Abstract
Background
In 2011, 64% of children in Mozambique, ages 12–23 months, were fully immunized. Large provincial differences in vaccine uptake exist.
Methods
We conducted a survey of 1650 females with children aged 12–23 months in the districts of Gurùé and Milange. Implementation occurred from November to December 2014. Descriptive statistics and logistic regression using R-software 3.0.2 were used to examine factors associated with full vaccination status. ArcGIS version 10.3.1 (ESRI, Redlands, CA, USA) was used to map spatial patterns of vaccine uptake.
Results
Full vaccination was roughly 48%. Identifying ‘hospital’ as a location to get vaccinated was associated with having a fully vaccinated child (OR=1.87, 95% CI=1.02, 3.41, p=0.043). Households where health decisions are made solely by the male or the female had 38% (95% CI=0.32, 1.21) and 55% (95% CI=0.29, 0.69) lower odds, respectively, of their child being fully immunized. For every 10 km increase from the nearest health facility there was a 36% lower odds of the child being fully immunized (OR=0.64, 95% CI=0.44, 0.93, p<0.001).
Conclusion
Zambézia Province, as a whole and the districts of Gurùé and Milange specifically, is falling short of vaccination targets. Intensified efforts focused on the least educated, most distant and which take a more family-centered approach are needed to improve vaccine uptake.
Keywords: Immunization, Mozambique, Sub-Saharan Africa, Vaccination
Introduction
As 2015 came to an end, the global mobilization that marked the end of the Millennium Development Goals (MDG) had produced one of the most successful health and development movements in history.1 While the MDGs brought incredible advances globally, there is growing recognition that inequities persist and that the existing focus on national averages may actually have exacerbated regional and within country inequalities, particularly for child health.2,3 Addressing these inequalities with a focus that targets interventions at a more regional and local level may help to reduce the disparities in childhood mortality that remain in low and middle-income countries (LMIC) today.4,5
Providing available vaccines to all children remains one of the strongest and proven public health strategies to help achieve this goal. Major progress in vaccine coverage has been made in the last several decades and millions of lives have been saved globally thanks to vaccines.6,7 Nevertheless, challenges remain, given that in 2014 an estimated 19 million children worldwide still did not have access to basic required immunizations.8 In 2014, measles, neonatal tetanus, hemophilus influenza type b (Hib) and pertussis each caused between 60 000 and 200 000 childhood deaths, respectively. All of these deaths are considered preventable with proper vaccination.
In 2000, Global Alliance for Vaccine and Immunization (GAVI) and the WHO Africa Region set a target referred to as the ‘80/80 goal’. The objective was to reach ≥80% coverage for diphtheria-pertussis-tetanus (DPT-3) vaccination in every district in more than 80% of developing countries by 2005. From this target, the Reaching Every District (RED)/Reaching Every Child (REC) approach was designed in 2002.9 By 2005, WHO and UNICEF had developed the Global Immunization Vision and Strategy (GIVS) to strengthen national immunization programs, with the aim of reducing the morbidity and mortality of vaccine preventable diseases.10 Unlike other health interventions, vaccination is a cost-effective strategy that essentially guarantees a child´s protection against preventable disease.11–13 Distance to a healthcare facility, parental attitude, knowledge, perceived importance of vaccines, and family socioeconomic status are common barriers to achieving vaccine coverage.7,14
In Mozambique, a country that ranks 180 of 188 countries on the 2015 United Nations Development Program (UNDP) Human Development Index (HDI),15 the country's Expanded Program on Immunization (EPI) has been working with international partners to increase vaccine coverage. In 2011, a comprehensive multi-year plan for 2012–2016 was established to help meet national priorities. These priorities included increasing district level vaccine coverage for measles and the pentavalent DPT-Hep B-Hib vaccine to ≥80% for 85% of the districts, and increasing national coverage to 90%.16
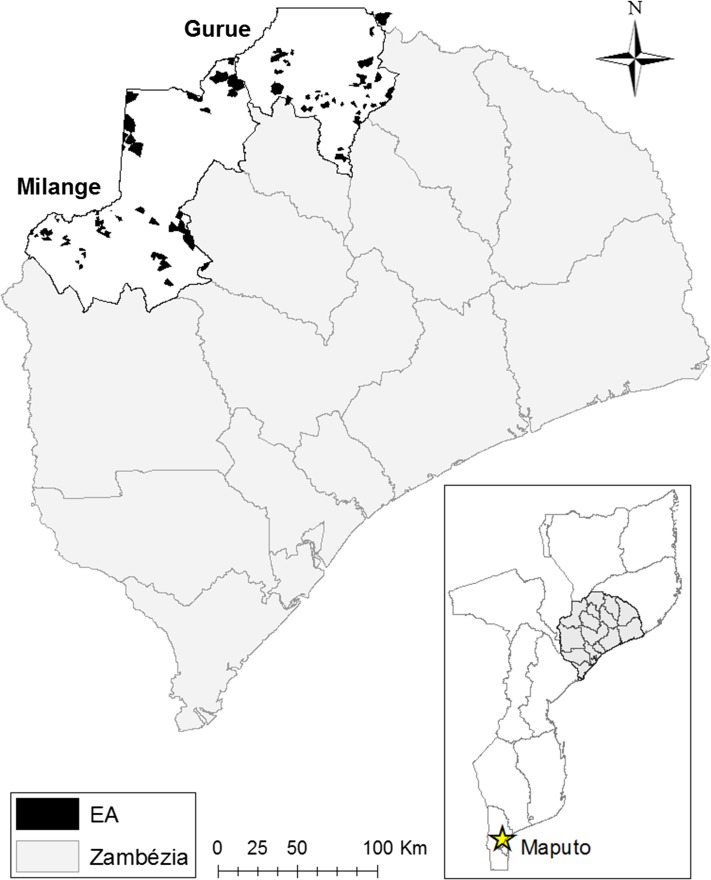
According to the 2011 Demographic Health Survey (DHS) for Mozambique, only 64% of children nationwide, aged 12–23 months, were fully immunized (defined as one dose of Bacillus Calmette–Guérin [BCG], three doses each of polio and DPT, and one dose of measles vaccine received before 1 year of age).17 Large provincial differences in vaccine uptake exist, with Maputo Province in the south, a province overly advantaged in terms of economics and resources, reporting >87% vaccine coverage; compared with Zambézia Province, an extremely rural and economically disadvantaged province in the country's central-north region, reporting only 47% vaccine coverage (Figure 1).
