1. Introduction
Rotator cuff (RC) tears are common injuries sustained by competitive overhead athletes resulting from acute trauma or more commonly, chronic degenerative changes from overuse.1, 2 These injuries have been frequently documented in both collegiate and professional level athletes in which a repetitive overhead throwing motion is used.3, 4, 5 When RC tears occur in athletes and younger populations, they tend to result from trauma, multiple subluxations, or repetitive overhead motions where large rotational torques are observed, often occurring in athletes participating in sports such as baseball, tennis, or swimming.6, 7, 8, 9 Brockmeier et al. describes the pathophysiology of RC tears suggesting the microtrauma from repetitive overhead throwing results in supraphysiological tensile and shear forces on the RC.6
When the RC tendons experience excessive loads they become susceptible to tears, especially near the junction of the supraspinatus and infraspinatus.10 The tears are categorized as either full-thickness or partial-thickness, and further categorized by location: on the bursal or articular side of the humerus.11 A subtype of RC tears, known as partial articular-sided supraspinatus tendon avulsion (PASTA) lesions occur at the RC footprint where fibers of the supraspinatus and infraspinatus tendons separate from their bony attachment at the greater tuberosity of the humerus.7, 12, 13 Schaeffeler et al. further described these lesions as a discontinuation of the undersurface of the supraspinatus or infraspinatus fibers located on the articular side, in which contrast material extends into the tendon.7
Although RC injuries are a common etiology for shoulder pain in adults, evidence suggests RC lesions occur less often in the pediatric population, and account for less than 1% of all total RC tears.2, 14 Current literature reports shoulder injuries comprise nearly 11% of all high school athlete injuries15. However, few studies have reported the incidence of RC tears in the pediatric population, with current evidence limited to case reports and small retrospective reviews.14, 15 Additionally, Alley, Banerjee, Papaliodis, Tsitos, Zanaros2, reports the proximal humeral physes is physiologically weaker than the RC resulting in acute physeal separation or proximal humeral epiphysiolysis injuries occurring more commonly from repetitive stress in overhead throwing compared to RC injuries. However, to the best of authors’ knowledge, no literature exists detailing differences in the pathophysiology between rotator cuff tears in the pediatric versus older populations.
Recent literature has reported inconsistencies in the correlation between RC lesions viewed with magnetic resonance imaging (MRI) and those found arthroscopically, 16, 17, 18 especially regarding partial-thickness tears.19 Although studies have demonstrated partial-thickness RC lesions have a higher incidence in younger populations, the definition of younger population in these sources remains varied, with sources including patient populations up to 40 years of age.7 Therefore, in an effort to increase our understanding of operative RC lesions in the pediatric population defined as patients aged 18 years or younger, we examined 1) the prevalence and characteristics of RC lesions in pediatric patients undergoing operative management for shoulder pathology at our institution and 2) compared the accuracy of MRI findings in diagnosing RC lesions confirmed arthroscopically. We hypothesized MRI would accurately detect the location and type of RC lesion in a pediatric cohort.
2. Materials and methods
Following Institutional Review Board approval, a retrospective review of patients with shoulder pathology that resulted in operative management from January 2010 to October 2016 was performed. Patients were identified from Department of Orthopaedics Sports Medicine Institute using the CPT codes listed in Appendix A. Of the 1136 cases identified that received operative intervention secondary to shoulder pathology, a total of 44 patients were aged 12–18 defining the pediatric population age range. Patients were excluded from final analysis if they were older than 18 years, or did not receive operative treatment for shoulder pathologies. A total of ten patients were included in the final observational analysis.
Operative reports and intraoperative arthroscopic images were evaluated to identify RC lesions. All patients underwent arthroscopy by one of three fellowship-trained sports medicine surgeons. A diagnostic arthroscopy was done with a 30° scope through the posterior portal, which is located 2 cm inferior and 1 cm medial to posterolateral corner of acromion. Through the posterior portal the following structures were identified for pathology: Biceps tendon, Supraspinatus, Infraspinatus, Teres Minor, Rotator interval, Anterior ligamentous complex (MGHL, IGHL), Subscapularis recess for loose bodies, Anterior labrum, Glenoid, and Humeral head.
