costs attributable to sealants;
published in a peer-reviewed journal;
conducted in a high-income country as defined by the World Bank19; and
published in English.
A librarian at the Centers for Disease Control and Prevention searched the literature published between January 2000 and November 20, 2014. Searched databases were PubMed, EconLit, Social Sciences Citation Index, JSTOR, and the specialized databases of economic literature at the Centre for Reviews & Dissemination at the University of York. The complete search strategy is in Appendix A (available online). Reference lists of included economic studies were also searched. Two reviewers independently reviewed titles, abstracts, and keywords of each retrieved article. The full texts of ordered articles were then reviewed to identify qualifying studies. Information recorded for each study was based on the consensus of two reviewers who extracted each study independently.
Economic outcome measures considered in this review were:
cost;
economic benefit (e.g., averted treatment costs and productivity losses);
net cost (cost minus benefit); and
cost effectiveness (i.e., net cost per gained health outcome).
Economic outcomes not presented in a study were estimated if the study had sufficient information. In addition, productivity losses per child were imputed for U.S. studies that did not include this in their estimated economic benefit. To do this, the reviewers first estimated productivity losses associated with a dental visit. This value, $48.46, was the average time for a dental visit including travel (1.5 hours20) multiplied by average employee hourly compensation in 201421 ($32.31). Dental visit productivity losses were then multiplied by the number of averted cavities per child, assuming that one dental visit would be required to treat each cavity. The reviewers also discounted outcomes/costs in studies that did not do this by assuming a constant annual caries attack rate and a social discount rate of 3%. All economic values reported in this paper were converted to 2014 U.S. dollars using the U.S. city average consumer price index for dental services (Dental Consumer Price Index22). The Dental Consumer Price Index was used because the 2002 economic review found that dental labor accounted for the majority of SSP costs.13 International currencies were converted to U.S. dollars using purchasing power parity rates from the World Bank.23 Purchasing power parity rates were used because “they are less susceptible to financial flows and governmental exchange rate manipulation than are market exchange rates.”18
Once the cost and economic benefit were comparable across the studies, the median one-time intervention cost and annual economic benefit per sealed tooth were used to estimate the net cost of an SSP to society over 4 years (the time horizon reported in the effectiveness review5). Finally, one- and two-way sensitivity analyses were conducted to examine the effect on the findings from imputing productivity losses for studies that did not present them, including non-U.S. studies and studies with outlier values, and limiting SSP benefit to 4 years.
EVIDENCE SYNTHESIS
Search Results
The literature search identified 469 unique studies (Figure 1). After reviewing titles and abstracts, 413 studies were excluded. After reviewing full texts of the remaining 56 studies, 33 were excluded because they were either reviews or did not include information on costs or benefits of sealants. Among the remaining 23 economic evaluations of sealants, 13 were excluded—four because they were not conducted in high-income countries,24–27 five because the treatment arm included additional interventions,28–32 two because of insufficient information,33,34 and two because sealants were applied only to primary teeth.35,36
Figure 1.
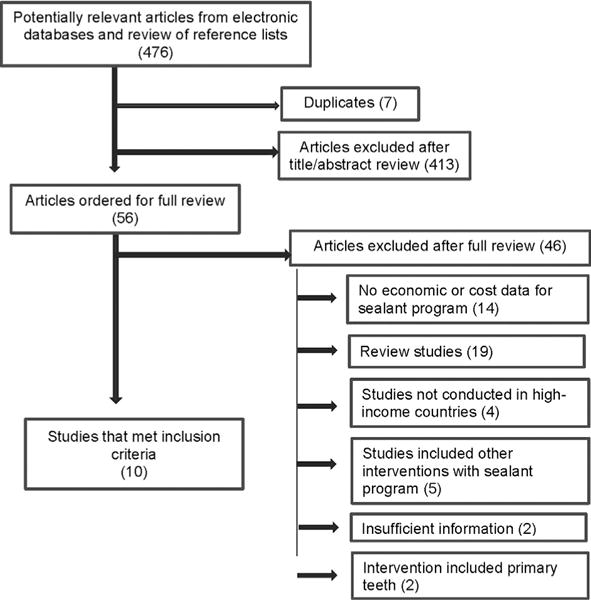
Flowchart showing 2014 economic evidence search yield.
Ten studies from the current literature search were included in this review.37–46 Only one study46 (conducted in early 1990s) included cost data for resource categories typically used by SSPs (i.e., labor, equipment, and supplies). To increase sample size, four studies with cost data47–50 from the 2002 economic review were also included. These added studies used sealant materials included in the most recent effectiveness review.5 The final body of evidence for this review included 14 studies. Analyses were conducted in 2015.
Description of Included Studies
Among the studies from the 2002 economic review, one was conducted in Australia50 and three in the U.S.47–49 Among the studies published after 1999, one was conducted in Australia,37 one in Canada,38 one in Chile,42 and seven in the U.S. (Appendix B, Table 1, available online).39–41,43–46 Among the post-1999 studies, four had cost information for at least one resource category used by programs delivering sealants in schools37,38,44,46 and one for a program delivering sealants to schoolchildren in a community clinic.42 Two of the studies with cost data and published after 1999 were conducted in the early 1990s,37,46 one in 2003,44 one in 2008,38 and one in 2009.42
For the final review, information was available for the following economic outcomes: SSP costs and cost effectiveness, economic benefit of sealants delivered in clinical or school settings, and net costs of providing sealants to Medicaid-enrolled children estimated from both the Medicaid and societal perspectives.