Figure 1.
Map of Zambézia Province with enumeration areas surveyed in the districts of Gurùé and Milange.
UNICEF is currently leading an initiative to support Mozambique's efforts to decrease inequity in access to immunization services through a UNICEF–GAVI agreement. In December 2013, UNICEF performed an equity analyses, which revealed that inequities are mostly geographically determined, and that Zambézia Province is home to the most deprived populations and has the lowest coverage rates of high impact health interventions, including immunization (unpublished data). Analyses performed with subnational data showed that 5 out of 17 districts in the province were disproportionately disadvantaged. Two of the most vulnerable districts identified, Milange and Gurùé, were chosen with the Mozambican Ministry of Health (MOH) and the Zambézia Provincial Health Directorate [Direcção Provincial de Saúde (DPS)] to receive intensified support as a proof of concept of the REC approach towards immunization coverage, combined with district planning. Other than the low coverage, they were selected for being both a long distance away from the provincial capital and for their respective population size. UNICEF has been supporting the MOH since 2014 to implement the REC approach in the districts of Gurùé and Milange. If the strategy proves to effectively increase immunization coverage, it will be scaled-up countrywide with the initial support of GAVI RSS funds recently allocated in the country.
In this study we report immunization specific cross-sectional survey data collected at baseline, in order to examine predictors of complete childhood immunization among children aged 12–23 months in the two districts of Zambézia Province—Gurùé and Milange. The results of this study provide relevant information for national policy and decision makers to adopt strategies that focus on the main barriers identified to immunization coverage.
Materials and methods
Sample design and data collection
A population-based household survey was carried out between 24 November and 17 December 2014. The sample was a stratified two-stage cluster, which utilized the 2007 Mozambique Population and Housing Census as a sampling frame. First, the sampling frame was stratified by district, then enumeration areas (EA) were randomly selected with probability proportional to size. Survey teams completed interviews in 110 enumeration areas (EA) across Gurùé (50 EA) and Milange (60 EA) districts (Figure 1). Households were selected by dividing the EA into quadrants, choosing a central point within each quadrant, spinning a bottle (or ink pen) to select a direction in which to proceed, and choosing the first household in this direction to serve as the starting point for interviewing the four nearest households. Constraints in the field required this altered approach, which does not employ the preferred method of household listing and random selection with equal probability. Household sampling probability was calculated by dividing the probability of EA selection by the number of households interviewed within the EA (typically 16). Child sampling probability was equal to household sampling probability divided by the number of eligible children aged 12–23 months. The survey instrument included over 500 questions related to standard socio-economic and health metrics, and was developed by a multi-disciplinary team of researchers from Vanderbilt University, UNICEF, and the University Eduardo Mondlane Faculty of Medicine in Maputo, Mozambique. Questions and scales deemed appropriate were adopted from previous national surveys in Mozambique and other international surveys such as the DHS and Multiple Indicator Cluster Survey (MICS). Only those questions relating to determinants of vaccine uptake were included in our analysis. The sampling design and implementation of this study are further detailed elsewhere: http://globalhealth.vanderbilt.edu/fgh/unicef-zambezia/.18
Four mobile teams, consisting of a team leader and four interviewers each, administered the survey face-to-face using mobile phones with an electronic questionnaire for data collection. From topographic maps, the survey teams divided the EAs into four quadrants. Starting in the center of the assigned quadrant, interviewers randomly selected a direction, then chose the first household in that direction (i.e. starting point), and systematically approached the nearest households for interview. Female interviewers conducted the survey with female heads-of-household, defined as the only or principal wife of the immediate family of the household. Only those households in which a child aged 12–23 months at the time the survey was conducted were included. If more than one child aged between 12 and 23 months lived in the household, data were collected for each of them. The female head-of-household was chosen as it was felt she was the most likely person to be familiar with the health and care taking of the entire family. In polygamous families, the eldest wife was selected. Interviewers were trained to conduct interviews in Portuguese or in one of the predominant local languages.
For this age group (12–23 months), full dosages of BCG, polio, DPT, Hepatitis B, HIB, PCV, and measles vaccinations were required in order to count a child as ‘fully immunized’. If any of the recommended doses could not be verified then the child was classified as ‘not fully immunized’.