The preoperative MRI was then retrospectively reviewed for documenting RC lesions and confirmed by a fellowship-trained musculoskeletal radiologist. All MRI examinations were performed on 1.5T systems and included the following parameters: Axial T2 FS (TR 3720–3800, TE 28–33, NEX 2 ETL 8, BW 230–240, matrix 384 × 250), coronal oblique T2 FS (TR 4120–4380, TE 57–65, NEX 2, ETL 8–11, BW 230–240, matrix 384 × 250), coronal oblique proton density (TR 2750–2980, TE 38–43, NEX 1–2, ETL 6–8, BW 240, matrix 512 × 307), axial proton density (TR 2650–2800, TE 39–41, ETL 6, BW, 240, matrix 512 × 307), sagittal oblique T1 (TR715- 769, TE 11–27, NEX 1–2, ETL 3–7, BW 165–230, matrix 512 × 307). No IV or intra-articular contrast was utilized. The radiologist was blinded to the original report and arthroscopic findings to minimize interpretation bias. The findings for both MRI and arthroscopy were categorized by anatomic location. Lesions to the rotator cuff tendons were detailed to specify the specific tendon and tear location. Lesions were classified as partial-thickness, full thickness, or footprint lesions. Footprint lesion were defined as lesions located at the insertion of the rotator cuff. The radiologists findings on MRI findings were then compared to the surgeons arthroscopic findings.
3. Results
A total of 1136 cases receiving operative management for shoulder pathology were identified. Of which, 44 patients were between age 12 to 18 years old. Of the 44 pediatric patients identified, 10 patients had RC lesions documented on operative reports. The average age of pediatric patients included in our analysis was 16.7 years (Min: 14 years, Max: 18 years, Table 1).
Table 1.
Demographic data of reported lesions and their associated injuries.
| Sample | Gender | Age | Side | Associated Pathology | Sport | Activity | Trauma |
|---|---|---|---|---|---|---|---|
| 1 | M | 14 | Right | Biceps tendon tear^ | Basketball | Push off wall | Yes |
| 2 | M | 18 | Left | Tight posterior capsule† | Baseball | Pitcher | No |
| 3 | M | 16 | Right | – | Baseball | Pitcher | No |
| 4 | M | 18 | Left | SLAP tear‡ | Baseball | Pitcher | No |
| 5 | M | 16 | Right | SLAP tear Internal impingement |
Baseball | Pitcher | No |
| 6 | M | 18 | Right | Anterior labral tear | Baseball | Sliding into base | Yes |
| 7 | M | 18 | Right | Posterior labral tear | Weight-Lifting | Military press | Yes |
| 8 | M | 17 | Right | Bankart tear SLAP tear Hill-Sachs lesion Biceps tendon tear |
Baseball | Dislocation | Yes |
| 9 | M | 16 | Right | Bankart tear° | – | Instability | No |
| 10 | M | 16 | Right | Bankart tear | Baseball | – | No |
M = Male; SLAP = Superior labral tear from anterior to posterior.
– Data not available.
Biceps tear was debrided intraoperatively.
Posterior capsule tightness was observed and released intraoperatively.
Type 2 SLAP tear.
Patient required posterior labral repair and capsulorrhaphy.
All 10 (100%) patients were males, with 9 of the 10 (90%) cases resulting from sports-related injuries. A majority of RC lesions resulted from baseball injuries, 7 of 10 (70%) cases, with the remaining 3 injuries resulting from basketball, weight-lifting, and chronic instability. An identifiable traumatic event occurred in 4 of 10 (40%) cases, with 2 of 4 (50%) traumatic events occurring during a baseball game. The most common associated pathology were SLAP tears and Bankhart tears (3 cases, 30%, Table 1), followed by bicep tendon tears in 2 cases, (20%, Table 1), Hill-Sachs lesions, internal impingement, and posterior capsule tightness in 1 case each. Table 2. details the characterization and management of RC lesions identified via MRI or arthroscopically in the operating room (OR). Four of the RC lesions were managed with debridement and the remaining 6 lesions were repaired in a side-to-side fashion if the lesion was a partial-thickness tear or via reattachment to the RC footprint with anchors if the lesion involved the footprint.
Table 2.
