Abstract
Background
Previous research found poverty to be associated with adverse health outcomes among older adults but the factors that translate low economic resources into poor physical health are not well understood. The goal of this analysis was to assess the impact of material, psychosocial, and behavioural factors as well as education in explaining the poverty-health link.
Methods
In total, 28 360 observations from 11 390 community-dwelling respondents (65+) in the Survey of Health, Ageing and Retirement in Europe (2004–13, 10 countries) were analysed. Multilevel growth curve models were used to assess the impact of combined income and asset poverty risk on old-age frailty (frailty index) and associated pathway variables.
Results
In total, 61.8% of the variation of poverty risk on frailty level was explained by direct and indirect effects. Results stress the role of material and particularly psychosocial factors such as perceived control and social isolation, whereas the role of health behaviour was negligible.
Conclusion
We suggest to strengthen social policy and public health efforts in order to fight poverty and its deleterious health effects from early age on as well as to broaden the scope of interventions with regard to psychosocial factors.
Introduction
Many studies have focussed on health inequalities among older adults with regard to socio-economic status (SES) operationalized by education, occupation and/or income. Fewer studies have focussed on poverty—i.e. economic resources ‘so serious below those commanded by the average individual or family that [the poor] are, in effect, excluded from ordinary living patterns, customs and activities’1 (p. 31)]—and its significant detrimental effect on physical health and functioning in old age.2–11 More crucially, the obvious follow-up question as to ‘why’ poor older adults have poorer health than their economically better-off counterparts has received even less attention. Whereas research attempting to explain the SES-health link by assessing material, psychosocial and behavioural factors has accumulated over the last years,12–17 analogous evidence on the poverty-health link remains scattered and partial. Existing studies18–23 emphasize the role of adverse childhood circumstances, lower educational achievement, higher environmental risk exposure, higher stress levels and, particularly, more harmful health behaviours as specific explanatory factors for the poverty-health link. However, these studies mostly focussed on single pathway factors—particularly on behavioural factors such as smoking or exercising—and in turn, did not account for mutual confounding respectively direct and indirect contributions of material, psychosocial and behavioural factors. Furthermore, the widespread reliance on cross-sectional data from single countries, provinces, or cities in these studies18–23 limits the generalizability of the results and hinders the identification of causal relationships. More robust cross-national and longitudinal evidence on the topic is lacking. Last but not least, poverty risk (PR) is most often operationalized solely as low income which ignores the role of other economic resources such as real and financial assets which are particularly relevant for old-age health and well-being.11,24
Against the backdrop of these shortcomings, the purpose of this article was (i) to assess the impact of combined income and asset PR on frailty—a comprehensive measure of health in old age—and (ii) to assess a broad range of material, psychosocial and behavioural pathway variables in order to explain the poverty-health link among older adults in 10 European countries.
Methods
Data
The Survey of Health, Ageing and Retirement in Europe (SHARE) provides representative data of individuals (50+) in residential households. SHARE currently features five waves, four of which (1, 2, 4, 5) provide panel data from 10 countries (Austria, Belgium, Denmark, France, Germany, Italy, Netherlands, Spain, Sweden, Switzerland) over a 10-year period (2004–13), whereas the third wave conducted retrospective interviews on life histories. Information is obtained through personal interviews, complemented by self-completion questionnaires. The target population of the first wave was born before 1954, and the overall response rate was 61.8%. Out of the 11 390 respondents (65+) in wave 1 (2004/05), 7390 (64.9%), 5174 (45.4%) and 4406 (38.7%) participated in the second (2006/07), the fourth (2010/11) and the fifth (2013) wave, respectively, which amounted to a total of 28 360 observations (2.49 observations per person on average).
Variables
Frailty index
The frailty index (FI), a cumulative measure of health deficits25–27 was computed based on 39 items available in all four waves of SHARE, including self-reported health, diagnosed illnesses, activities of daily living, sensory impairment, body mass index deficit, and grip strength (Supplementary Table S1). The FI (range = 0–1) was calculated by dividing the sum score by the number of deficit items.
Poverty risk
We identified older adults to be at PR based on the co-occurrence of low household income and limited wealth at least once during the assessment period. Income PR was defined as <60% of the national median net household income,28 including all regular sources of income (pensions, social transfers, employment, rent). Asset PR was defined as belonging to the lowest quintile regarding country-specific household net wealth, which included real (real estate, car(s) and business shares minus mortgages) and financial assets (bank accounts, bonds/stocks/funds, long-term investments minus financial liabilities).
Socio-demographic/time variables
These variables included: (i) age (in years), (ii) birth cohort (before 1926/1926–30/1931–35/1936–40), (iii) sex (male/female), (iv) non-response in at least one subsequent wave of SHARE (no/yes) and (v) death of the respondent between 2004 and 2013 (no/yes).