Economic Outcomes
School sealant program resource costs
Nine studies37,38,42,44,46–50 had cost information for 14 different SSPs (Table 1). One study38 not including equipment costs was classified as having complete cost information because excluding it would have biased costs estimates downward. Among the 12 SSPs with complete cost information, the median total cost per child was $76.09 (range, $33.36–$163.16). For the five studies reporting number of sealed teeth, the median cost per tooth was $11.64 (range, $8.34–$52.13). This value is well below the average fee reported by dentists in national surveys, $50.81 (95% CI=$50.01, $51.61),51 and the average Medicaid reimbursement reported by state Medicaid dental directors, $31.27.52
Table 1.
School Sealant Program Cost by Resource Category
| Study | Per child, $ | Total per tooth, $ | |||||
|---|---|---|---|---|---|---|---|
| Labor | Equipment | Supplies | Travel | Other | Total per child | ||
| Garcia48 1 | 32.87 | 1.03 | 6.17 | 1.77 | NR | 41.84 | – |
| Garcia48 2 | 35.30 | 2.06 | 5.27 | 3.33 | NR | 45.97 | – |
| Garcia48 3 | 62.59 | 3.00 | 9.59 | 0.41 | 0.19 | 75.80 | – |
| Garcia48 4 | 66.62 | 3.35 | 5.82 | 0.58 | NR | 76.37 | – |
| Garcia48 5 | 63.31 | 1.67 | 8.60 | 1.89 | 1.11 | 76.58 | – |
| Garcia48 6 | 77.26 | 4.16 | 7.73 | 0.56 | 1.07 | 90.77 | – |
| Calderone47 | 23.51 | 3.89 | 5.35 | 3.27 | NR | 36.00 | 8.49 |
| Morgan50 | 25.35 | 3.08 | 1.64 | 1.43 | 3.86 | 35.35 | – |
| Klein49 | NR | NR | NR | NR | NR | 116.44 | 11.64 |
| Arrow37 | 7.42 | NR | 3.12 | NR | NR | – | – |
| Marino42 | 7.19 | NRa | 25.92 | 0.24 | NR | 33.36 | 8.34 |
| Scherrer44 | 33.57 | 0.38 | NR | NR | NR | – | – |
| Werner46 | 149.52 | 1.27 | 12.37 | NR | NR | 163.16 | 52.13 |
| Bertrand38 | 115.33 | NR | 18.09 | 9.48 | 7.11 | 149.99 | 47.77 |
| Median | 35.30 | 2.53 | 6.95 | 1.60 | 1.09 | 76.09 | 11.64 |
| Median (U.S.) | 62.59 | 2.06 | 6.95 | 1.77 | 1.07 | 76.37 | 11.64 |
| M (SD) | 53.83 (40.26) | 2.39 (1.22) | 9.14 (6.56) | 2.30 (2.62) | 2.67 (2.54) | 78.47 (42.81) | 25.67 (19.90) |
School-linked program that referred children to dental clinic. Costs associated with sealant placement (e.g., equipment, clinical labor) were included in fee paid to dental clinic. Study stated fee was included in cost of supplies.
NR, not reported; U.S., studies conducted in the U.S.
The median labor cost per child was $35.30. Labor accounted for more than two thirds of total costs in ten of the 11 SSPs with data for both labor and total costs.38,42,46–48,50 The two studies with the highest labor cost per child reported sealing times of 56 minutes46 and 93 minutes38 (including exams) to seal 3.1 tooth surfaces per child—more than double the 26 minutes estimated by the reviewers using information from the Association of State and Territorial Dental Directors Best Practices for SSP website (i.e., website reported SSP could seal 15–16 children per sealant station in 6.7 hours).45,53 One study44 found that changing existing laws to allow dental hygienists instead of dentists to screen and place sealants reduced SSP costs by 18%–29% depending on the program size.
Consumable supplies were the next highest resource cost category with a median cost per child of $6.95. For the one study that itemized costs, infection control accounted for 73%.46 Supplies and labor time for infection control are incurred at the child level, suggesting that SSP costs per sealed tooth should increase with decreases in the number of at-risk teeth sealed per child and when SSPs screen and seal children at different times.
Capital equipment costs were a relatively small portion of the cost per child (median, $2.53; range, $0.38–$4.16), suggesting minimal economies of scale. The two largest programs had some of the highest costs per child.38,49 One study, however, found that because travel and set-up costs are fixed per school day, increasing the number of children seen per sealant unit per day decreased costs per child.44 Median cost per child for travel was $1.60 and for other resources was $1.09.
