Figure 1. Schematic of postulated therapeutic action of MSC exosomes in hyperoxia-induced BPD.
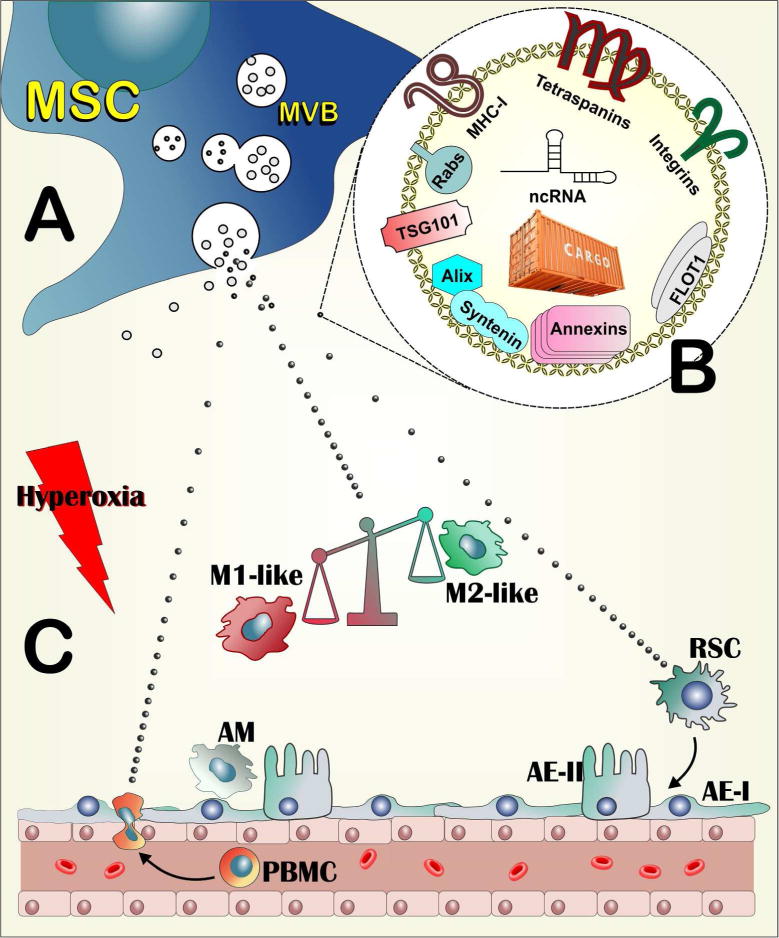
(A). MSCs routinely generate exosomes in multivesicular bodies (MVB) through the endocytic pathway. The majority of produced exosomes represent jettisoning of unwanted moieties by the cell and probably have no discernable function (larger grey symbols). Upon specific organismal or environmental cues, MSCs also produce a subpopulation of exosomes that harbor the therapeutic activity (small black symbols). (B). The therapeutic exosomes harbor cell surface components arguably involved in targeting recipient cells (Tetraspanins, Integrins) or immunomodulation, such as MHC-I. They also contain molecules associated with the pathways of their biogenesis, such as Rabs, TGS101, Alix Syntenin, Annexins and FLOT1. Their cargo includes small non-coding RNAs, but also macromolecular modules yet to be characterized. (C). The hyperoxic insult creates an inflammatory environment in the lung, which activates the alveolar macrophages (AM) and recruits circulating monocytes (PBMC) to the alveolar space. The main function of MSC exosomes is to induce a shift in macrophage polarization, tilting the balance from a destructive, M1-like inflammatory state to an anti-inflammatory, M2-like state. Additional actions of exogenously administered MSC exosomes could be the direct or indirect inhibition of PBMC recruitment to the injured lung and the direct or indirect enhancement of the activity of lung resident stem cells (RSC), leading to faster healing of injured tissue. AE-I and AE-II : Alveolar epithelial cells type I and type II respectively.