Education
Education was measured using the International Standard Classification of Education (ISCED-97): primary (0–1), lower secondary (2), upper secondary (3) and post-secondary/tertiary (4–6) education.
Material factors
These factors included (i) severe financial problems, i.e. great difficulties to make ends meet (no/yes), (ii) low-quality accommodation (due to one of the following items): no indoor bathroom or indoor toilet, insufficient heating/cooling (no/yes), (iii) neighbourhood problems (due to one of the following items): insufficient access to facilities, lack of public transport, pollution/noise or vandalism/crime (no/yes), and lack of access to health care services, i.e. health care utilization forgone due to (iv) non-availability (no/yes) or (v) non-affordability (no/yes).
Psychosocial factors
These factors included measures of social isolation: (i) living with a partner (yes/no), (ii) feeling often lonely (no/yes) and (iii) social participation, measured by engagement in community activities (through one of the following items): voluntary work, educational training, membership in a club or in a religious or political organization (yes/no). Furthermore, we included (iv) occupational social prestige measured by the International Occupational Prestige Score (SIOPS, 13–78) based on household-level ISCO codes and (v) perceived control (3–12; α = 0.69–0.70) and (vi) hedonic well-being (3–12, α = 0.63–0.69), two sum scores, each based on three items from the CASP-12 scale.29
Behavioural factors
These factors included: (i) heavy smoking, i.e. >30 pack-years (no/yes), (ii) daily/almost daily alcohol consumption (no/yes) and (iii) regular sport/physical activities, i.e. more than once a week (yes/no).
Missing data
Missing values were negligible, except for a number of predictor variables from the drop-off module, a self-completion paper and pencil questionnaire handed out after completion of the computer-assisted main interviews. In total, 64.9% of the respondents (65+) who completed the main interview also filled in said drop-off questionnaire. Consequently, there were considerable rates of missing data in the concerned predictor variables (Supplementary Table S2). These were considered mostly missing at random (MAR), since their missingness was arguably not due to the nature of the required information itself but rather due to the interview mode used to collect them30 or sociodemographic attributes,31 and thus observable variables. Against this backdrop, we applied a multiple-imputation procedure, using R-package ‘mice’ resulting in 50 complete datasets, the results of which were pooled according to Rubin’s rule. In order to approximate MAR, we utilized all predictor variables and a number of additional auxiliary variables32 such as interviewer ratings of the respondent’s willingness to answer or their ability to understand questions (Supplementary Table S2), which were used to predict missing values.
Model
Frailty trajectories were assessed using growth curve models (R-package lme4 (v1.1-12) based on hierarchical linear modelling33 with three levels: up to four measurements were nested within individuals, which were in turn nested within countries. Growth curve models using age as time metric provided estimates of the impact of PR on frailty levels at grand-mean-centred age (76.8 years) and regarding change over time (5-year intervals) while controlling for birth cohort. A quadratic growth model for FI was found to provide the best statistical fit, and was thus used for all analyses. We estimated main effects for all predictors and interaction terms with time for PR in order to assess potential changes in impact as people age, and for sex since frailty trajectories are known to vary between women and men.
The first conditional multilevel growth curve model included PR only. Models II (education), III (material), IV (psychosocial) and V (behavioural) each added one set of factors, respectively. To analyse the mechanisms translating PR into frailty, we computed the raw percentage reduction of the effect size () of PR after inclusion of the subsequent factors. In a second step, independent contributions of each set of variables (x), e.g. behavioural, regarding the explanation of the impact of PR on frailty were calculated as the percentage reduction in the effect size of PR in the full model (model VI) minus the reduction in a model with all factors except factor x. Overlap was calculated by subtracting the independent contributions from the total reduction of the impact of PR in the full model.13,14,16
Results
Main analysis
In the total sample, FI values ranged from 0 to 0.92 and showed the expected distribution (mean = 0.18, median = 0.14, 95th/99th percentile = 0.47/0.64). At baseline (2004/05), 18.8 and 20.0% of the respondents were classified as being at risk of income or asset poverty, while only 6.1% were both. In total 25% of the income-poor older adults were at the same time found in the two highest wealth quintiles. Between 2004 and 2013, 1,574 (13.8%) of the respondents were at risk of both income and asset poverty at least once. Table 1 shows the sample characteristics as well as associations of predictor variables with PR and FI. Most potential pathway variables showed the expected bivariate association with PR.
Table 1.