Characterization and management of rotator cuff lesions identified via magnetic resonance imaging or arthroscopic findings in the operating room.
| Preoperative MRI |
OR |
||||||||
|---|---|---|---|---|---|---|---|---|---|
| Patient | Tear | Type | Location | Tendon(s) Involved | Tear | Type | Location | Tendon(s) Involved | Treatment |
| 1 | Yes | FP | Articular | Supraspinatus Infraspinatus |
Yes | PT | Articular | Supraspinatus | Repair |
| 2 | Yes | PT | Articular | Supraspinatus Infraspinatus |
Yes | FP | Articular | Supraspinatus | Repair |
| 3 | No | X | X | X | Yes | FP | Articular | Supraspinatus | Repair |
| 4 | – | – | – | – | Yes | FP | Articular | Supraspinatus | Repair |
| 5 | Yes | FP | Articular | Infraspinatus | Yes | PT | Articular | Infraspinatus | Repair |
| 6 | – | – | – | – | Yes | PT | Articular | Infraspinatus | Repair |
| 7 | No | X | X | X | Yes | PT | Articular | Supraspinatus | Debridement |
| 8 | Yes | PT | Bursal | Supraspinatus | Yes | PT | Bursal | – | Debridement |
| 9 | Yes | PT | Articular | Supraspinatus | Yes | PT | Articular | Supraspinatus | Debridement |
| 10 | – | – | – | – | Yes | PT | Articular | Supraspinatus | Debridement |
MRI = Magnetic resonance imaging; OR = Operating Room; FP = Footplate; PT = Partial-thickness
– Data not available.
X Data not applicable.
3.1. MRI findings
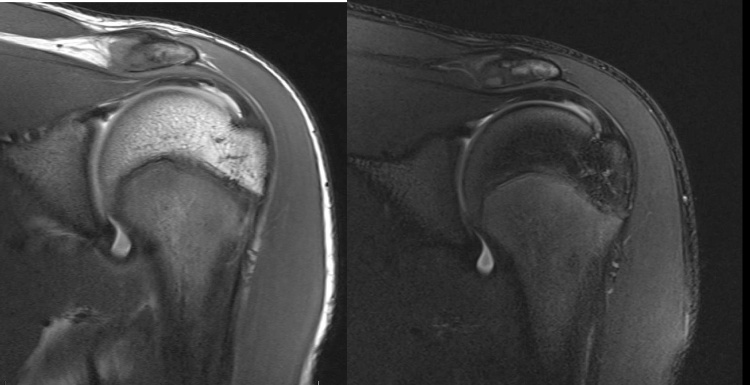
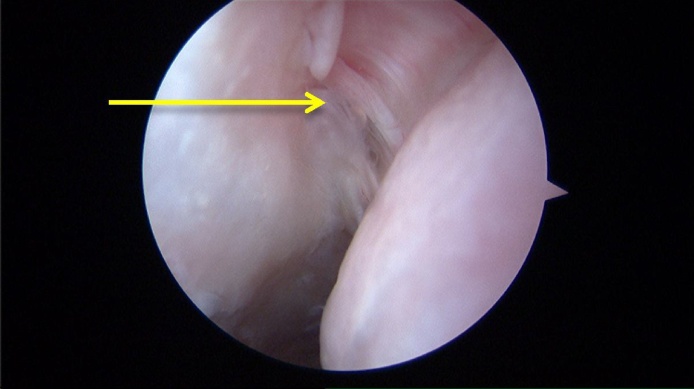
Of the 10 cases included in the analysis, 7 (70%) cases had preoperative MRIs, of which 5 (71.4%) cases identified RC lesions. Of the documented RC lesions, 2 (40%) were reported as footprint lesions (Table 2, Fig. 1) and 3 (60%) were reported as partial-thickness lesions (Table 2, Fig. 2).
Fig. 1.
Coronal View, Proton Density (Left) and T2 Fat Saturated (Right) MRI of the left shoulder showing a footprint (PASTA) lesion.
Fig. 2.
Right shoulder MRI in coronal view showing partial-thickness bursal-sided tear of the supraspinatus.
Lesions were reported as articular-sided in 4 (80%) cases and bursal-sided in 1 (20%) case. Isolated involvement of the supraspinatus and infraspinatus tendon was reported in 2 (40%) and 1 (20%) of the cases, respectively. Involvement of both the supraspinatus and infraspinatus tendons was reported in 2 (40%) of cases.
