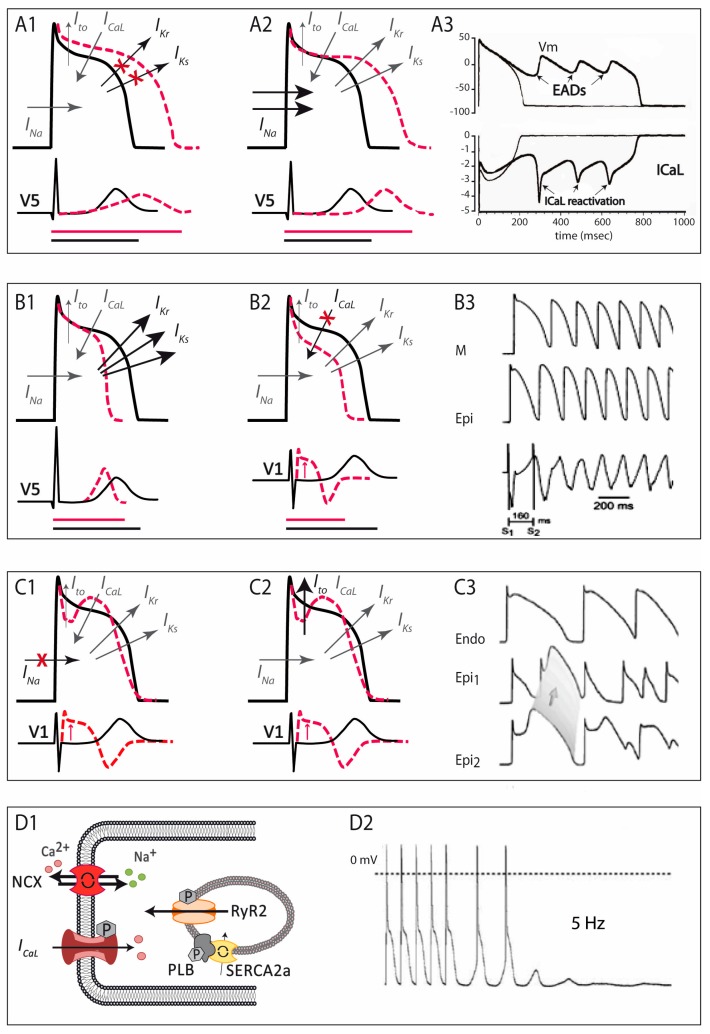
Figure 3.
Schematic representation of the pathophysiological mechanisms involved in the four main primary electrical disorders. (A) in LQTS, either by a decrease in K+ currents (A1) or an increase in Na+ currents (A2), AP duration is prolonged, and so is the QTc interval on the ECG (depicted by the bottom horizontal lines: in black normal QT, in red long-QT interval). This situation favors the development of early afterdepolarizations, the trigger of ventricular arrhythmias in LQTS patients (A3). (B) in SQTS, an increase in K+ currents accelerates repolarization (B1), and manifests as short QTc interval in the ECG (depicted by the bottom horizontal lines: in black normal QT, in red short-QT interval); in those cases of SQTS caused by loss-of-function mutations in the calcium channel (B2), besides shortening of the AP duration there is transmural gradient in early phases of repolarization, leading to ST-segment elevation like the one seen in BrS (combined phenotype, QT interval depicted by horizontal lines and ST segment elevation by the red arrow). In SQTS, an increased dispersion of repolarization favors the appearance of atrial and ventricular arrhythmias (B3). (C) In BrS, a decrease in Na+ currents (C1) or, less commonly, an increase in Ito currents (C2); produces a ionic imbalance in early repolarization, giving rise to the characteristic ST-segment elevation seen in the ECG (depicted by the red arrows). The consequent epicardial and transmural dispersion of repolarization favors ventricular arrhythmias by a mechanism of phase-2 reentry (C3). (D) CPVT is produced by abnormal Ca2+ leak from the sarcoplasmic reticulum (D1), which favors the occurrence of delayed afterdepolarizations, which in turn can trigger ventricular arrhythmias (D2). Modified from [6].