Sample characteristics and bivariate analysis
| Sample characteristics | At PR | FI (mean w1–w5) | |||
|---|---|---|---|---|---|
| n | %/mean (SD) | No %/mean (SD) | Yes %/mean (SD) | mean/Pearson r | |
| PR | |||||
| At PR | |||||
| No | 9816 | 86.2 | – | – | 0.17 |
| Yes | 1574 | 13.8 | – | – | 0.23 |
| Demographics/sample attrition | |||||
| Sex | |||||
| Male | 5152 | 45.2 | 47.9 | 28.6 | 0.16 |
| Female | 6238 | 54.8 | 52.1 | 71.4 | 0.20 |
| Age (in years, 65–103)a | 11 390 | 73.9 (6.8) | 73.7 (6.7) | 75.4 (7.2) | 0.40 |
| Birth cohort | |||||
| Before 1926 | 2745 | 24.1 | 23.0 | 31.3 | 0.26 |
| 1926–30 | 2433 | 21.4 | 21.0 | 23.8 | 0.19 |
| 1931–35 | 3125 | 27.4 | 27.9 | 24.8 | 0.15 |
| 1936–40 | 3087 | 27.1 | 28.2 | 20.1 | 0.13 |
| Non-response (at least once after w1) | |||||
| No | 5164 | 45.4 | 43.7 | 55.3 | 0.20 |
| Yes | 6,26 | 55.7 | 56.3 | 44.7 | 0.17 |
| Death (between waves 1–5) | |||||
| No | 9284 | 81.6 | 85.4 | 84.9 | 0.17 |
| Yes | 2095 | 18.4 | 14.6 | 15.1 | 0.27 |
| Education | |||||
| ISCED 0–1 | 5024 | 44.6 | 41.9 | 61.2 | 0.22 |
| ISCED 2 | 2022 | 17.9 | 17.8 | 18.9 | 0.17 |
| ISCED 3 | 2513 | 22.3 | 23.6 | 14.0 | 0.15 |
| ISCED 4–6 | 1709 | 15.2 | 16.7 | 5.9 | 0.13 |
| Material factors | |||||
| Great difficulties making ends meeta | |||||
| No | 10 425 | 91.6 | 93.1 | 82.0 | 0.17 |
| Yes | 957 | 8.4 | 6.9 | 18.0 | 0.25 |
| Low-quality accommodation | |||||
| No | 6398 | 86.5 | 87.1 | 83.1 | 0.16 |
| Yes | 995 | 13.5 | 12.9 | 16.9 | 0.21 |
| Neighbourhood problems | |||||
| No | 5744 | 81.5 | 87.1 | 83.1 | 0.16 |
| Yes | 1306 | 18.5 | 12.9 | 16.9 | 0.21 |
| Forgone health care due to non-availability | |||||
| No | 11 128 | 98.4 | 98.4 | 98.0 | 0.18 |
| Yes | 186 | 1.6 | 1.6 | 2.0 | 0.26 |
| Forgone health care due to non-affordability | |||||
| No | 10 937 | 96.7 | 97.0 | 94.5 | 0.18 |
| Yes | 374 | 3.3 | 3.0 | 5.5 | 0.27 |
| Psychosocial factors | |||||
| Partnera | |||||
| Yes | 7441 | 65.3 | 69.6 | 38.5 | 0.16 |
| No | 3949 | 34.7 | 30.4 | 61.5 | 0.22 |
| Often lonely | |||||
| No | 6297 | 89.2 | 90.2 | 82.9 | 0.16 |
| Yes | 764 | 10.9 | 9.8 | 17.1 | 0.24 |
| Social participationa | |||||
| Yes | 3585 | 32.1 | 32.8 | 27.5 | 0.14 |
| No | 7583 | 67.9 | 67.2 | 72.5 | 0.20 |
| Social prestige (13–78) | 10 385 | 39.8 (13.5) | 40.5 (13.6) | 35.2 (11.6) | −0.17 |
| Perceived control (3–12)a | 6922 | 8.5 (2.2) | 8.5 (2.2) | 8.0 (2.2) | −0.46 |
| Subjective well-being (3–12)a | 6992 | 10.4 (1.9) | 10.4 (1.8) | 10.2 (1.9) | −0.26 |
| Behavioural factors | |||||
| History of heavy smoking | |||||
| No | 9750 | 85.6 | 85.4 | 87.2 | 0.18 |
| Yes | 1640 | 14.4 | 14.6 | 12.8 | 0.18 |
| Frequent alcohol consumptiona | |||||
| No | 8493 | 75.0 | 73.5 | 83.8 | 0.19 |
| Yes | 2836 | 25.0 | 26.5 | 16.2 | 0.16 |
| Sport/physical activity (>once a week)a | |||||
| Yes | 8418 | 74.3 | 26.9 | 18.3 | 0.12 |
| No | 2915 | 25.7 | 73.1 | 81.7 | 0.20 |
Notes: SHARE waves 1,2,4,5 (release 5.0.0), w1, wave 1; w5, wave 5; SD, standard deviation; ISCED, International Classification of Education.