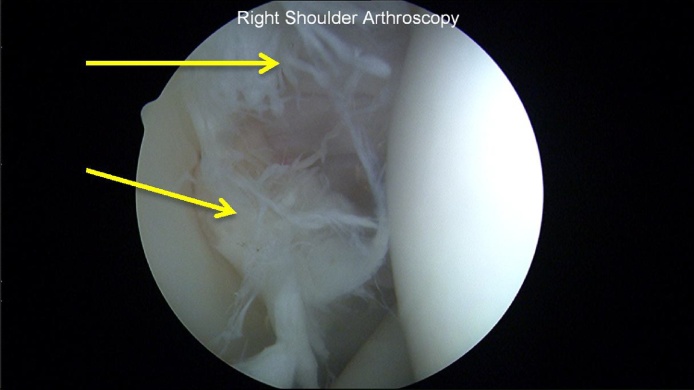
3.2. Arthroscopic findings
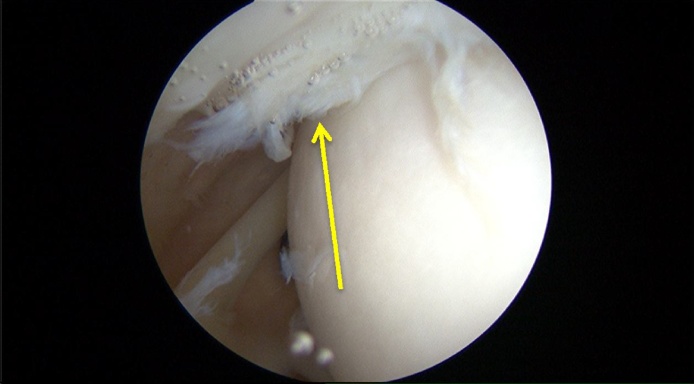
RC lesions were identified in all 10 (100%) cases included in the analysis. Footprint and partial-thickness lesions were identified in 3 (30%, Fig. 3) and 7 (70%, Fig. 4) of cases, respectively.
Fig. 3.
Left shoulder arthroscopic view demonstrating supraspinatus tear.
Fig. 4.
Right shoulder arthroscopic view demonstrating supraspinatus tear.
The majority of lesions (Fig. 5) were articular-sided (9 cases, 90%, Table 2), and 1 lesion (10%, Table 2) was bursal-sided. Isolated involvement of the supraspinatus and infraspinatus tendon was reported in 7 (77.8%) and 2 (22.2%) of cases, respectively. One of the 10 cases failed to report tendon involvement.
Fig. 5.
Right shoulder partial thickness tear to the infraspinatus, viewed on the articular side of the rotator cuff.
3.3. Arthroscopic and MRI evaluation
Of all 10 operative cases with confirmed RC lesions viewed arthroscopically, 7 (70%) cases had preoperative MRIs. Of the preoperative MRIs, 2 of 7 (28.5%) missed RC lesions visualized intraoperatively. Of the 5 cases with preoperative MRIs correctly identifying RC lesions, all 5 (100%, Table 2) and 4 of 5 (80%) accurately reported the location and tendon involvement of the RC lesion, respectively. However, 2 of the MRI reports reported tendon involvement not observed intraoperatively. The type of lesion was accurately described in only 2 of 5 (40%) MRI reports.
4. Discussion
The current study contributes to limited prior publications focusing on RC lesions in pediatric populations. Uniquely, the current study compares MRI imaging obtained preoperatively to findings intraoperatively via arthroscopy in patients who underwent operative intervention for shoulder pathology at a single academic institution. The current study suggests MRI is an accurate preoperative instrument for RC lesion localization in the pediatric population; however, may be limited in identifying RC tear type in the same population. Prior literature examining radiological use have reported limitations in the diagnosis of RC tears with MRI.16, 17 Prior literature reports the differentiation between small full-thickness tears and partial-thickness tears on MRI to be challenging. The current study supports the results of prior literature with 71.4% (5 of 7) of operative cases accurately reporting preoperative findings of RC lesions on MRI. Significantly, only 40% (2 of 5) of preoperative MRIs with RC lesions accurately reported RC lesion type. However, preoperative MRI was accurate in detecting the location, and tendon involvement. Lastly, the majority of RC lesions resulted from overhead throwing motions, consistent with prior literature.6
RC lesions are underreported in pediatric populations with few studies identifying the prevalence and characteristics of the lesions observed. In the adult population, however, RC lesions are commonly investigated with prior literature reporting RC lesions are the most common cause of shoulder complaints in adults, with the majority of tears occurring at the anterior supraspinatus.20, 21, 22, 23, 24, 25, 26 The current study supports prior literature demonstrating 77.8% (7 of 9) of operative cases involved the supraspinatus tendon identified via intraoperative arthroscopy. Consistent with prior literature, the current study also demonstrated 30% of operative RC lesions occurred at the RC footprint.
