Abstract
An esophageal mucosal bridge is a rare finding that is seldom encountered on upper endoscopy. They most commonly present secondary to an underlying inflammatory disorder and cause chest pain and dysphagia, among other symptoms. More rarely, they present asymptomatically with no identifiable inflammatory conditions. Our case consists of a 31-year-old woman who presented with an asymptomatic, noninflammatory mucosal bridge of the esophagus. To our knowledge, this makes the third such case. The rarity of this condition coupled with the lack of epidemiologic data available make this case worthy for literature review.
Keywords: mucosal bridge, dysphagia, esophagus, endoscopy
Introduction
Mucosal bridges are linear extensions of smooth muscle that connect across the lumen of the gastrointestinal tract. The resulting connection gives the appearance of a “double lumen” or “pseudo-carina” when visualized on upper endoscopy.1 Cases of mucosal bridges are rare, with reported sites including the esophagus, gastric antrum, small intestine, colon, and biliary tree.2 Clinically, symptoms vary greatly depending on their location, and are at times asymptomatic. Of note, there have been reported cases of mucosal bridges presenting in the vocal cords but are outside the scope of this discussion.3
Case Report
A 31-year-old woman with medical comorbidities of HIV on antiretroviral therapy and granulomatous hepatitis related to Mycobacterium avium intracellulare presented to the emergency department complaining of fatigue and malaise of 5 days duration. The patient denies any fevers, headache, nausea, vomiting, abdominal pain, diarrhea, constipation, bright red blood per rectum, or heavy menstruation. She claimed she is compliant with her medications. On presentation, the patient was afebrile with blood pressure of 138/78 mm Hg, heart rate of 84 beats per minute, and 98% saturation on room air. Physical examination revealed pallor but otherwise not significant. Laboratory workup revealed severe anemia with hemoglobin of 6 g/dL and mean corpuscular volume of 78 fL. Iron profile revealed iron levels of 40 µg/dL and total iron binding capacity of 440 µg/dL; otherwise blood work was not significant. The patient was transfused 2 units of packed red blood cells. As a part of the anemia workup, a diagnostic endoscopy and colonoscopy was scheduled. Esophagogastroduodenoscopy revealed a mucosal bridge across the lower third of the esophagus giving the appearance of “pseudo-carina” (Figures 1 and 2). Endoscopic appearance did not suggest any underlying active inflammatory mucosal pathology. As the patient was asymptomatic and had not complained of dysphagia or odynophagia, the mucosal bridge was not manipulated. Esophagogastroduodenoscopy and colonoscopy were completed, and no pathology was found toward anemia. We concluded that this mucosal bridge could be a congenital anomaly or that arising from a prior unrecognized (and healed) HIV-related opportunistic infection(s). Noninflammatory esophageal mucosal bridges are very rare. To our knowledge, this is the third case of a noninflammatory esophageal mucosal bridge being reported. The patient is followed-up by hematology to diagnose the etiology and treat anemia.
Figure 1.
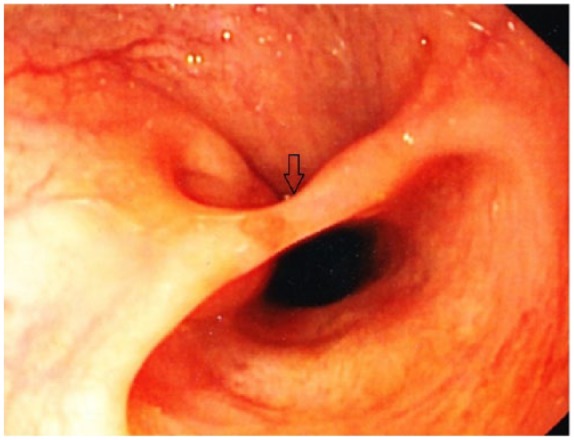
Esophagogastroduodenoscopy revealed a mucosal bridge (black arrow) across the lower third of the esophagus on view 1.
Figure 2.