Time-varying variable: values refer to the first wave (2004/05).
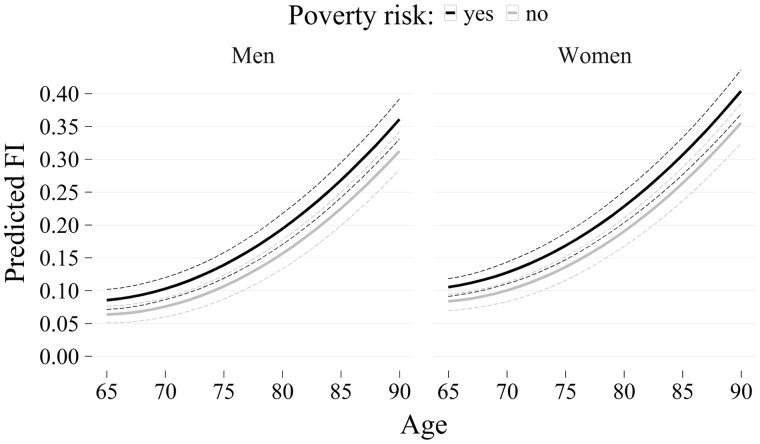
Growth curve models showed that FI increased progressively with age (linear = 0.046, CI = 0.040–0.051; quadratic = 0.009, CI = 0.009–0.010) (figure 1). Older adults at PR were frailer ( = 0.034, CI = 0.028–0.042) than their non-poor counterparts. The interaction effect between PR and age ( = 0.005, CI = 0.002–0.009) indicated that the negative impact of PR increased with age, although the rate of change was negligibly small (figure 1). At age 75, the FI of older men (FIpredicted = 0.139, CI = 0.122–0.162) and women (FIpredicted = 0.168, CI = 0.152–0.191) at PR equated to the FI of males and females not-at-PR at ages 78.5 (FIpredicted = 0.140, CI = 0.122–0.160) and 78 (FIpredicted = 0.167, CI = 0.150–0.190). Accordingly, a 3.0–3.5-year gap of advanced physiological decline was attributable to PR.
Figure 1.
Predicted frailty trajectories by PR for older men and women (65+). Notes: Predicted frailty trajectories based on the fixed part of the model with 95% confidence intervals (dashed lines). FI, frailty index
Table 2 shows the results of the nested multilevel growth curve models. Note that the effect of poverty decreased and model fit increased particularly when psychosocial factors were included (model IV). Analysis of pathway factors (not tabulated) showed that each set of potential pathway factors included separately (models II–V) reduced the impact of PR: behavioural = −8.8%, education = −17.6%, material = −20.6%, psychosocial = −44.1%. The individual contributions from each set of factors in explaining the impact of PR on frailty, net of other factors, were: 20.6% for psychosocial factors, 8.8% for material and only 2.9% for education and health behaviour, respectively. Overlap in the contribution between factors, i.e. indirect effects running through multiple sets of predictors, was considerable (26.5%). For the explanation of the poverty-frailty link, financial difficulties (material), perceived control (psychosocial) and exercising (behavioural) were the most important respective variables. In total, 61.8% of the association between PR and frailty were accounted for.
Table 2.
Nested multilevel growth curve models of FI
| Model I poverty | Model II education | Model III material | Model IV psychosocial | Model V behavioural | Model VI full model | |
|---|---|---|---|---|---|---|
| [CI-95] | [CI-95] | [CI-95] | [CI-95] | [CI-95] | [CI-95] | |
| At PR (ref.: No) | ||||||
| Yes | 0.034 [0.028, 0.040] | 0.028 [0.022, 0.034] | 0.027 [0.021, 0.034] | 0.019 [0.017, 0.034] | 0.031 [0.026, 0.044] | 0.013 [0.007, 0.018] |
| Education level: (ref.: ISCED 0–1) | ||||||
| ISCED 2 | – | −0.022 [−0.028, −0.016] | – | – | – | −0.013 [−0.019, −0.008] |
| ISCED 3 | – | −0.029 [−0.035, −0.023] | – | – | – | −0.015 [−0.020, −0.009] |
| ISCED 4–6 | – | −0.037 [−0.043, −0.031] | – | – | – | −0.014 [−0.020, −0.008] |
| Great financial difficulties (ref.: No) | ||||||
| Yes | – | – | 0.026 [0.021, 0.031] | – | – | 0.013 [0.009, 0.018] |
| Low-quality accommodation (ref.: No) | ||||||
| Yes | – | – | 0.021 [0.015, 0.023] | – | – | 0.014 [0.009, 0.020] |
| Neighbourhood problems (ref.: No) | ||||||
| Yes | – | – | 0.022 [0.017, 0.027] | – | – | 0.014 [0.010, 0.019] |
| Forgone health care due to non-availability (ref.: No) | ||||||
| Yes | – | – | 0.048 [0.032, 0.064] | – | – | 0.039 [0.024, 0.053] |
| Forgone health care due to non-affordability (ref.: No) | ||||||
| Yes | – | – | 0.064 [0.053, 0.076] | – | – | 0.052 [0.041, 0.061] |
| Partnership (ref.: Yes) | ||||||
| No | – | – | – | 0.004 [0.000, 0.007] | – | 0.002 [−0.006, 0.001] |
| Often lonely (ref.: No) | ||||||