Prior studies have reported the prevalence and type of RC lesion observed in the pediatric population. Eisner, Roocroft, Moor, Edmonds27 performed a retrospective review examining associated pathology of rotator cuff tears in 53 patients discovered on MRI or arthroscopy who underwent operative and non-operative interventions. Unlike the current study, the authors reported that operative intervention was more commonly observed in females with 21 of 30 (70%) operative cases having associated pathology, most commonly posterior and posterosuperior labral tears. The current study observed operative RC lesions in males, with the most common associated pathology being Bankart lesions and SLAP tears and the minority of associated pathology being posterior labral tears. However, these authors failed to discuss the differences between MRI and arthroscopic findings. Polousky, Harms28 examined RC lesions in 2 patients diagnosed by MRI. Both patients experienced isolated subscapularis tendon injuries which was not observed in any patients in the current study.
In a study of 455 patients published in 2013, Zbojniewicz, Maeder, Emery, Salisbury29 reported 12.2% of patients experienced RC tears identified on MRI, with the supraspinatus involved in 56% of lesions, and the majority of lesions being articular-sided partial-thickness tears29. The results of the current study support these findings, with the majority of lesions (77.8%) involving the supraspinatus tendon, were articular-sided (90%), and were partial-thickness tears (70%). Zbojniewicz, Maeder, Emery, Salisbury29 also reported 36% of RC lesions occurred with a concomitant labral tear. Interestingly, the results of the current study demonstrated a more common association with 70% of RC lesions occurring with a concomitant labral tear. Notably, the cited literature identified RC lesions by MRI, whereas, the current study utilized intraoperative arthroscopic findings to characterize RC lesions. The differences observed between studies may have resulted from the difference in population of patients examined. All patients in the current study underwent operative intervention for RC lesions. In contrast, the prior study may have identified RC lesions in patients who were not symptomatic and did not undergo operative intervention. This may be reflected in the relative increase in severity of injuries with a greater percentage of patients with concomitant labral pathology in the current patient population. There are several limitations to the current study. Firstly, the current study is a retrospective observational study, increasing the potential for selection bias. The risk of selection bias was minimized by including a broad range of CPT codes in the initial procedural search in effort to include all possible shoulder procedures. Secondly, the nature of observational studies limits the evaluation of statistical trends in the population examined. The cohort examined represented a small sample of patients who underwent operative intervention for shoulder pathology, and therefore may not capture RC injuries treated non-operatively. Lastly, all patients underwent operative intervention at a single sports medicine institute, which may not reflect the general pediatric population. Future studies examining a larger, more diverse patient population are necessary to provide more insight into the prevalence and characteristics of RC lesions within this age group.
5. Conclusion
The current study contributes to a small body of literature examining the prevalence and characteristics of RC tears in the pediatric population. Based on the results of the current study, RC lesions may be underreported and/or inaccurately reported among pediatric patients if prevalence rates are based solely on MRI findings. Additionally, pediatric patients with operative RC tears should be expected to have associated injuries, with complete and thorough arthroscopic visualization identifying these injuries, most commonly involving the labrum. RC tears in the pediatric population are most commonly articular-sided, partial-thickness tears of the supraspinatus. Our study supports prior literature and further demonstrates RC lesions resulting from overhead throwing motion may begin as early as childhood.
Funding
The authors have received no funding in the preparation of this manuscript.
Conflict of interest
The authors declare no conflict of interest.
Contributor Information
Jose R. Perez, Email: josep1205@med.miami.edu.
Jean Jose, Email: jjose@med.miami.edu.
Appendix A. CPT Code and Descriptions.*
| CPT Code | Description |
|---|---|
| 23410 | Repair rotator cuff acute |
| 23412 | Repair rotator cuff chronic |
| 23420 | Repair of shoulder |
| 29827 | Arthroscopy rotator cuff repair |
| 29807 | Shoulder arthroscopy/surgery |
| 23550 | Treat clavicle dislocation |
| 23552 | Treat clavicle dislocation |
| 23615 | Treat humerus fracture |
| 23660 | Treat shoulder dislocation |
| 23670 | Treat dislocation/fracture |
| 29805 | Shoulder arthroscopy dx |
| 29806 | Shoulder arthroscopy/surgery |
| 29819 | Shoulder arthroscopy/surgery |
| 29820 | Shoulder arthroscopy/surgery |
| 29821 | Shoulder arthroscopy/surgery |
| 29822 | Shoulder arthroscopy/surgery |
| 29823 | Shoulder arthroscopy/surgery |
| 29824 | Shoulder arthroscopy/surgery |
| 29825 | Shoulder arthroscopy/surgery |
| 29826 | Shoulder arthroscopy/surgery |
| 29827 | Arthroscopy rotator cuff repair |
| 29828 | Arthroscopy biceps tenodesis |
*Information obtained from the CMS.gov Physician Fee Schedule website.