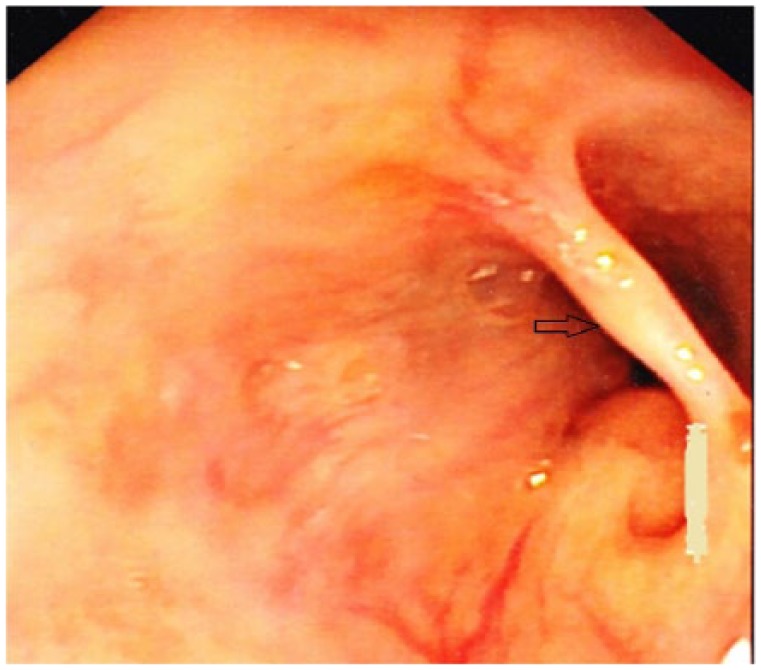
Esophagogastroduodenoscopy revealed a mucosal bridge (black arrow) across the lower third of the esophagus on view 2.
Discussion
Despite the first esophageal mucosal bridge being described in 1969, there is still a dearth of epidemiologic data available in the literature.4 This, for the most part, is attributed to their rare occurrence. Subsidiary reasons for their uncommon incidence may be due to the fact that many cases present asymptomatically, as was the case with our patient. Given the new, stricter guidelines regarding upper endoscopy, if a patient does not present with alarm signs, a mucosal bridge may go undiagnosed for quite some time.5
The pathogenesis of mucosal bridges is also a subject of contention. Current theories postulate an underlying inflammatory process as the main etiology behind its development.6 When the walls of inflamed esophagus come into contact with each other, the underlying granulation tissue of each wall develop adhesions, leading to the formation of mucosal bridges.7 The well-established relationship of inflammatory bowel disease and mucosal bridges support this theory.8 Another theory proposes ulceration as the root cause. The rationale behind this theory is healing of an ulcer by reepithelialization of the mucosal undersurface and subsequent formation of a mucosal tube attached at each end to nonulcerated bowel wall.9 In addition to inflammatory bowel disease, other documented associations of esophageal mucosal bridges include lupus, tuberculosis, esophageal candidiasis, reflux esophagitis, and radiation esophagitis.1,10-13 Cases have also been found to arise following esophageal variceal sclerotherapy and traumatic insertion of a nasogastric tube.14,15 Our patient presented with a noninflammatory mucosal bridge with none of the aforementioned associations. These cases are exceedingly rare, with only 2 other reported cases in the literature to our knowledge. A congenital malformation is considered to be the culprit in these cases.
Symptoms of esophageal mucosal bridges include chest pain, obstructive symptoms, weight loss, and intermittent bleeding.16 Currently, there are a variety of treatment options available for eradication of esophageal mucosal bridges. Argon plasma coagulation therapy has been used successfully in several cases.1,17 Another technique that has proven effective consists of placing a hemostatic clip at each end of the bridge and incising the center of the bridge with electrocautery.16,18 There is no data that support one method over the other, leaving the choice to the discretion of the endoscopist.
Conclusion
In conclusion, esophageal mucosal bridges are rare entities that can be acquired, or less commonly, developed congenitally. Due to their rarity, there is a lack of epidemiologic data available in the literature. What is clear however is that treatment with argon plasma coagulation or electrocautery has shown to be effective with no reported recurrences. In asymptomatic patients the decision to treat should be deferred to the patient.
Footnotes
Authors’ Note: The case report was presented in the form of an abstract (poster) in the American College of Gastroenterology conference in Las Vegas, Nevada (October 2016).
Author Contributions: Conception: Tagore Sunkara and Vinaya Gaduputi
Drafting of the article: Tagore Sunkara, Eric Omar Then, Krishna Sowjanya Yarlagadda, Manan Jhaveri, and Vinaya Gaduputi
Critical revision of the article: Tagore Sunkara, Eric Omar Then, Krishna Sowjanya Yarlagadda, Manan Jhaveri, and Vinaya Gaduputi
Final approval of the article: Tagore Sunkara, Eric Omar Then, Krishna Sowjanya Yarlagadda, Manan Jhaveri, and Vinaya Gaduputi
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Informed Consent: Verbal informed consent was obtained from the patient(s) for their anonymized information to be published in this article.
Ethics Approval: Ethical approval to report this case was obtained from the SBH Health System institutional review board (Approval Number: 2016.46).