| Yes | – | – | – | 0.014 [0.06, 0.021] | – | 0.013 [0.006, 0.019] |
| Social participation (ref.: Yes) | ||||||
| No | – | – | – | 0.016 [0.013, 0.018] | – | 0.013 [0.011, 0.016] |
| Social prestige (13–78)/10 | – | – | – | −0.006 [−0.007, −0.005] | – | −0.003 [−0.005, −0.002] |
| Perceived control (3–12) | – | – | – | −0.014 [−0.015, −0.013] | – | −0.013 [−0.014, −0.013] |
| Subjective well-being (3–12) | – | – | – | −0.007 [−0.008, −0.006] | – | −0.007 [−0.007, −0.005] |
| Heavy smoker (ref.: No) | ||||||
| Yes | – | – | – | – | 0.015 [0.009, 0.020] | 0.011 [0.006, 0.016] |
| Daily alcohol consumption (ref.: No) | ||||||
| Yes | – | – | – | – | −0.014 [−0.018, −0.011] | −0.009 [−0.012, 0.006] |
| Frequent sport/physical activity (ref.: Yes) | ||||||
| No | – | – | – | – | 0.030 [−0.033, −0.027] | −0.024 [−0.026, −0.021] |
| R2 | 0.234 | 0.247 | 0.254 | 0.341 | 0.246 | 0.369 |
Notes: SHARE waves 1,2,4,5 (release 5.0.0), 28 360 observations from 11 390 respondents from 10 countries. , non-standardized regression coefficients of FI at average age. CI-95, 95% confidence interval. All models were adjusted for age, age2, sex, sex*age, birth cohort, non-response, death, and poverty*age. R2 refers to the fixed effects (marginal R2).
Sensitivity analysis
The results of the sensitivity analyses are found in Supplementary Tables S3 and S4. First, we tested the robustness of our results with regard to the imputation procedure. When compared with list-wise deletion, results based on multiple imputation showed better model fits and highly similar substantive results. Second, we stratified the analyses by sex since PR is known to be more prevalent among older women and since their frailty/growth levels are higher/steeper than those of men. However, sex-based differences were modest only. Third, childhood SES and health and adult health problems could confound our results. Based on retrospective interviews from the subset of respondents who participated in the third wave, we thus expanded our models to include childhood conditions at age 10 (health, SES) and health problems during adulthood (physical injuries, longer periods of ill-health/disability) (Supplementary Table S5). In the growth curve models, poorer SES and health in childhood and later health problems were independently associated with increased old-age FI. Importantly, controlling for these predictors and consequently relying on a smaller subset of respondents did neither change the results with regard to PR nor the pathway variables. Fourthly, frailty levels and time-varying predictor variables were measured at the same point in time, which allows for causality to potentially work both ways. Thus we computed models using lagged time-varying predictors to depict the relationship between a predictor, such as regularly engaging in sport/physical activity, and FI in the subsequent wave 2/4 years later. These lagged models showed only small to moderate effect reductions for the time-varying predictors, but left both the direction of the association and statistical significance untouched, thus supporting the hypothesized direction of causation.
Discussion
This study analysed pathway variables linking PR and old-age frailty in 10 European countries. We operationalized PR based on ‘both’ low income and wealth. Considering wealth is important since older adults tend to have (accumulated) above-average wealth.24 Indeed, we found that only a third of the older adults at income PR in our study reported at the same time low household wealth and a quarter, conversely, belonged to the wealthiest 40%. This is to say that researchers should pay more attention to both income and wealth when ascribing and assessing old-age poverty.