Data analysis
Data obtained from the questionnaire were analyzed using R-software 3.0.2 (www.r-project.org). Descriptive statistics were calculated for continuous variables as weighted median with interquartile range (IQR) and for categorical variables as weighted percentages, with each observation being weighted by the inverse of the household (or child) sampling probability. Among those children with immunization cards presented to the surveyor, determinants of full vaccination status were modeled using multivariable logistic regression with robust covariance estimation to account for correlation of households from the same EA. Only including children with immunization cards meant higher confidence in the correct ascertainment of immunization status, but a 41% reduction in sample size. Data were collected on all children in the household. Covariates included district, reason for vaccinating children, family decision-maker, mode of travel, and distance to the nearest health facility. Distance to health facility was measured from the centroid of each EA. Missing values of covariates were multiply imputed to prevent case-wise deletion. If there was non-linearity (p<0.10), continuous variables were included in the model using restricted cubic splines.19 In the multivariable model, covariates were chosen a priori based on socio-demographic characteristics, which may represent one's health knowledge and health-seeking behavior.
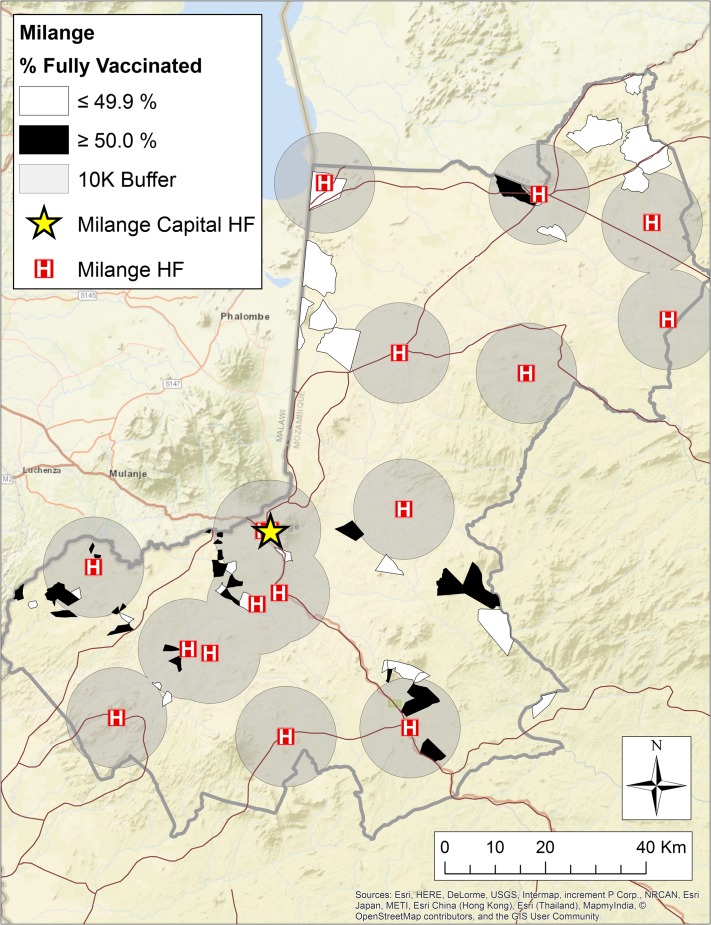
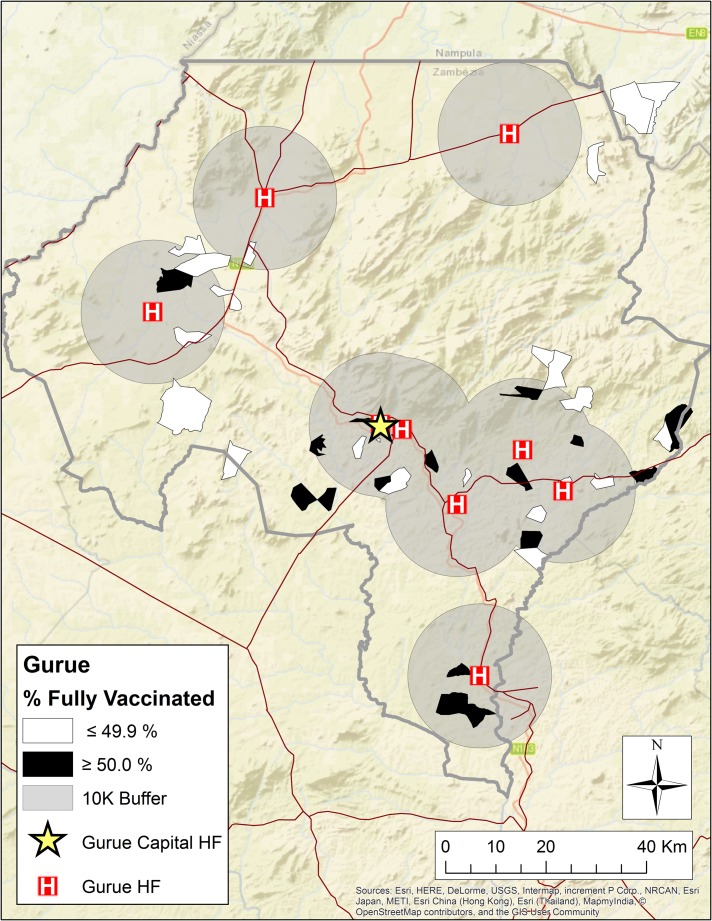
Geospatial mapping
ArcGIS version 10.3.1 (ESRI, Redlands, CA, USA) was used to map and visualize spatial patterns of vaccine uptake. Administrative boundaries and topographic data were obtained from DIVA-GIS Free Spatial Data (http://www.diva-gis.org/gdata) and ESRI (http://www.arcgis.com/home/item.html?id=30e5fe3149c34df1ba922e6f5bbf808f). Data were projected into Moznet UTM Zone 36S. The values representing each EA are the proportion of women in each EA who confirmed 100% vaccination completion for their child by showing a vaccination card. EAs are symbolized with less than or equal to 49.9% fully vaccinated (white) and greater than or equal to 50% fully vaccinated (black) (Figures 2 and 3).