Economic benefit
Two studies used Medicaid claims data to estimate averted treatment costs attributable to placing sealants on permanent first molars of Medicaid-enrolled children in dental offices (Table 2; Appendix B, Table 2, available online).40,45 The reviewers estimated productivity losses and discounted costs in both studies. For the study that only reported costs at 8 years,40 annual costs (for discounting purposes) were estimated by dividing total costs by 8. This study compared reimbursements for sealants and restorations among continuously enrolled children, aged 5–7 years, with and without a dental sealant claim. Over 8 years, children not receiving sealants were three times more likely to have received a restoration (33.4% vs 10.5%). Averted restoration costs were $71.52 per child; including productivity losses would increase the economic benefit to $81.23. The annual benefit per tooth would equal $6.08.
Table 2.
Economic Benefit (Averted Costs), 2014 US$
| Study | Averted costs per child, $ | Annual averted costs per tooth, $ | |||
|---|---|---|---|---|---|
| Treatment costs | Productivity losses | Total | Annual | ||
| Dasanayake40,a | 71.52 | 9.71 | 81.23 | 10.15 | 6.08 |
| Weintraub,45 low-riska | 5.10 | 4.94 | 10.04 | 2.01 | 2.01 |
| Weintraub,45 medium-riska | 21.65 | 12.96 | 34.61 | 6.92 | 6.92 |
| Weintraub,45 high-riska | 34.92 | 18.12 | 53.04 | 10.61 | 10.61 |
| Scherrer44 | 209.97 | 23.89 | 233.86 | 25.98 | 6.50 |
| Marino42 | 12.16 | 6.62 | 18.78 | 3.13 | 0.78 |
| Griffin41,a | 36.55 | 13.47 | 50.03 | 5.56 | 5.56 |
| Quinonez43 | 73.28 | – | 73.28 | 7.33 | 7.33 |
| Median: All (Weintraub MR) | 54.04 | 12.96 | 61.65 | 7.13 | 6.29 |
| Median: Economic models | 54.92 | 13.47 | 61.65 | 6.44 | 6.03 |
| Median: Medicaid (Weintraub MR) | 46.59 | 11.33 | 57.92 | 8.54 | 6.50 |
| Median (Weintraub MR [U.S.]) | 71.52 | 13.22 | 73.28 | 7.33 | 6.50 |
| M (Weintraub MR) (SD) | 70.86 (66.34) | 13.33 (5.83) | 81.96 (71.19) | 9.85 (7.52) | 5.53 (2.20) |
Productivity losses estimated by reviewers.
MR, medium-risk; U.S., studies conducted in U.S.
A similar study in North Carolina conducted per permanent first molar stratified findings by the child’s initial caries risk.45 A molar was deemed low risk if no other first molars had received a caries-related service on an occlusal surface, medium risk if one other molar had a previous service, and high risk if two or more other molars had received a service. Although the study used 8 years of Medicaid claims data, the 5-year results are used because the effectiveness review found SSP to be effective for 4 years and the benefits in this study, which were reported for each year, stopped after 5 years. Among not-sealed low-, medium-, and high-risk first molars, the percentage receiving restorative care over 5 years was, respectively, 21.0%, 47.1%, and 58.5%. The reduction in restoration receipt and averted treatment costs per low-, medium-, and high-risk first molars was 53.3%, 62.6%, and 70.7% (Appendix B, Table 2, available online) and $5.10, $21.65, and $34.92, respectively. After including productivity losses, economic benefit equaled $10.04, $34.61, and $53.04, respectively, for low-, medium-, and high-risk teeth. The corresponding annual benefit equaled $2.01, $6.92, and $10.61.
The remaining estimates of the economic benefit from sealants were obtained from economic models—two for SSPs42,44 and two for delivering sealants in dental offices.41,43 Scherrer et al.44 modeled the benefit and costs of SSPs in Wisconsin and found that over 9 years SSPs would avert $209.97 in treatment costs and $23.89 in productivity losses per sealed child. The annual benefit per tooth sealed was $6.50. The other study42 found that over 6 years SSPs in Chile would prevent $12.16 in treatment costs and $6.62 in productivity losses per sealed child. The annual benefit per sealed tooth was $0.78.
The two models of sealants delivered in clinical settings estimated the economic benefit from the payer perspective.41,43 For this review, only findings for sealing versus not sealing one first molar per child were included, as they are more comparable to other included studies. Averted treatment costs per permanent first molar over 9 years41 and 10 years43 were $36.55 and $73.28, respectively. The reviewers could not estimate productivity losses for Quinonez and colleagues43 because the outcome was caries-free months. Adding productivity losses to economic benefit in Griffin et al.41 yielded a societal benefit of $50.03. The annual economic benefit per tooth was $5.56 and $7.33 for Griffin and colleagues41 and Quinonez et al.,43 respectively.
Among the six studies estimating benefit40–45 and using the findings for medium-risk teeth in Weintraub and colleagues,45 the estimated median annual molar attack rate was 8.0% (range, 4.9%–13.2%) and the median reduction in caries attributable to sealants 4–10 years after sealant placement was 55.1% (range, 38.7%–68.4%). The annual benefit to society ranged from $0.78 to $7.33 per tooth (median, $6.29). This value is quite similar to the median calculated from the two studies using primary data, $6.50.40,45
School sealant program net cost using median cost and benefit
Data on median SSP cost (Table 1) and benefit (Table 2) per tooth were combined to estimate SSP net cost. Assuming a 3% discount rate, the economic benefit summed over 4 years would equal $23.37 (Appendix, Table 3, available online). The SSP median one-time cost to seal a tooth was $11.64. SSP benefit exceeded cost 2 years after sealant placement and, over 4 years, saved $11.73 per sealed tooth. SSPs were still cost saving when imputed productivity losses were not included in the estimate of SSP benefit. Additional sensitivity analyses indicated that changes in assumptions did not significantly change findings (Appendix C, available online).