References
- 1.Carvalho C.D., Cohen C., Belangero P.S. Partial rotator cuff injury in athletes: bursal or articular? Revista brasileira de ortopedia. 2015;50:416–421. doi: 10.1016/j.rboe.2015.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Alley M.C., Banerjee S., Papaliodis D., Tsitos K., Zanaros G.S. Transosseous physeal-sparing rotator cuff repair in an adolescent football player. Orthopedics. 2016;39:e353–358. doi: 10.3928/01477447-20160129-06. [DOI] [PubMed] [Google Scholar]
- 3.Fukuda H. Partial-thickness rotator cuff tears: a modern view on Codman's classic. J Shoulder Elbow Surg. 2000;9:163–168. [PubMed] [Google Scholar]
- 4.Bryant L., Shnier R., Bryant C., Murrell G.A. A comparison of clinical estimation, ultrasonography, magnetic resonance imaging, and arthroscopy in determining the size of rotator cuff tears. J Shoulder Elbow Surg. 2002;11:219–224. doi: 10.1067/mse.2002.121923. [DOI] [PubMed] [Google Scholar]
- 5.Brownlow H.C., Smith C., Corner T., Neen D., Pennington R. Pain and stiffness in partial-thickness rotator cuff tears. Am J Orthop (Belle Mead NJ) 2009;38:338–340. [PubMed] [Google Scholar]
- 6.Brockmeier S.F., Dodson C.C., Gamradt S.C., Coleman S.H., Altchek D.W. Arthroscopic intratendinous repair of the delaminated partial-thickness rotator cuff tear in overhead athletes. Arthroscopy. 2008;24:961–965. doi: 10.1016/j.arthro.2007.08.016. [DOI] [PubMed] [Google Scholar]
- 7.Schaeffeler C., Mueller D., Kirchhoff C., Wolf P., Rummeny E.J., Woertler K. Tears at the rotator cuff footprint: prevalence and imaging characteristics in 305 MR arthrograms of the shoulder. Eur Radiol. 2011;21:1477–1484. doi: 10.1007/s00330-011-2066-x. [DOI] [PubMed] [Google Scholar]
- 8.Snyder S. Shoulder Arthroscopy. Lippincott Williams & Wilkins; Philadelphia: 2003. Arthroscopic repair of partial articular supraspinatus tendon avulsions: PASTA lesions of the rotator cuff tendon; pp. 219–229. [Google Scholar]
- 9.Cools A.M., Palmans T., Johansson F.R. Age-related, sport-specific adaptions of the shoulder girdle in elite adolescent tennis players. J Athl Train. 2014;49:647–653. doi: 10.4085/1062-6050-49.3.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kim H.M., Dahiya N., Teefey S.A. Location and initiation of degenerative rotator cuff tears: an analysis of three hundred and sixty shoulders. J Bone Joint Surg Am. 2010;92:1088–1096. doi: 10.2106/JBJS.I.00686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fukuda H. The management of partial-thickness tears of the rotator cuff. J Bone Joint Surg Br. 2003;85:3–11. doi: 10.1302/0301-620x.85b1.13846. [DOI] [PubMed] [Google Scholar]
- 12.Codman E.A. Thomas Todd Company; 1934. The Shoulder: Rupture of the Supraspinatus Tendon and Other Lesions in or About the Subacromial Bursa. [Google Scholar]
- 13.DeFranco M.J., Cole B.J. Current perspectives on rotator cuff anatomy. Arthroscopy. 2009;25:305–320. doi: 10.1016/j.arthro.2008.07.023. [DOI] [PubMed] [Google Scholar]
- 14.Itoi E., Tabata S. Rotator cuff tears in the adolescent. Orthopedics. 1993;16:78–81. doi: 10.3928/0147-7447-19930101-13. [DOI] [PubMed] [Google Scholar]
