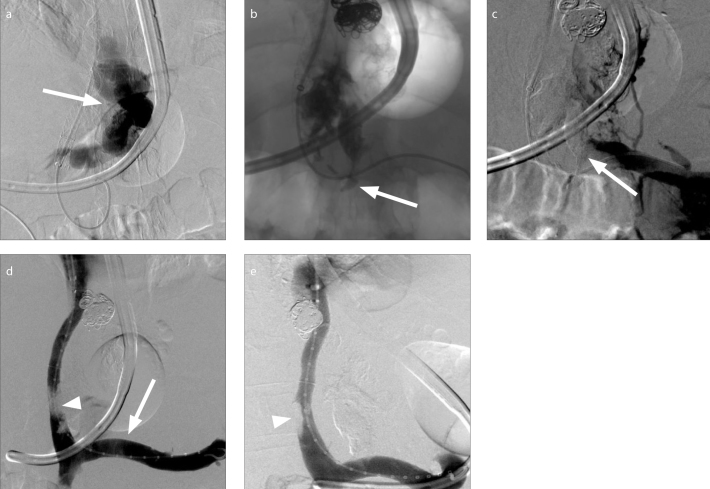
Figure 3. a–e.
A 56-year-old male with cirrhosis complicated by ascites and hemorrhaging gastroesophageal varices was referred to IR for transjugular intrahepatic portosystemic shunt (TIPS) creation and variceal embolization. Following successful TIPS creation, attempted embolization of a large, tortuous type-1 gastroesophageal varix arising from the coronary vein (a, arrow) was complicated by variceal rupture. A 2:1 n-BCA:ethiodized oil mixture was injected using the continuous column technique at the rupture site. Glue migrated into the origin of the coronary vein and splenic vein (b, arrow). Venogram (c) demonstrated glue within the coronary vein and the distal splenic vein, partially occluding the lumen of the latter vessel (c, arrow). A loop snare was used for transvenous retrieval of a section of the protruding polymer as depicted on spot fluoroscopy. Given persistent near-occlusion of the splenic vein at its junction with the superior mesenteric vein, a 13 mm Viabahn endoprosthesis (Gore Medical) was deployed (d, arrow) across the origin of the coronary vein from which glue was protruding. Completion venograms demonstrated a patent splenic vein (d, e) and TIPS without extravasation. Apparent filling defect was created by superimposed glue (d, arrowhead) and right portal thrombus (e, arrowhead), present on preoperative imaging.