Net cost of delivering sealants to Medicaid-enrolled children
Two studies using claims data to estimate the net cost of sealing permanent first molars of Medicaid-enrolled children in dental offices were discussed in the section titled Economic benefit.40,45 The study conducted among Alabama children found that the 8-year per-child cost savings to Medicaid were $26.71; including productivity losses increased the cost savings to $36.41 (Appendix B, Table 4, available online). The study conducted among North Carolina children found that over 5 years, sealing a high-risk first molar was cost saving to Medicaid ($6.30). After including productivity losses, the cost saving to society from sealing medium- and high-risk first molars was $5.99 and $24.41, respectively.
The third study conducted among children who turned 6 years old between 1996 and 1999 and were continuously enrolled in Iowa Medicaid39 examined the cost per gained quality-adjusted tooth-year53 attributable to clinical delivery of sealants. For this review, the findings in the sensitivity analysis on Medicaid’s net cost to seal a permanent first molar are included. Net costs from Medicaid’s perspective were $5.41, $6.39, $16.07, and $3.93 for the upper left, upper right, lower right, and lower left first molars, respectively. When net costs were estimated from the societal perspective, sealants became cost saving or neutral (rounded down to $0.00) for all first molars with the exception of the lower right.
Possible explanations for why sealants were cost saving to Medicaid for all enrolled children in Alabama compared with only high-risk children in North Carolina and no children in Iowa are:
Medicaid-enrolled children/teeth not receiving sealants were more likely to receive restorative care in Alabama (33%) than in North Carolina (22%) or Iowa (18%).
The percentage reduction in restoration incidence was slightly higher in Alabama.
There was possible misclassification of sealed versus not sealed teeth in the Alabama study, as the analysis was conducted at the child level and did not match restoration receipt in a tooth with its sealant status but instead whether the child had at least one sealant.
One final reason why sealants may have been cost saving only for high-risk molars in North Carolina is that Medicaid reimbursement for sealants was relatively high compared with restorations. Medicaid fees for both sealants and restorations were not reported in the other two studies. The ratio of sealant to restoration reimbursements equaled 62% in North Carolina versus 35% when using relative value units54 (a measure of the relative value of resources to provide each procedure) or 37% when using private dental fees in 1999.55
School sealant program cost effectiveness: economic models
Four studies modeled the cost effectiveness of SSPs sealing first molars.38,42,44,46 Two studies were discussed in the section titled Economic Benefit.42,44 Scherrer et al.44 estimated the per-child cost of SSPs to be $67.05 (Table 3). These costs included Wisconsin’s grants to SSPs and Medicaid reimbursements for sealants. Over 9 years, SSPs saved society $166.81 per child receiving sealants. Marino and colleagues42 estimated the cost of resources used by SSPs to be $33.36 per child. Over 6 years, SSPs prevented 1.11 decayed tooth surfaces per child, with a resulting cost-effectiveness ratio of $13.13 per averted decayed tooth surface.
Table 3.
Cost Effectiveness of School Sealant Programs by Comparison Group, Societal Perspective (2014 US$)
| Study | Intervention cost, $ | Net cost, $ | Outcome | Averted/gained health outcome | Cost-effectiveness ratio |
|---|---|---|---|---|---|
| Sealant versus no sealant | |||||
| Scherrer44 | 67.05 | −166.81 | Caries | 1.85 | Cost saving |
| Marino42 | 33.36 | 14.58 | Caries | 1.11 | $13.13 |
| Werner46 | 163.16 | 1.51 | Caries | 0.93 | $1.63 |
| Delivery of sealants free of charge in clinics and schools versus clinics only | |||||
| Bertrand38 | 149.99 | −30.76 | Caries-free children | 0.01 | Cost saving |
In the third study,46 the reviewers discounted outcomes and estimated SSP economic benefit because these were not done in the study. To estimate restorative costs, the reviewers used survey data from the American Dental Association51 on the average fee for a one-surface amalgam restoration ($125.38) converted from 2009 to 2014 U.S. dollars. This value was added to estimated productivity losses per dental visit, $48.46, and then multiplied by discounted averted decay, 0.93 surfaces, to obtain an estimated economic benefit of $161.65. Net cost per averted decayed tooth surface was $1.63.
For the final study that evaluated SSP cost effectiveness for various targeting strategies,38 the reviewers compared the two strategies that were most representative of the current U.S. healthcare environment:
delivery of sealants at no patient expense to all children in both schools and private dental clinics; and
delivery of sealants with no expense to all children in private dental clinics only.
Offering sealants in schools in addition to private dental clinics was more effective (1 percentage point increase in number of children without caries) and saved $30.76 per child over 10 years.