Figure 2.
Map of Milange district, with EA and 10 km buffer around the health facility.
Figure 3.
Map of Gurùé District, with EA and 10 km buffer around the health facility.
Results
A total of 1650 female heads-of-household were surveyed. Of these, 1618 (98%) had sufficient data completed to be databased for analysis. Table 1 summarizes demographic information for the female heads-of-household. Differences were reported between Gurùé and Milange with respect to the proportion of women who understand Portuguese (57.7% versus 17.6%, respectively) and the proportion who reported living in a rural geographic area (60% versus 93%, respectively). Otherwise, no major differences were appreciated across districts in the proportions reported for age, marital status, education or other household characteristics.
Table 1.
Basic demographics: female head-of-household, baseline survey November–December 2014
| Gurùé | Milange | |
|---|---|---|
| (n=1618) | (n=754) | (n=864) |
| Age of respondent (years) | 26 (22–31) | 25 (21–30) |
| Marital status | ||
| Single | 3.0% | 8.2% |
| Married/Common Law | 91.4% | 86.8% |
| Widowed | 2.7% | 2.2% |
| Divorced/separated | 2.8% | 2.7% |
| Education category | ||
| None (0 years) | 41.3% | 39.4% |
| Some primary (1–6 years) | 46.1% | 51.7% |
| Primary completed (7 years) | 4.8% | 3.9% |
| Some secondary (8–11 years) | 5.0% | 4.7% |
| Secondary completed (12 years) | 2.4% | 0.3% |
| Superior (>12 years) | 0.4% | 0.1% |
| Household size | 4 (4–5) | 4 (3–5) |
| Number of children under 5 years | 1 (1–2) | 1 (1–2) |
| Respondent understands Portuguese | 57.7% | 17.6% |
| Ethnic group identity | ||
| Elomwe | 99.1% | 20.4% |
| Cinyanja | 0.0% | 82.1% |
| Religion | ||
| Catholic | 73.1% | 36.4% |
| Protestant | 11.8% | 29.2% |
| Evangelical and Pentecostal | 7.4% | 21.2% |
| Other Christian | 2.1% | 8.2% |
| Islam | 4.0% | 1.6% |
| Other | 1.6% | 2.8% |
| Length at residency (years) | 6 (5–10) | 6 (4–10) |
| Urban/rural | ||
| Rural | 60.0% | 93.7% |
| Urban | 40.0% | 6.3% |
| Household has electricity | 8.8% | 13.2% |
| Household has radio | 46.5% | 48.0% |
| Household has television | 8.1% | 5.4% |
| Respondent has mobile phone | 16.9% | 25.4% |
Continuous variables are reported as weighted estimates of median (interquartile range).
Categorical variables are reported as weighted percentages.
Percentages may not sum to 100%.
Immunization data were collected from 1675 children across the two districts (Table 2). Over half of respondents (63.4% in Gurùé and 55% Milange) had immunization cards that were presented to the interviewer for the child in question. Among children for whom an immunization card was presented, full immunization with BCG+polio+DPT+HepB+Hib+PCV+measles was 49.7% (95% CI=44.7, 54.7) in Gurùé and 48.0% (95% CI=40.5, 55.5) in Milange. It is important to point out that both PCV 10 and Hib began being offered in Zambézia in 2012. Hib is now most frequently offered as part of a pentavalent vaccine with DPT+HepB; however, in some cases, it was given as an independent stand-alone vaccine, resulting in the differences seen in percentage coverage between DPT+Hep B and Hib (Table 2).
Table 2.
Immunization of children age 12–23 months, UNICEF baseline survey 2014
| Gurue | Milange | |
|---|---|---|
| (n=761) | (n=914) | |
| Head of household presents an immunization card | 63.4% (56.2, 70.5) | 55.0% (48.2, 61.8) |
| Children with immunization cards | 277 | 270 |
| BCG immunization record | ||
| Dose 1 | 97.5% (95.8, 99.2) | 99.0% (98.2, 99.9) |
| Polio immunization record | ||
| Dose 1 | 97.2% (95.7, 98.7) | 97.0% (95.3, 98.6) |
| Dose 2 | 94.0% (91.7, 96.3) | 91.7% (88.3, 95.1) |
| Dose 3 | 92.1% (89.5, 94.7) | 89.7% (85.4, 94.0) |
| Dose 4 | 91.4% (88.9, 93.9) | 83.8% (78.8, 88.7) |
| DPT+HepB immunization record | ||
| Dose 1 | 91.9% (88.4, 95.3) | 83.5% (78.4, 88.5) |
| Dose 2 | 89.2% (85.2, 93.2) | 80.5% (75.0, 86.1) |
| Dose 3 | 85.3% (81.3, 89.4) | 78.2% (72.2, 84.1) |
| Measles immunization record | ||
| Dose 1 | 87.0% (82.8, 91.3) | 74.7% (68.1, 81.3) |
| PCV10 immunization record | ||
| Dose 1 | 66.8% (61.6, 71.9) | 71.4% (64.0, 78.7) |
| Dose 2 | 66.0% (60.9, 71.0) | 68.1% (60.5, 75.7) |
| Dose 3 | 63.1% (58.2, 68.0) | 66.0% (58.0, 74.1) |
| HIB immunization record | ||
| Dose 1 | 59.9% (54.7, 65.1) | 61.3% (52.6, 70.1) |
| Dose 2 | 58.1% (53.0, 63.1) | 57.9% (49.1, 66.7) |
| Dose 3 | 56.2% (51.2, 61.3) | 57.5% (48.7, 66.3) |
| Fully immunized from card | ||
| (BCG+polio+DPT+HepB+HIB+PCV10+measles) | 49.7% (44.7, 54.7) | 48.0% (40.5, 55.5) |
Categorical variables are reported as weighted percentages with 95% CIs that take into account the effect of clustering.