- 15.Darrow C.J., Collins C.L., Yard E.E., Comstock R.D. Epidemiology of severe injuries among United States high school athletes: 2005–2007. Am J Sports Med. 2009;37:1798–1805. doi: 10.1177/0363546509333015. [DOI] [PubMed] [Google Scholar]
- 16.Kaplan L.D., McMahon P.J., Towers J., Irrgang J.J., Rodosky M.W. Internal impingement: findings on magnetic resonance imaging and arthroscopic evaluation. Arthroscopy: J Arthroscopic Relat. Surg. Off. Pub. Arthroscopy Association North America Int. Arthroscopy Assoc. 2004;20:701–704. doi: 10.1016/j.arthro.2004.06.006. [DOI] [PubMed] [Google Scholar]
- 17.Ilozue T., Fotiadou A., Amarah S. Evaluating the success of preoperative imaging for diagnosing rotator cuff tears in a regional centre. Acta Orthop Belg. 2014;80:322–330. [PubMed] [Google Scholar]
- 18.Dilisio M.F., Noel C.R., Noble J.S., Bell R.H. Traumatic supraspinatus tears in patients younger than 25 years. Orthopedics. 2015;38:e631–634. doi: 10.3928/01477447-20150701-63. [DOI] [PubMed] [Google Scholar]
- 19.Yamakawa S., Hashizume H., Ichikawa N., Itadera E., Inoue H. Comparative studies of MRI and operative findings in rotator cuff tear. Acta Med Okayama. 2001;55:261–268. doi: 10.18926/AMO/32019. [DOI] [PubMed] [Google Scholar]
- 20.Battaglia T.C., Barr M.A., Diduch D.R. Rotator cuff tear in a 13-year-old baseball player: a case report. Am J Sports Med. 2003;31:779–782. doi: 10.1177/03635465030310052401. [DOI] [PubMed] [Google Scholar]
- 21.Tarkin I.S., Morganti C.M., Zillmer D.A., McFarland E.G., Giangarra C.E. Rotator cuff tears in adolescent athletes. Am J Sports Med. 2005;33:596–601. doi: 10.1177/0363546504269033. [DOI] [PubMed] [Google Scholar]
- 22.Burns T.C., Reineck J.R., Krishnan S.G. Rotator cuff tears in adolescent female catchers. J Shoulder Elbow Surg. 2009;18:e13–16. doi: 10.1016/j.jse.2009.02.017. [DOI] [PubMed] [Google Scholar]
- 23.Edmonds E.W., Roocroft J.H., Parikh S.N. Spectrum of operative childhood intra-articular shoulder pathology. J Child Orthop. 2014;8:337–340. doi: 10.1007/s11832-014-0598-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mitchell C., Adebajo A., Hay E., Carr A. Shoulder pain: diagnosis and management in primary care. BMJ. 2005;331:1124–1128. doi: 10.1136/bmj.331.7525.1124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Macfarlane G.J., Hunt I.M., Silman A.J. Predictors of chronic shoulder pain: a population based prospective study. J Rheumatol. 1998;25:1612–1615. [PubMed] [Google Scholar]
- 26.Opsha O., Malik A., Baltazar R. MRI of the rotator cuff and internal derangement. Eur J Radiol. 2008;68:36–56. doi: 10.1016/j.ejrad.2008.02.018. [DOI] [PubMed] [Google Scholar]
- 27.Eisner E.A., Roocroft J.H., Moor M.A., Edmonds E.W. Partial rotator cuff tears in adolescents: factors affecting outcomes. J Pediatr Orthop. 2013;33:2–7. doi: 10.1097/BPO.0b013e318279c2e0. [DOI] [PubMed] [Google Scholar]
- 28.Polousky J.D., Harms S. Subscapularis tendon injuries in adolescents: a report of 2 cases. J Pediatr Orthop. 2011;31:e57–59. doi: 10.1097/BPO.0b013e31821f92ca. [DOI] [PubMed] [Google Scholar]
- 29.Zbojniewicz A.M., Maeder M.E., Emery K.H., Salisbury S.R. Rotator cuff tears in children and adolescents: experience at a large pediatric hospital. Pediatr Radiol. 2014;44:729–737. doi: 10.1007/s00247-014-2875-6. [DOI] [PubMed] [Google Scholar]