In summary, SSPs saved societal resources because of improved dental outcomes in two studies38,44 and cost $1.6346 and $13.1342 per averted decayed tooth surface, respectively, in two studies.
DISCUSSION
Almost all studies used primary data to estimate SSP cost whereas only two of six estimates of economic benefit used primary data. The economic benefit of sealants, however, was similar for studies using both types of data. The median SSP cost to place a sealant was markedly lower than fees charged for sealants delivered in clinical settings. SSPs were cost saving when estimated with the median one-time SSP cost and median annual benefit per tooth over 4 years. The sensitivity analysis indicated these findings were robust.
Two of four economic models evaluating SSPs found that the benefit exceeded the cost. In the two remaining studies, one study42 modeled the benefit to be about one eighth the median value found in this review and the other46 found costs to be almost five times higher than that median value. Finally, clinical delivery of sealants to children enrolled in Medicaid was also found to be cost saving to society.
The median attack rate (8%) for the six studies used to estimate economic benefit per tooth was lower than the cost-saving threshold attack rate of 12% (i.e., annual caries increment of 0.47 surfaces for four molars13) found in the 2002 economic review. Possible reasons for a higher cost-saving threshold attack rate in the 2002 review are that among the three studies that found positive net costs, one reported sealant times per child exceeding 1 hour and used an early sealant material excluded in the recent effectiveness review56 and the two remaining studies did not include productivity losses in estimating the economic benefit.49,50
Limitations
Included studies had limited primary data on productivity losses associated with dental visits to restore caries. The reviewers imputed productivity losses using average employee compensation and assuming every new cavity required a separate dental visit. These assumptions may have overestimated sealant benefit. The sensitivity analysis, however, indicated that SSPs were still cost saving without imputed productivity losses. Alternatively, the economic benefit may have been underestimated because the reviewers did not impute averted travel costs (e.g., fuel costs and depreciation associated with a dental visit). Finally, the reviewers might have missed relevant studies because, using Community Guide methodology, studies not written in English were excluded.
Applicability
The generalizability of these findings to other SSPs will depend on variability in SSP effectiveness, risk status of participating children, and cost. The median effect 5–10 years after sealant placement by SSPs found in this review, 53%, was similar to the estimated value, 50%, in the effectiveness review. The reviewers are unaware of a data source with annual caries attack rates for children participating in SSPs. The median first molar attack rate reported by SSPs in 12 states funded by the Division of Oral Health (Centers for Disease Control and Prevention) for the 2013–2014 school year (6.3%),57 however, was within the range of attack rates found in studies used to estimate SSP benefit (Appendix B, Table 2, available online). The finding that labor accounted for two thirds of total SSP costs suggests that even minimal improvements in efficiency or decreases in labor costs could greatly improve SSP cost effectiveness. Labor costs will vary by the competitiveness of local labor markets and whether state law requires higher-priced labor (i.e., dentist) to be present when determining need for and placing sealants.
Other Benefits
Reduced dental caries attributable to SSPs should result in lower untreated decay prevalence as well. The benefits in terms of decreased missed school days and improved academic performance resulting from reduced untreated dental caries prevalence58–60 were not examined in this review.
Evidence Gaps
The impact of consent rates and administrative costs was not well documented in the studies in this review and may warrant further study.
CONCLUSIONS
The economic evidence indicates that the benefits of school sealant programs are greater than their costs when the programs target schools attended by a large number of children at high risk for caries.
Supplementary Material
Acknowledgments
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Footnotes
Names and affiliations of the Community Preventive Services Task Force members can be found at www.thecommunityguide.org/about/task-force-members.html.
No financial disclosures were reported by the authors of this paper.
SUPPLEMENTAL MATERIAL
Supplemental materials associated with this article can be found in the online version at http://dx.doi.org/10.1016/j.amepre.2016.10.004.
References
- 1.Dye BA, Thornton-Evans G, Li X, Iafolla TJ. Dental caries and sealant prevalence in children and adolescents in the United States, 2011–2012. NCHS Data Brief. 2015;(191):1–8. [PubMed] [Google Scholar]
- 2.Dye BA, Li X, Beltran-Aguilar ED. Selected oral health indicators in the United States, 2005–2008. NCHS Data Brief. 2012;(96):1–8. [PubMed] [Google Scholar]
- 3.U.S. DHHS. Oral health in America: a report of the Surgeon General. Rockville, MD: U.S. DHHS, National Institute of Dental and Craniofacial Research, NIH; 2000. [Google Scholar]
- 4.Beauchamp J, Caufield PW, Crall JJ, et al. Evidence-based clinical recommendations for the use of pit-and-fissure sealants. A report of the American Dental Association Council on Scientific Affairs. J Am Dent Assoc. 2008;139(3):257–268. doi: 10.14219/jada.archive.2008.0155. http://dx.doi.org/10.14219/jada.archive.2008.0155. [DOI] [PubMed] [Google Scholar]
- 5.Guide to Community Preventive Services. Preventing dental caries: school-based dental sealant delivery programs. www.thecommunityguide.org/oral/schoolsealants.html. Published 2013. Accessed May 20, 2016.