For this age group (12–23 months), full dosages of BCG, polio, DPT, hepatitis B, HIB, PCV and measles vaccine were required in order to count a child as fully immunized.
When we compare basic demographics of the female head-of-household by whether or not their child was fully immunized, both education level and knowledge of Portuguese language showed statistically significant differences. For years of education, female heads-of-household had a median of 3 years (IQR: 0–5) among respondents with a fully immunized child, compared to a median of 2 years (IQR: 0–4) of education for those with children not fully immunized (p<0.001). When disaggregated by education category, 43.8% of female heads with children not fully immunized had reported no education versus only 30.6% for those fully immunized (p<0.001). A higher proportion of children were fully immunized if their female head-of-household reported understanding Portuguese (36.7% versus 25.8%; p<0.001). In relation to household assets, a statistically significant greater proportion of fully immunized children came from households with electricity (17.2% versus 9.8%; p=0.004), radio ownership (55.1% versus 44.4%; p<0.001), television ownership (11.0% versus 4.2%; p<0.001) and mobile phone ownership (31.1% versus 19.6%; p<0.001). No difference was seen for marital status, household size, ethnic group, religion or urban versus rural residence (Table 3).
Table 3.
Basic demographics: female head-of-household by child´s vaccination status
| Not fully vaccinated | Full vaccination | p-value | |
|---|---|---|---|
| (n=1143) | (n=475) | ||
| Age of respondent | 26 (22–30) | 25 (21–30) | 0.038 |
| Age category | 0.023 | ||
| Missing, n(%) | 129 (11.3%) | 24 (5.1%) | |
| 15–19 years | 9.4% | 14.9% | |
| 20–24 years | 30.6% | 31.9% | |
| 25–29 years | 30.0% | 27.0% | |
| 30–34 years | 14.5% | 16.0% | |
| 35–39 years | 13.9% | 7.4% | |
| 40–44 years | 1.3% | 1.7% | |
| >44 years | 0.3% | 1.0% | |
| Marital status | NS | ||
| Single | 6.0% | 8.6% | |
| Married/common law | 88.3% | 87.7% | |
| Divorced/separated | 3.0% | 2.0% | |
| Widowed | 2.6% | 1.7% | |
| Years of education | 2 (0–4) | 3 (0–5) | <0.001 |
| Education category | <0.001 | ||
| None (0 years) | 43.8% | 30.6% | |
| Some primary (1–6 years) | 49.3% | 52.1% | |
| Primary completed (7 years) | 3.3% | 6.0% | |
| Some secondary (8–11 years) | 2.7% | 9.8% | |
| Secondary completed (12 years) | 0.8% | 1.1% | |
| Superior (>12 years) | 0.1% | 0.4% | |
| Household size | 4 (3–5) | 4 (3–5) | NS |
| Respondent understands Portuguese | 25.8% | 36.7% | <0.001 |
| Ethnic group identity | |||
| Elomwe | 43.6% | 40.2% | NS |
| Cinyanja | 58.9% | 59.1% | NS |
| Religion | |||
| Catholic | 45.5% | 49.5% | |
| Protestant | 23.3% | 26.6% | |
| Evangelical and Pentecostal | 19.0% | 13.1% | |
| Other Christian | 7.1% | 5.1% | |
| Islam | 1.6% | 4.1% | |
| Other | 2.9% | 1.4% | |
| Urban/rural | NS | ||
| Rural | 86.2% | 79.3% | |
| Urban | 13.8% | 20.7% | |
| Household has electricity | 9.8% | 17.2% | 0.004 |
| Household has radio | 44.4% | 55.1% | <0.001 |
| Household has television | 4.2% | 11.0% | <0.001 |
| Respondent has mobile phone | 19.6% | 31.1% | <0.001 |
| EA distance to health facility (km), median (IQR) | 9.9 (6.4–13.2) | 8.7 (5.2–10.8) | <0.001 |
| EA distance to health facility (km) | <0.001 | ||
| <10 km | 50.7% | 64.5% | |
| 10 km or more | 49.3% | 35.5% |
Continuous variables are reported as weighted estimates of median (interquartile range), with each observation being weighted by the inverse of the household sampling probability.
Catergorical variables are reported as weighted percentages, with each observation being weighted by the inverse of the household sampling probability.
Percentages may not sum to 100%.
NS: values that were not significant at a p<0.05.