Poverty status can be considered a particularly relevant social determinant of health as it corresponds to a complex of accumulated risk factors. We attempted to shed light on the explanatory value of material, psychosocial and behavioural factors for the poverty-health association in old age which are analytically different, but in social reality often intertwined. Our study has shown PR to be associated with increased FI, comparable to the sex-disparity. This impact of PR on FI levels is in line with the adverse health effects of PR found in previous studies.2–11 Specifically, with regard to the adjusted effect of PR, a study10 using data from the US reported a highly similar effect size. Furthermore, we found the effect to slightly increase over time, which is compatible with both the status maintenance hypothesis,34 which outlines that SES attained in middle age continues to affect health in old-age, and the cumulative advantage theory.35 The latter asserts that disadvantages such as living at PR in old age—itself often the result of early childhood disadvantage, low education, and restricted or low-income employment history and inheritance—do accumulate further over time. For a clearer picture, however, further research based on longitudinal data covering the whole life course is required.
In our analysis of the explanatory value of material, psychosocial and behavioural factors with regard to the poverty-health link, we found a substantial overlap between the different types of factors similar to a recent study from the Netherlands.16 This supports the notion of poverty as a complex of interlinked risk factors. In contrast to a recent systematic review study on the SES-health link17 but in line with the results from one of the few studies focussing on older adults,15 we found psychosocial factors such as social isolation,14 well-being36 and in particular perceived control12,13,15,16 more important than material factors. Via sensitivity analyses, we demonstrated these to be robust relationships, supporting a causal link between multiple psychosocial factors and frailty.
In contrast, we found the impact of behavioural factors to be small, which is also in line with previous studies12,13,15 assessing the SES-health link. Frequent physical activity was less prevalent among respondents at PR,23 while heavy smoking was not associated with PR at all, and daily alcohol consumption was even less prevalent among those at PR. The latter could be due to the measurement method used in SHARE, which relied on the frequency of alcohol intake rather than on quantity. Indeed, it has been reported37 that lower SES groups tended to drink more heavily, whereas higher SES groups tended to drink more frequently instead. Expectedly, smokers with more than 30 pack-years and those who were not physically active showed increased levels of frailty, whereas the effect of frequent alcohol consumption was reversed.38 With respect to explaining the poverty–frailty link, however, a lifetime of heavy smoking and current lack of regular physical exercise hardly mattered.12,13,15,16 In other words, we found that while those at PR partly behaved more poorly with regard to their health,19 only a small proportion of the negative impact of PR on physical health in later life was attributable to such behaviour.
From a public health perspective, health care coverage generally seemed adequate in the 10 European countries included, with only a small minority (<4%) reporting forgone health care due to non-availability/affordability. However, forgone health care utilization was associated with a substantially increased FI, childhood SES predicted old-age health despite a large number of control variables, and the PR-related gap in frailty persisted, even slightly increased throughout old age. Thus, public health intervention should be intensified with regard to poverty and its negative consequences from an early age on. Against the backdrop of the small contribution of health behaviour and the more substantial effect of material, but particularly psychosocial factors in explaining the PR-related health gap, ambitions of public health policies should be redirected. They should be expanded towards improving the socio-economic and -cultural context in which poverty and, in consequence, a perceived lack of control over one’s life as well as social isolation are generated and reinforced. Thus interventions should rather focus on empowerment39 than on individual health behaviour and the alleged responsibility thereof.19,40
To our knowledge, this is the first study focussing on variables explaining how PR translates into poorer physical health among older adults. Further strengths of this article are the cross-national, longitudinal data used, the range of potential pathway variables tested and the extensive sensitivity analyses supporting the robustness of the results.
Our study, however, has several limitations as well. First, although longitudinal panel data covering four waves of SHARE was used, information on a number of predictor variables was available only for wave 1; therefore, subsequent changes in these variables were not considered. Second, with regard to variable selection, we endeavoured to include a large variety of predictors; however, information on several potentially important factors was missing: past working and housing conditions, quantity of alcohol intake, family problems, shame and social stigma. Third, poor older adults and those with high FI are likely under-represented in SHARE since they are arguably less easily available (institutionalization), capable or willing to participate in extensive survey studies.
In conclusion, we found PR associated with increased levels of frailty among older adults, and the gap persisted, even slightly increased throughout old age. Rather than educational or behavioural factors, material and in particular, psychosocial factors such as perceived control and social isolation explained a large part of PR-related differences in frailty. Future research and public health efforts should focus on the socioeconomic and sociocultural context in which these factors are generated and reinforced, rather than to concentrate on behavioural aspects alone.
Supplementary data
Supplementary data are available at EURPUB online.
