Figure 2. Tuberculosis-related outcomes* stratified by WHO’s symptom-based approach for the management of child contacts†.
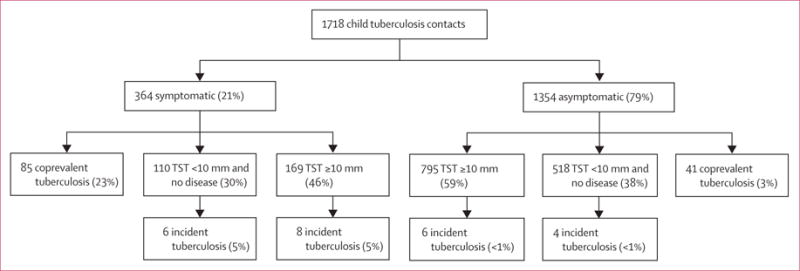
TST=tuberculin skin test. *Individuals with coprevalent disease were excluded from analyses of incident disease. In this analysis, tuberculosis infection was defined as a tuberculin skin-test induration response of ≥10 mm. Percentages might not total 100% because within-characteristic percentages were rounded to the nearest integer. †Participants were included in the pragmatic guideline if they had one tuberculosis-related symptom including chronic cough, fever, night sweats, haemoptysis, weight loss, and loss of appetite. Chronic cough was defined as a continuous, non-remitting cough present for >3 weeks. Fever was defined as body temperature of >38°C for 14 days, after exclusion of common causes such as malaria or pneumonia. Weight loss was defined as reporting of weight loss or failure to thrive with confirmatory evidence from the child’s growth chart. Haemoptysis was defined as the expectoration of blood from the lung airways or parenchyma. Night sweats and loss of appetite were self-reported by children and parents. Asymptomatic contacts included children with cough of <3 weeks’ duration or fever of <2 weeks’ duration, or both. The difference between coprevalent tuberculosis among symptomatic and asymptomatic contacts was statistically different (23% vs 3%, p<0.0001). Contacts with tuberculosis infection (tuberculin skin-test induration ≥10 mm) did not result in increased risk for incident tuberculosis (among symptomatic contacts, 5% vs 5% incident tuberculosis rates among contacts infected and uninfected at baseline, p=0.80; among asymptomatic contacts, <1% vs <1% incident tuberculosis rates among contacts infected and uninfected at baseline, p=1.0)