Factors independently associated with full-vaccination were assessed using multivariable logistic regression (Table 4). For female heads-of-household, the factors associated with having a fully immunized child included their knowledge about where to seek immunization, shared responsibility with a male caregiver about healthcare decisions for the child, and distance to the health facility. Compared with households in which the male and female caregiver shared decision-making responsibility for the child´s healthcare, households in which the woman was the sole decision maker had a 55% lower odds of their child being fully immunized (OR=0.45, 95% CI=0.29, 0.69).
Table 4.
Determinants of full vaccination using multivariate logistic regression
| Odds Ratio (95%CI) | p-value | |
|---|---|---|
| District | NS | |
| Milange (ref) | 1 | |
| Gurùé | 0.85 (0.57, 1.28) | |
| Reason for vaccinating children | 0.002 | |
| Protect children against illness (ref) | 1 | |
| Heal them | 0.54 (0.31, 0.94) | |
| Help them grow healthy | 1.32 (0.93, 1.87) | |
| Hospital identified as location for vaccination | 1.87 (1.02, 3.41) | 0.043 |
| Health facility identified as location for vaccination | 0.55 (0.37, 0.81) | 0.003 |
| School identified as location for vaccination | 0.42 (0.24, 0.73) | 0.002 |
| Mobile brigade identified as location for vaccination | 1.19 (0.82, 1.73) | NS |
| Household has radio | 1.20 (0.89, 1.61) | NS |
| Decision maker for health care of children | <0.001 | |
| Both (ref) | 1 | |
| Men | 0.62 (0.32, 1.21) | |
| Women | 0.45 (0.29, 0.69) | |
| Distance to nearest health facility (per 10 km increase) | 0.64 (0.44, 0.93) | 0.019 |
| Mode of travel to nearest health facility | NS | |
| On foot (ref) | 1 | |
| Bicycle | 0.82 (0.58, 1.15) | |
| Motorcycle | 0.79 (0.30, 2.06) | |
| Car | 2.48 (0.94, 6.53) | |
| Ever visited a government health facility for health problem | 1.24 (0.81, 1.87) | NS |
| Ever visited a traditional healer for health problems | 0.66 (0.42, 1.03) | NS |
NS: values that were non-significant at a p≤0.05.
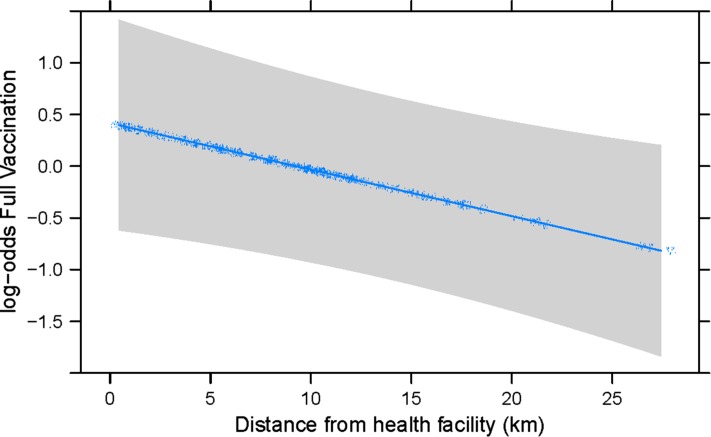
When we analyzed full vaccination status by distance, we found that a statistically significant greater proportion of children who lived within 10 km of a health facility were fully vaccinated (64.5% versus 50.7%; p<0.001). Figures 2 and 3 show the location of health facilities per district in relation to EAs surveyed, with a buffer of 10 km denoted around each health facility. EAs with ≥50% of children showing full vaccination by immunization card are represented in black and EAs with ≤49.9% of children showing full vaccination represented in white. Of children reporting full vaccination, the median distance to a health facility was 8.7 km (IQR: 5.2–10.8 km) compared to 9.9 km (IQR: 6.4–13.2 km) for children not fully vaccinated (p<0.001) (Table 3). Using multivariable logistic regression, for every 10 km increase from the nearest health facility (linear association, Figure 4) there is a 36% lower odds that one´s child will be fully vaccinated (OR=0.64, 95% CI=0.44, 0.93, p<0.001) (Table 4).
Figure 4.
Log-odds of full vaccination status by distance (in km) of the enumeration areas (EA) to the nearest health facility.
Discussion
Overall, full vaccination status, at baseline, in children aged 12–23 months in the districts of Gurùé and Milange was low (49.7% and 48%, respectively). This proportion is relatively unchanged from the 2011 provincial estimates for children of a similar age (47.3%) and considerably lower than the national estimate of 64%, as reported in the 2011 DHS.17 Our baseline study evaluated the factors associated with full vaccination status and found higher maternal education; head-of-household understanding Portuguese; identification of hospital as a place to receive immunization; and shorter distance to a health facility to be positively associated with full vaccination status.
In our study, a statistically significant higher proportion of children fully vaccinated had a female head-of household reporting at least some primary education (69.4% versus 56.2%). This is consistent with other studies in sub-Saharan Africa in which higher maternal education was associated with a roughly two fold higher likelihood of a child being fully vaccinated.7,20–24 In addition, a statistically significant higher proportion of children fully vaccinated came from households in which the female head-of-household reported understanding Portuguese. This is not surprising given our finding of a positive association with higher maternal education. Portuguese is the official language in Mozambique and in our experience the language most frequently used by healthcare workers. However, for a patient to speak Portuguese in rural Mozambique, it is likely that they received some schooling in order to have enough exposure to learn the language, as the local languages are more commonly spoken. This discrepancy in language between health facilities and communities could further contribute to lack of immunization.
