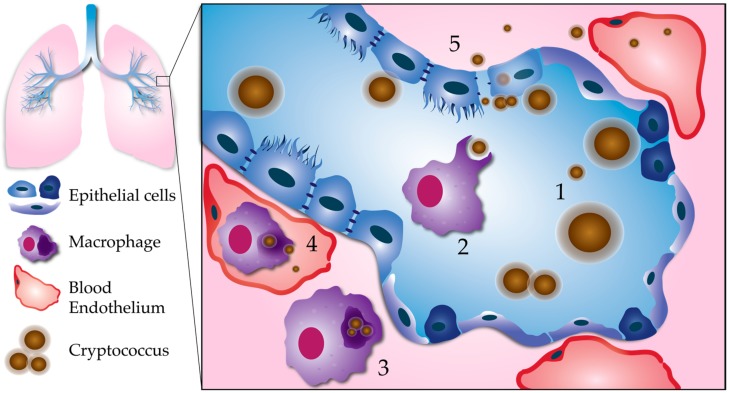
Figure 1.
Processes leading to pulmonary escape by C. neoformans. (1) Fungal factors influencing pulmonary escape: Proliferation within the lungs results in phenotypic diversity. Cell body, cell wall, and capsule enlargement promote adaptation to host stresses, and evasion of the host immune system. This reservoir of resilient cells may generate smaller cells with a greater propensity for dissemination. (2) Phagocytosis: Smaller, less encapsulated cells are more easily phagocytosed, especially with the aid of opsonization. (3) Intracellular survival: C. neoformans is able to survive and replicate within the phagolysosome of host phagocytes, such as macrophages. Macrophages containing C. neoformans act as “Trojan horses” to carry fungal cells across the respiratory epithelium. (4) Escape from macrophages: Macrophages can carry C. neoformans to distal sites, such as the brain microvasculature. C. neoformans can escape from macrophages at unknown stages in dissemination via nonlytic exocytosis, or vomocytosis. Here, we show vomocytosis occurring within an alveolar-associated capillary, but it could potentially take place at multiple sites within the body, including the blood–brain barrier. (5) Extracellular escape: C. neoformans also has the potential to escape the lungs independent of macrophages. After adhering to the respiratory epithelium, C. neoformans may cross through epithelial cells in a process called transcytosis. Lysis of epithelial cells and/or disruption of epithelial cell tight junctions could allow for C. neoformans to cross in between epithelial cells (paracellular crossing). Blood-borne extracellular C. neoformans must adapt to alkaline physiological pH (pH 7.3).