- 6.Ahovuo-Saloranta A, Forss H, Walsh T, et al. Sealants for preventing dental decay in the permanent teeth. Cochrane Database Syst Rev. 2013;3:CD001830. doi: 10.1002/14651858.CD001830.pub4. http://dx.doi.org/10.1002/14651858.CD001830.pub4. [DOI] [PubMed] [Google Scholar]
- 7.Griffin SO, Oong E, Kohn W, et al. The effectiveness of sealants in managing caries lesions. J Dent Res. 2008;87(2):169–174. doi: 10.1177/154405910808700211. http://dx.doi.org/10.1177/154405910808700211. [DOI] [PubMed] [Google Scholar]
- 8.Fontana M, Platt JA, Eckert GJ, et al. Monitoring of sound and carious surfaces under sealants over 44 months. J Dent Res. 2014;93(11):1070–1075. doi: 10.1177/0022034514551753. http://dx.doi.org/10.1177/0022034514551753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.U.S. DHHS. Healthy people 2020. Topics and objectives. Oral health. www.healthypeople.gov/2020/topics-objectives/topic/oral-health. Published 2013. Accessed September 3, 2015.
- 10.Ku L, Sharac J, Bruen B, Thomas M, Norris L. Increased use of dental services by children covered by Medicaid: 2000–2010. Medicare Medicaid Res Rev. 2013;3(3) doi: 10.5600/mmrr.003.03.b01. http://dx.doi.org/10.5600/mmrr.003.03.b01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.National Quality Forum. Prevention: Dental sealants for 6.9 year-old children at elevated caries risk. www.qualityforum.org/Qps/MeasureDetails.aspx?standardID=2508&print=0&entityTypeID=1. Accessed May 20, 2016.
- 12.Siegal MD, Detty AM. Do school-based dental sealant programs reach higher risk children? J Public Health Dent. 2010;70(3):181–187. doi: 10.1111/j.1752-7325.2009.00162.x. http://dx.doi.org/10.1111/j.1752-7325.2009.00162.x. [DOI] [PubMed] [Google Scholar]
- 13.Truman BI, Gooch BF, Sulemana I, et al. Reviews of evidence on interventions to prevent dental caries, oral and pharyngeal cancers, and sports-related craniofacial injuries. Am J Prev Med. 2002;23(1 Suppl):21–54. doi: 10.1016/s0749-3797(02)00449-x. http://dx.doi.org/10.1016/S0749-3797(02)00449-X. [DOI] [PubMed] [Google Scholar]
- 14.Dye BA, Tan S, Smith V, et al. Trends in oral health status: United States, 1988–1994 and 1999–2004. Vital Health Stat 11. 2007;(248):1–92. [PubMed] [Google Scholar]
- 15.The Pew Charitable Trusts. Expanding the dental team: increasing access to care in public settings. www.pewtrusts.org/~/media/Assets/2014/06/27/Expanding_Dental_Case_Studies_Report.pdf. Accessed May 20, 2016.
- 16.Griffin SO, Barker LK, Wei L, et al. Use of dental care and effective preventive services in preventing tooth decay among U.S. children and adolescents—Medical Expenditure Panel Survey, United States, 2003-2009 and National Health and Nutrition Examination Survey, United States, 2005-2010. MMWR Suppl. 2014;63(2):54–60. [PubMed] [Google Scholar]
- 17.Association of State and Territorial Dental Directors. Best practice approach: school-based dental sealant programs. www.astdd.org/docs/bpar-selants-update-03-2015.pdf. Published 2015. (Originally published 2003.). Accessed May 20, 2016.
- 18.Carande-Kulis VG, Maciosek MV, Briss PA, et al. Methods for systematic reviews of economic evaluations for the Guide to Community Preventive Services. Task Force on Community Preventive Services. Am J Prev Med. 2000;18(1 suppl):75–91. doi: 10.1016/s0749-3797(99)00120-8. http://dx.doi.org/10.1016/S0749-3797(99)00120-8. [DOI] [PubMed] [Google Scholar]
- 19.The World Bank. Country and lending groups. https://datahelpdesk.worldbank.org/knowledgebase/articles/906519. Published 2016. Accessed May 20, 2016.
- 20.American Dental Association. 2000 Survey of Dental Practice. Chicago, IL: American Dental Association; 2002. [Google Scholar]
- 21.Bureau of Labor Statistics. Pay and benefits. www.bls.gov/data/#wages. Accessed May 20, 2016.
- 22.Bureau of Labor Statistics. Inflation and prices. www.bls.gov/data/#prices. Accessed May 20, 2016.
- 23.The World Bank. PPP conversion factor, GDP (LCU per international $) http://data.worldbank.org/indicator/PA.NUS.PPP. Accessed May 20, 2016.