Prior studies have shown that improving a caregiver´s health literacy and knowledge about the benefits of vaccination were associated with an overall increase in full vaccination coverage.7,25 Information about vaccination is inherently complex. Patients and caregivers need to understand about the disease itself, risk of contracting a disease, risks to receiving the vaccination, and potential risks of vaccine failure.25 However, simple steps can be taken to make sure information disseminated about vaccination is easier to understand and use. Alternative formats for information dissemination such as longer consultation times with a health provider or techniques, such as ‘teach-back’, which check to see that information is successfully conveyed and received, and can be used.25
We found a higher likelihood of a child being fully vaccinated in households with shared healthcare decision-making as compared with households in which healthcare decisions were made by either the male or female alone. Families represent an essential and lifelong support system for children, and the high value African families place on children plays a large role in identifying their care needs and providing for their basic necessities.26 Recently, strategies aimed at increasing male engagement in antenatal care in Zambézia Province showed success in increasing HIV testing and uptake of antiretroviral therapy for HIV positive pregnant women when their male partner was an active participant in care.27 Similarly, initiatives that ensure that support garnered for children is directed at the family unit are becoming more widespread.28 Future initiatives aimed at improving vaccine uptake could learn from the successes of these initiatives and develop a more family-centered approach.
The Mozambican Ministry of Health estimates that 60% of the population lives 30 km or farther from any health facility.29 The necessity to travel long distances to a healthcare facility is a barrier in healthcare utilization and is associated with increased child mortality.30 In our study, longer distances to a health facility was associated with a decreased likelihood of one´s child being fully vaccinated, which is consistent with a previous study in the Magude district of southern Mozambique.14 We found that access to a car, as the mode of transport to a health facility, increased by over two fold the likelihood of one´s child being fully vaccinated, although it was not statistically significant. As such, interventions aimed at increasing the availability of transportation or assistance with covering the costs of transportation could be beneficial for increasing overall vaccine coverage.
Strengths of this study include a large sample of district-focussed data as opposed to countrywide data. Predictors of full vaccination were similar across districts. Survey interviewers were Zambézia Province residents that conducted the survey in the predominant local languages of Gurùé and Milange. The models in the analysis were developed a priori and tested non-linearity of covariates with restricted cubic splines. The survey was designed to collect information about the household from the female head-of-household, defined as the principal wife of the nuclear (immediate) family. The female head-of-household was selected to be the interviewee, because she is thought to be the person most familiar with the health and caretaking of all household members. However, we recognize that a limitation of our study is the fact that potential bias could have been introduced by the fact that no interviews were conducted with males. This is especially true for questions such as ‘who the decision maker is for healthcare of the children.’ Other limitations include our decision to exclude self-reported immunization data from heads-of household that could not show their child´s immunization card for analysis. Another limitation is that households were not selected within EA using household listing and equal probability, but instead we used a quadrant-based approach which is not ideal for outcomes that tend to be clustered (like immunization). In such cases, many female heads-of-household could not identify by name the immunizations received. As such, estimates may represent an under estimation of true immunization coverage. Finally, this survey was implemented in two distinct rural districts of Zambézia Province and, as such, may not be generalizable to other districts in Zambézia Province or other Provinces within Mozambique.
Conclusions
Great strides have recently been taken to combat under-five mortality and in reaching international targets defined by the MDGs. Despite this, regional and within-country inequalities exist. Zambézia Province as a whole and the districts of Gurùé and Milange specifically, are falling short in relation to targets for complete vaccination uptake. Intensified efforts focussed on the least educated, most distant from a health facility, and taking a more family centered approach are needed to improve vaccine uptake.
Acknowledgments
Authors’ contributions: SS, MB, LG, MR, AB, SM, CC, AG and TM were involved in the design of the study, interpretation of findings, drafting and revising the manuscript. SS, TM and MB participated in performing statistical analysis. LG, MB, SM, AG and TM participated in data acquisition. CC created the maps. All authors read and approved the final manuscript. TM and AB are guarantors of the paper.
Acknowledgments: We acknowledge Ezequiel Barreto Ossemane and Damasceno Lopes of the Friends in Global Health HIS team, who provided assistance with uploading questionnaires into the mobile phones, and provided back-up and trouble-shooting support during survey implementation. We would like to acknowledge Eva Millas of UNICEF for her support of the Reaching Every Community (REC) project in Zambézia Province. Additionally, we thank the hard work of our local interviewers; without their dedication and support this survey could not have been completed.
Funding: This work was supported by UNICEF [VIGH-PCA2014/08].
Competing interests: None declared.
Ethical approval: This study was approved by the Inter-institutional Bioethics Committee for Health of Zambézia Province (Comité Inter-Institucional de Bioética para Saúde de Zambézia), and the Vanderbilt Institutional Review Board. Each female head-of-household voluntarily provided informed verbal and written consent before participating in the study.