ORCID IDs: Tagore Sunkara  https://orcid.org/0000-0001-9536-9027
https://orcid.org/0000-0001-9536-9027
Krishna Sowjanya Yarlagadda  https://orcid.org/0000-0001-6119-9672
https://orcid.org/0000-0001-6119-9672
Eric Omar Then  https://orcid.org/0000-0003-3649-1190
https://orcid.org/0000-0003-3649-1190
Vinaya Gaduputi  https://orcid.org/0000-0002-3789-5392
https://orcid.org/0000-0002-3789-5392
References
- 1. Cunningham S, Singla M, Itzkowitz S. Esophageal mucosal bridge in a young man with radiation esophagitis. Gastrointest Endosc. 2015;82:1121. [DOI] [PubMed] [Google Scholar]
- 2. Parsi MA. Endoscopic treatment of a symptomatic gastric mucosal bridge. Gastrointest Endosc. 2014;80:723. [DOI] [PubMed] [Google Scholar]
- 3. Martins RH, Tavares EL, Fabro AT, Martins MG, Dias NH. Mucosal bridge of the vocal fold: difficulties in the diagnosis and treatment. J Voice. 2012;26:127-131. [DOI] [PubMed] [Google Scholar]
- 4. Saha AK, Kundu AK. Mucosal bridge in oesophagus. J Assoc Physicians India. 2014;62:704-705. [PubMed] [Google Scholar]
- 5. ASGE Standards of Practice Committee; Early DS, Ben-Menachem T, et al. Appropriate use of GI endoscopy. Gastrointest Endosc. 2012;75:1127-1131. [DOI] [PubMed] [Google Scholar]
- 6. Chang FY, Lai KH, Lee SD, Tsai YT. Asymptomatic mucosal bridge of the upper esophagus. Gastrointest Endosc. 1989;35:472-473. [DOI] [PubMed] [Google Scholar]
- 7. Vazifdar KF, Wagle SD, Dhir V. Multiple mucosal bridges of esophagus: an unusual cause of dysphagia. Indian J Gastroenterol. 1996;15:152. [PubMed] [Google Scholar]
- 8. Fefferman DS, Farrell RJ. Endoscopy in inflammatory bowel disease: indications, surveillance, and use in clinical practice. Clin Gastroenterol Hepatol. 2005;3:11-24. [DOI] [PubMed] [Google Scholar]
- 9. Waye JD. Endoscopy in inflammatory bowel disease. Clin Gastroenterol. 1980;9:279-296. [PubMed] [Google Scholar]
- 10. Itano T, Tomoda J, Harada H, et al. A case of systemic lupus erythematosus with esophageal mucosal bridge [in Japanese]. Nihon Shokakibyo Gakkai Zasshi. 1986;83:2598-2601. [PubMed] [Google Scholar]
- 11. Shikiya K, Kinjo N, Akamine K, et al. A case of mid-esophageal diverticulum with mucosal bridge caused by tuberculosis of the apex of the right lung [in Japanese]. Nihon Shokakibyo Gakkai Zasshi. 1991;88:724-729. [PubMed] [Google Scholar]
- 12. Rattan J, Hallak A, Rozen P, Werbin N, Gilat T. Esophageal monilioma and mucosal bridge. Gastrointest Endosc. 1982;28:114-115. [DOI] [PubMed] [Google Scholar]
- 13. Kume K, Yoshikawa I. Mucosal bridge due to reflux esophagitis. Gastroenterol Insights. 2009;01:e4. doi: 10.4081/gi.2009.e4. [DOI] [Google Scholar]
- 14. Gottfried EB, Goldberg HJ. Mucosal bridge of the distal esophagus after esophageal variceal sclerotherapy. Gastrointest Endosc. 1985;31:267-269. [DOI] [PubMed] [Google Scholar]
- 15. Buchman AL, Waring JP. Mucosal bridge formation in the esophagus caused by injury from a nasoenteric feeding tube. JPEN J Parenter Enteral Nutr. 1994;18:278-279. [DOI] [PubMed] [Google Scholar]
- 16. Ranketi S, Mwachiro M, Topazian M, Burgert S. Endoscopic treatment of cervical esophageal transluminal bridge. Gastrointest Endosc. 2017;86:561-562. [DOI] [PubMed] [Google Scholar]
- 17. Mukherjee M, Oh J, Khdair A, Grosman I. Esophageal mucosal bridges associated with idiopathic esophageal ulcer treated with argon plasma coagulation. Gastrointest Endosc. 2008;68:387-389. [DOI] [PubMed] [Google Scholar]
- 18. Perisetti A, Banerjee D, Tharian B. Clinical challenges and images in gastroenterology: “endoscopic resection of esophageal mucosal bridge” [published online September 9, 2017]. Gastroenterology. doi: 10.1053/j.gastro.2017.08.070. [DOI] [PubMed] [Google Scholar]