- 24.Cao HZ, Feng XP, Lo EC. The cost-effectiveness of ART and resin sealant on caries prevention [in Chinese] Shanghai Kou Qiang Yi Xue. 2002;11(1):16–18. [PubMed] [Google Scholar]
- 25.Goldman AS, Chen X, Fan M, Frencken JE. Methods and preliminary findings of a cost-effectiveness study of glass-ionomer-based and composite resin sealant materials after 2 yr. Eur J Oral Sci. 2014;122(3):230–237. doi: 10.1111/eos.12129. http://dx.doi.org/10.1111/eos.12129. [DOI] [PubMed] [Google Scholar]
- 26.Holtshousen WS, Smit A. A cost-efficiency analysis of a mobile dental clinic in the public services. SADJ. 2007;62(8):334 336–338. 340. [PubMed] [Google Scholar]
- 27.Tagliaferro EPD, Marinho DS, Pereira CCD, et al. Cost-effectiveness analysis of preventive methods for occlusal surface according to caries risk: results of a controlled clinical trial. Cad Saude Publica. 2013;29(suppl 1):S121–S130. doi: 10.1590/0102-311x00021613. http://dx.doi.org/10.1590/0102-311x00021613. [DOI] [PubMed] [Google Scholar]
- 28.Bailit H, Tryfon B, Drozdowski M. Financial feasibility of a model school-based dental program in different states. Public Health Rep. 2008;123(6):761–767. doi: 10.1177/003335490812300612. http://dx.doi.org/10.2307/25682128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Crowley SJ, Campain AC, Morgan MV. An economic evaluation of a publicly funded dental prevention programme in regional and rural Victoria: an extrapolated analysis. Community Dent Health. 2000;17(3):145–151. [PubMed] [Google Scholar]
- 30.Leskinen K, Salo S, Suni J, Larmas M. Practice-based study of the cost-effectiveness of fissure sealants in Finland. J Dent. 2008;36(12):1074–1079. doi: 10.1016/j.jdent.2008.09.005. http://dx.doi.org/10.1016/j.jdent.2008.09.005. [DOI] [PubMed] [Google Scholar]
- 31.Sakuma S, Yoshihara A, Miyazaki H, Kobayashi S. Economic evaluation of a school-based combined program with a targeted pit and fissure sealant and fluoride mouth rinse in Japan. Open Dent J. 2010;4:230–236. doi: 10.2174/1874210601004010230. http://dx.doi.org/10.2174/1874210601004010230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zabos GP, Glied SA, Tobin JN, et al. Cost-effectiveness analysis of a school-based dental sealant program for low-socioeconomic-status children: a practice-based report. J Health Care Poor Underserved. 2002;13(1):38–48. doi: 10.1353/hpu.2010.0513. http://dx.doi.org/10.1353/hpu.2010.0513. [DOI] [PubMed] [Google Scholar]
- 33.Alanen P, Holsti ML, Pienihakkinen K. Sealants and xylitol chewing gum are equal in caries prevention. Acta Odontol Scand. 2000;58(6):279–284. doi: 10.1080/00016350050217136. http://dx.doi.org/10.1080/00016350050217136. [DOI] [PubMed] [Google Scholar]
- 34.Kowash MB, Toumba KJ, Curzon ME. Cost-effectiveness of a long-term dental health education program for the prevention of early childhood caries. Eur Arch Paediatr Dent. 2006;7(3):130–135. doi: 10.1007/BF03262553. http://dx.doi.org/10.1007/BF03262553. [DOI] [PubMed] [Google Scholar]
- 35.Chi DL, van der Goes DN, Ney JP. Cost-effectiveness of pit-and-fissure sealants on primary molars in Medicaid-enrolled children. Am J Public Health. 2014;104(3):555–561. doi: 10.2105/AJPH.2013.301588. http://dx.doi.org/10.2105/ajph.2013.301588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ney JP, van der Goes DN, Chi DL. Economic modeling of sealing primary molars using a “value of information” approach. J Dent Res. 2014;93(9):876–881. doi: 10.1177/0022034514544299. http://dx.doi.org/10.1177/0022034514544299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Arrow P. Cost minimisation analysis of two occlusal caries preventive programmes. Community Dent Health. 2000;17(2):85–91. [PubMed] [Google Scholar]
- 38.Bertrand E, Mallis M, Bui NM, Reinharz D. Cost-effectiveness simulation of a universal publicly funded sealants application program. J Public Health Dent. 2011;71(1):38–45. doi: 10.1111/j.1752-7325.2010.00200.x. http://dx.doi.org/10.1111/j.1752-7325.2010.00200.x. [DOI] [PubMed] [Google Scholar]
- 39.Bhuridej P, Kuthy RA, Flach SD, et al. Four-year cost-utility analyses of sealed and nonsealed first permanent molars in Iowa Medicaid-enrolled children. J Public Health Dent. 2007;67(4):191–198. doi: 10.1111/j.1752-7325.2007.00025.x. http://dx.doi.org/10.1111/j.1752-7325.2007.00025.x. [DOI] [PubMed] [Google Scholar]
- 40.Dasanayake AP, Li Y, Kirk K, Bronstein J, Childers NK. Restorative cost savings related to dental sealants in Alabama Medicaid children. Pediatr Dent. 2003;25(6):572–576. [PubMed] [Google Scholar]