Funding
This work was supported by no specific institution but only the Medical University of Graz. This article uses data from SHARE Waves 1, 2, 3 (SHARELIFE), 4 and 5 (DOIs: 10.6103/SHARE.w1.260, 10.6103/SHARE.w2.260, 10.6103/SHARE.w3.100, 10.6103/SHARE.w4.111, 10.6103/SHARE.w5.100). The SHARE data collection has been primarily funded by the European Commission through FP5 (QLK6-CT-2001-00360), FP6 (SHARE-I3: RII-CT-2006-062193, COMPARE: CIT5-CT-2005-028857, SHARELIFE: CIT4-CT-2006-028812) and FP7 (SHARE-PREP: N211909, SHARE-LEAP: N227822, SHARE M4: N261982). Additional funding from the German Ministry of Education and Research, the US National Institute on Aging (U01_AG09740-13S2, P01_AG005842, P01_AG08291, P30_AG12815, R21_AG025169, Y1-AG-4553-01, IAG_BSR06-11, OGHA_04-064) and from various national funding sources is gratefully acknowledged (see www.share-project.org).
Conflicts of interest: None declared.
Key points
Poverty has been found to be detrimental for physical health among older adults, but the impact of multiple pathway factors (material, psychosocial, behavioural, education) in explaining this poverty-health link has not been studied to date.
Poor older adults showed significantly higher frailty levels than non-poor older adults, and the gap slightly increased over time.
In total, 62% of the impact of poverty on frailty could be explained; the detrimental effect of poverty on health was mainly due to psychosocial factors and material factors, whereas the impact of behavioural factors was small.
Overlap between education, material, psychosocial and behavioural factors was substantial, which highlights poverty as a complex of interacting risk factors for health.
Efforts to fight poverty and its detrimental health effects should be strengthened and the scope of interventions should be broadened with regard to psychosocial factors.
Supplementary Material
References
- 1. Townsend P. (1979): Poverty in the United Kingdom. Penguin: Hamondsworth. [Google Scholar]
- 2. Grundy E, Slogget A. Health inequalities in the older population: the role of personal capital, social resources and socio-economic circumstances. Soc Sci Med 2003;56:935–47. [DOI] [PubMed] [Google Scholar]
- 3. Groffen DAI, Bosma H, van den Akker M, et al. Material deprivation and health-related dysfunction in older Dutch people: findings from the SMILE study. Eur J Public Health 2007;18:258–63. [DOI] [PubMed] [Google Scholar]
- 4. Crimmins EM, Kim JK, Seeman TE. Poverty and biological risk: The earlier “aging” of the poor. J Gerontol Med Sci 2009;64:286–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Pförtner T-K, Andress H-J, Janssen C. Income or living standard and health in Germany: different ways of measurement of relative poverty with regard to self-rated health. Int J Public Health 2011;56:373–84. [DOI] [PubMed] [Google Scholar]
- 6. Loui GH, Ward MM. Socioeconomic and ethnic differences in disease burden and disparities in physical function in older adults. Am J Public Health 2014;101:1322–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Saito M, Kondo K, Kondo N, et al. Relative deprivation, poverty, and subjective health: JAGES cross-sectional study. PLoS One 2014;9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Lynch JW, Kaplan GA, Shema SJ. Cumulative impact of sustained economic hardship on physical, cognitive, psychological, and social functioning. N Engl J Med 1997;337:1889–95. [DOI] [PubMed] [Google Scholar]
- 9. McDonough P, Sacker A, Wiggins RD. Time on my side? Life course trajectories of poverty and health. Soc Sci Med 2005;61:1795–808. [DOI] [PubMed] [Google Scholar]
- 10. Yang Y, Lee LC. Dynamics and heterogeneity in the process of human frailty and aging: Evidence from the U.S. older adult population. J Gerontol Soc Sci 2010;65:246–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Adena M, Myck M. Poverty and transitions in health in later life. Soc Sci Med 2014;116:202–10. [DOI] [PubMed] [Google Scholar]
- 12. Van Lenthe FJ, Schrijvers CT, Droomers M, Joung IM, et al. Investigating explanations of socio-economic inequalities in health. Eur J Public Health 2004;14:63–70. [DOI] [PubMed] [Google Scholar]
- 13. Van Oort FVA, van Lenthe FJ, Mackenbach JP. Material, psychosocial, and behavioural factors in the explanation of educational inequalities in mortality in the Netherlands. J Epidemiol Community Health 2005;59:214–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Aldabe B, Anderson R, Lyly-Yränäinen M, et al. Contribution of material, occupational, and psychosocial factors in the explanation of social inequalities in health in 28 countries in Europe. J Epidemiol Community Health 2011;65:1123–231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Groffen DAI, Bosma H, Tan FES, et al. Material vs. psychosocial explanations of old-age educational differences in physical and mental functioning. Eur J Public Health 2011;22:587–92. [DOI] [PubMed] [Google Scholar]