Availability of data and materials: The authors have permission from UNICEF to publish the data. The design and implementation of this study are detailed in the text. In order to access the data, kindly request permission from the corresponding author at troy.moon@vanderbilt.edu
References
- 1. United Nations The Millennium Development Goals Report 2015. New York: United Nations, 2015:1–71. [Google Scholar]
- 2. UN System Task Team on The Post-2015 UN Development Agenda: the Heart UN Development Agenda Addressing inequalities: the heart of the post-2015 agenda and the future we want for all. New York: United Nations; 2012. [Google Scholar]
- 3.Health and the post-2015 development agenda. Lancet 2013;381:699. [DOI] [PubMed]
- 4. Gandhi G. Charting the evolution of approaches employed by the Global Alliance for Vaccines and Immunizations (GAVI) to address inequities in access to immunization: a systematic qualitative review of GAVI policies, strategies and resource allocation mechanisms through an equity lens (1999–2014). BMC Publ Health 2015;15:1198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Carrera C, Azrack A, Begkoyian G, et al. . The comparative cost-effectiveness of an equity-focused approach to child survival, health, and nutrition: a modelling approach. Lancet 2012;380:1341–51. [DOI] [PubMed] [Google Scholar]
- 6. Ryman TK, Dietz V, Cairns KL. Too little but not too late: results of a literature review to improve routine immunization programs in developing countries. BMC Health Serv Res 2008;8:134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Legesse E, Dechasa W. An assessment of child immunization coverage and its determinants in Sinana District, Southeast Ethiopia. BMC Pediatr 2015;15:31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.The Vaccine Alliance Progress Report 2014. Available from: http://www.gavi.org/progress-report/ [accessed 1 March 2017].
- 9. Vandelaer J, Bilous J, Nshimirimana D. Reaching Every District (RED) approach: a way to improve immunization performance. Bull World Health Org 2008;86:A–B. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Global Immunization Vision and Strategy 2006–2015. Geneva: World Health Organization, 2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Bhutta ZA, Chopra M, Axelson H, et al. . Countdown to 2015 decade report (2000–10): taking stock of maternal, newborn, and child survival. Lancet 2010;375:2032–44. [DOI] [PubMed] [Google Scholar]
- 12. Mulholland EK, Griffiths UK, Biellik R. Measles in the 21st century. N Engl J Med 2012;366:1755–7. [DOI] [PubMed] [Google Scholar]
- 13. Lanaspa M, Balcells R, Sacoor C, et al. . The performance of the expanded programme on immunization in a rural area of Mozambique. Acta Trop 2015;149:262–6. [DOI] [PubMed] [Google Scholar]
- 14. Jani JV, De Schacht C, Jani IV, et al. . Risk factors for incomplete vaccination and missed opportunity for immunization in rural Mozambique. BMC Public Health 2008;8:161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.United Nations Development Programme, Human Development Reports. Available from: http://hdr.undp.org/en/countries/profiles/MOZ [accessed 11 January 2017].
- 16.Mozambique Findings from the 2015 Gavi Full Country Evaluation. Available from: http://www.gavi.org/country/mozambique/ [accessed 11 January 2017].
- 17.Moçambique Inquérito Demográfico e de Saúde 2011. Available from: http://dhsprogram.com/pubs/pdf/FR266/FR266.pdf [accessed 11 January 2017].
- 18.UNICEF Zambézia Equity Priority District Survey. Available from: http://globalhealth.vanderbilt.edu/fgh/unicef-zambezia/ [accessed 11 January 2017].
- 19. Harrell F. Regression modeling strategies: with applications to linear models, logistic and ordinal regression, and survival analysis. New York: Springer, 2015. [Google Scholar]
- 20. Odusanya OO, Alufohai EF, Meurice FP, et al. . Determinants of vaccination coverage in rural Nigeria. BMC Publ Health 2008;8:381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Le Polain de Waroux O, Schellenberg JRA, Manzi F, et al. . Timeliness and completeness of vaccination and risk factors for low and late vaccine uptake in young children living in rural southern Tanzania. Int Health 2013;5:139–47. [DOI] [PubMed] [Google Scholar]
- 22. Oliveira MFS de, Martinez EZ, Rocha JSY.. Factors associated with vaccination coverage in children <5 years in Angola. Rev Saúde Pública 2014;48:906–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Ratzan SC. Vaccine literacy: a new shot for advancing health. J Health Commun 2011;16:227–9. [DOI] [PubMed] [Google Scholar]
- 24. Castro-Sánchez E, Chang PWS, Vila-Candel R, et al. . Health literacy and infectious diseases: why does it matter. Int J Infect Dis 2016;43:103–10. [DOI] [PubMed] [Google Scholar]
- 25. Rowlands G. Health literacy. Hum Vaccines Immunother 2014;10:2130–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Achema G, Ncama BP. Exploring family-centered care for children living with HIV and AIDS in Nigeria. Jpn J Nurs Sci 2016;13:256–64. [DOI] [PubMed] [Google Scholar]
- 27. Audet CM, Blevins M, Chire YM, et al. . Engagement of men in antenatal care services: increased HIV testing and treatment uptake in a community participatory action program in Mozambique. AIDS Behav 2016, Sep;20(9):2090–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Richter LM, Sherr L, Adato M, et al. . Strengthening families to support children affected by HIV and AIDS. AIDS Care 2009;21:3–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Nhampossa T, Mandomando I, Acacio S, et al. . Health care utilization and attitudes survey in cases of moderate-to-severe diarrhea among children ages 0–59 months in the District of Manhica, southern Mozambique. Am J Trop Med Hyg 2013;89:41–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Van den Broeck J, Eeckels R, Massa G. Maternal determinants of child survival in a rural African community. Int J Epidemiol 1996;25:998–1004. [DOI] [PubMed] [Google Scholar]