- 41.Griffin SO, Griffin PM, Gooch BF, Barker LK. Comparing the costs of three sealant delivery strategies. J Dent Res. 2002;81(9):641–645. doi: 10.1177/154405910208100913. http://dx.doi.org/10.1177/154405910208100913. [DOI] [PubMed] [Google Scholar]
- 42.Marino R, Fajardo J, Morgan M. Cost-effectiveness models for dental caries prevention programmes among Chilean schoolchildren. Community Dent Health. 2012;29(4):302–308. [PubMed] [Google Scholar]
- 43.Quinonez RB, Downs SM, Shugars D, Christensen J, Vann WF., Jr Assessing cost-effectiveness of sealant placement in children. J Public Health Dent. 2005;65(2):82–89. doi: 10.1111/j.1752-7325.2005.tb02791.x. http://dx.doi.org/10.1111/j.1752-7325.2005.tb02791.x. [DOI] [PubMed] [Google Scholar]
- 44.Scherrer CR, Griffin PM, Swann JL. Public health sealant delivery programs: optimal delivery and the cost of practice acts. Med Decis Making. 2007;27(6):762–771. doi: 10.1177/0272989X07302134. http://dx.doi.org/10.1177/0272989x07302134. [DOI] [PubMed] [Google Scholar]
- 45.Weintraub JA, Stearns SC, Rozier RG, Huang CC. Treatment outcomes and costs of dental sealants among children enrolled in Medicaid. Am J Public Health. 2001;91(11):1877–1881. doi: 10.2105/ajph.91.11.1877. http://dx.doi.org/10.2105/AJPH.91.11.1877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Werner CW, Pereira AC, Eklund SA. Cost-effectiveness study of a school-based sealant program. ASDC J Dent Child. 2000;67(2):93–97. 82. [PubMed] [Google Scholar]
- 47.Calderone JJ, Mueller LA. The cost of sealant application in a state dental disease prevention program. J Public Health Dent. 1983;43(3):249–254. doi: 10.1111/j.1752-7325.1983.tb01916.x. http://dx.doi.org/10.1111/j.1752-7325.1983.tb01916.x. [DOI] [PubMed] [Google Scholar]
- 48.Garcia AI. Caries incidence and costs of prevention programs. J Public Health Dent. 1989;49(5):259–271. doi: 10.1111/j.1752-7325.1989.tb02084.x. Spec No. [DOI] [PubMed] [Google Scholar]
- 49.Klein SP, Bohannan HM, Bell RM, Disney JA, Foch CB, Graves RC. The cost and effectiveness of school-based preventive dental care. Am J Public Health. 1985;75(4):382–391. doi: 10.2105/ajph.75.4.382. http://dx.doi.org/10.2105/AJPH.75.4.382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Morgan MV, Crowley SJ, Wright C. Economic evaluation of a pit and fissure dental sealant and fluoride mouthrinsing program in two nonfluoridated regions of Victoria, Australia. J Public Health Dent. 1998;58(1):19–27. doi: 10.1111/j.1752-7325.1998.tb02986.x. http://dx.doi.org/10.1111/j.1752-7325.1998.tb02986.x. [DOI] [PubMed] [Google Scholar]
- 51.American Dental Association. 2009 Survey of Dental Fees. Chicago, IL: American Dental Association; 2009. [Google Scholar]
- 52.American Dental Association. State innovations to improve access to oral health: a compendium update. multivu.prnewswire.com/mnr/ada/20973/#. Published 2008. Accessed May 20, 2016.
- 53.Birch S. Measuring dental health: improvements on the DMF index. Community Dent Health. 1986;3(4):303–311. [PubMed] [Google Scholar]
- 54.Relative Value Studies Inc. Relative Values for Dentists 2000. Denver, CO: Relative Value Studies Incorporated; 2000. [Google Scholar]
- 55.American Dental Association. 1999 Survey of Dental Fees. Chicago, IL: American Dental Association Survey Center; 2000. [Google Scholar]
- 56.Leake JL, Martinello BP. A four year evaluation of a a fissure sealant in a public health setting. Dent J. 1976;42(8):409–415. [PubMed] [Google Scholar]
- 57.Griffin SO. The School-Based Health Alliance 2015 meeting. Austin, TX: 2015. Measuring school sealant program efficiency. [Google Scholar]
- 58.Agaku IT, Olutola BG, Adisa AO, Obadan EM, Vardavas CI. Association between unmet dental needs and school absenteeism because of illness or injury among U.S. school children and adolescents aged 6-17 years, 2011-2012. Prev Med. 2015;72:83–88. doi: 10.1016/j.ypmed.2014.12.037. http://dx.doi.org/10.1016/j.ypmed.2014.12.037. [DOI] [PubMed] [Google Scholar]
- 59.Jackson SL, Vann, Kotch JB, Pahel BT, Lee JY. Impact of poor oral health on children’s school attendance and performance. Am J Public Health. 2011;101(10):1900–1906. doi: 10.2105/AJPH.2010.200915. http://dx.doi.org/10.2105/AJPH.2010.200915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Seirawan H, Faust S, Mulligan R. The impact of oral health on the academic performance of disadvantaged children. Am J Public Health. 2012;102(9):1729–1734. doi: 10.2105/AJPH.2011.300478. http://dx.doi.org/10.2105/AJPH.2011.300478. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