- 16. Hoogendijk EO, van Hout HPJ, Heymans MW, et al. Explaining the association between educational level and frailty in older adults: results from a 13-year longitudinal study in the Netherlands. Ann Epidemiol 2014;24:538–44. [DOI] [PubMed] [Google Scholar]
- 17. Moor I, Spallek J, Richter M. Explaining socioeconomic inequalities in self-rated health: A systematic review of the relative contribution of material, psychosocial and behavioral factors. J Epidemiol Community Health Published Online First: 28 September 2016. [DOI] [PubMed] [Google Scholar]
- 18. Kahn JR, Pearlin LI. Financial strain over the life course and health among older adults. J Health Soc Behav 2006;47:17–31. [DOI] [PubMed] [Google Scholar]
- 19. Lynch JW, Kaplan GA, Salonen JT. Why do poor people behave poorly? Variation in adult health behaviours and psychosocial characteristics by stages of the socioeconomic lifecourse. Soc Sci Med 1997;44:809–16. [DOI] [PubMed] [Google Scholar]
- 20. Evans GW, Kantrowitz E. Socioeconomic status and health: the potential role of environmental risk exposure. Annu Rev Public Health 2002;23:303–31. [DOI] [PubMed] [Google Scholar]
- 21. Cohen DA, Farley TA, Mason K. Why is poverty unhealthy? Social and physical mediators. Soc Sci Med 2003;57:1631–41. [DOI] [PubMed] [Google Scholar]
- 22. Krueger PM, Chang VW. Being poor and coping with stress. Health behaviors and the risk of death. Am J Public Health 2008;98:889–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Aue K, Roosen J, Jensen HH. Poverty dynamics in Germany: evidence on the relationship between persistent poverty and health behaviour. Soc Sci Med 2016;153:62–70. [DOI] [PubMed] [Google Scholar]
- 24. Hansen T, Slagsvold B, Moum T. Financial satisfaction in old age: a satisfaction paradox or a result of accumulated wealth? Soc Indic Res 2008;89:323–47. [Google Scholar]
- 25. Rockwood K, Mitnitski A. Frailty in relation to the accumulation of deficits. J Gerontol Med Sci 2007;62:722–7. [DOI] [PubMed] [Google Scholar]
- 26. Searle SD, Mitnitski A, Gahbauer EA, Gill TM, Rockwood K. A standard procedure for creating a frailty index. BMC Geriatrics 2008;8:24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Romero-Ortuno R. The frailty index in Europeans: associations with determinants of health. Geriatr Gerontol Int 2014;14:420–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Eurostat: Glossary: At-risk-of-poverty rate, 2014. Available at: http://ec.europa.eu/eurostat/statistics-explained/index.php/Glossary:At-risk-of-poverty_rate, (5 June 2016, date last accessed).
- 29. Hyde M, Wiggins RD, Higgs P, Blane DB. A measure of quality of life in early old age: The theory, development and properties of a needs satisfaction model (CASP-19). Aging Ment Health 2003;7:186–94. [DOI] [PubMed] [Google Scholar]
- 30. Bowling A. Mode of questionnaire administration can have serious effects on data quality. J Public Health 2005;27:281–91. [DOI] [PubMed] [Google Scholar]
- 31. Korkeila K, Suominen S, Ahvenainen J, et al. Non-response and related factors in a nation-wide health survey. Eur J Epidemiol 2001;17:991–9. [DOI] [PubMed] [Google Scholar]
- 32. Collins LM, Schafer JL, Kam C-M. A comparison of inclusive and restrictive strategies in modern missing data procedures. Psychol Methods 2001;6:330–51. [PubMed] [Google Scholar]
- 33. Raudenbush S, Bryk A. Hierachical Linear Models. Thousand Oaks: SAGE Publications, 2002. [Google Scholar]
- 34. O’Rand AM, Henretta JC. Age and Inequality. Diverse Pathways Through Later Life. Colorado: Westview Press, 1999. [Google Scholar]
- 35. Dannefer D. Cumulative advantage/disadvantage and the life course: Cross-fertilizing age and social science theory. J Gerontol Soc Sci 2003;58:327–37. [DOI] [PubMed] [Google Scholar]
- 36. Steptoe A, Deaton A, Stone AA. Subjective wellbeing, health, and ageing. Lancet 2015;285:640–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Huckle T, You RQ, Caswell S. Socio-economic status predicts drinking patterns but not alcohol-related consequences independently. Addiction 2010;105:1192–202. [DOI] [PubMed] [Google Scholar]
- 38. Ronksley PE, Brien SE, Turner BJ, et al. Association of alcohol consumption with selected cardiovascular disease outomes: a systematic review and meta-analysis. BMJ 2011;342:d671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Tengland P-A. Behavior change or empowerment: On the ethics of health-promotion goals. Health Care Anal 2016;24:24–46. [DOI] [PubMed] [Google Scholar]
- 40. Guttman N, Ressler WH. On being responsible: Ethical issues in appeals to personal responsibility in health campaigns. J Health Commun 2001;6:117–36. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.