Abstract
Aim
We examined ethnicity-related differences in the uptake of a temporary free-of-charge HPV vaccine (HPVV) catch-up programme offered in Denmark from August 2012 to December 2013 to women born from 1985–1992 and compared it with the previous self-payment system in place.
Methods
We conducted a nationwide retrospective cohort study. We performed logistic regression analyses to examine the relationship between ethnic background and HPV vaccine (HPVV) programme initiation.
Results
The free programme increased the vaccination uptake from 16% to 75%. Descendants (Denmark-born women with both parents of foreign origin) and immigrants in Denmark for more than 5 years were less likely to initiate the free HPVV programme than Denmark-born women ((aOR=0.56; 95% CI: 0.54–0.59) and (aOR=0.39; 95% CI: 0.38–0.40), respectively). The likelihood of HPVV programme initiation among immigrants increased with time in Denmark ((aOR=2.28; 95% CI: 2.11–2.48) for immigrants living in Denmark for 16–20 years compared to 6–10 years)).
Conclusion
The initiation of the free-of-charge HPVV programme was satisfactory. However, large differences in uptake were demonstrated, indicating that some target groups are harder to reach than others. The integration process (as related to use of health services) occurs over many years where differences between the different population groups seem to vanish.
Keywords: HPV, Human papillomavirus, Vaccine, Uptake, Ethnic background, Initiation
1. Introduction
Between 2006 and 2013, two HPV vaccines (HPVV) have been licensed globally, aimed at preventing cervical cancer: Cervarix®, a bivalent vaccine that targets papillomavirus 16 and 18, and Gardasil®, which additionally targets papillomavirus 6 and 11 [1]. Additionally, a nine-valent vaccine that targets five additional papillomavirus (types 31,33,45,52,53) has been licensed by EMA in 2015 [2] and by FDA in 2014 [3]. WHO considers girls aged 9–13 years as the primary target group (routine group) to receive the HPVV [4]. Some vaccination programmes target women up to 26 years of age [5]. The highest rates of genital HPV infection are found in women from 18 to 28 years of age [6]. Targeting additionally older catch-up groups contributes to achieve higher coverage rates and to accelerating the benefits of the vaccine. Moreover, some countries experience higher HPVV coverage rates among catch-up than among routine groups [7].
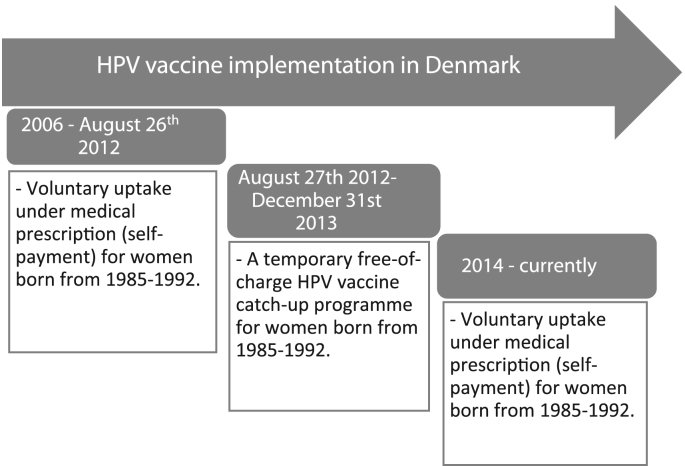
Gardasil® was introduced into the Danish standard childhood vaccination programme in January 2009, aimed at girls aged 12 years. Additionally, a catch-up programme for girls aged 13–15 years had been in place lasting from October 2008 to the end of 2010 [8]. High general public support for introducing the HPVV in Denmark, in particular from organisations such as the Danish Cancer Society, resulted in the decision to also include women between the ages of 19 and 28 years in a cost-free catch-up programme lasting from 27 August 2012 to 31 December 2013 [9] (Fig. 1).
Fig. 1.
Timeline for HPV vaccination programme implementation in Denmark for women born in 1985–1992.
This study focuses primarily on HPVV programme initiation during this cost-free catch-up programme in the cohort of women born between 1985 and 1992, and in particular on the role of ethnic background as a determinant of HPVV programme initiation. We have this particular focus as the literature suggests that ethnic background influences HPVV uptake [10], [11], [12], [13], [14], [15]. In Denmark, two studies based on a cohort of girls born in 1996 [16] and 1996–1997 [17] respectively, revealed that ethnic Danish girls had a higher HPV routine vaccination uptake than Non-Danes. Since Denmark is a country with large ethnic minorities and immigrant populations, an analysis is relevant in order to determine differences in HPV vaccination by ethnic background also among older cohorts. Second, we compared this programme with the previous self-payment system in place to assess whether the free-of-charge catch-up programme had a particular effect on HPVV programme initiation in specific ethnic groups, i.e. if the introduction of a free-of-charge programme resulted in a different ethnic HPVV initiation profile when compared to initiation levels prior to the programme, when the vaccination was subject to a self-payment of approximately 1350DKK/181€ per dose. This study provides the first comprehensive analysis of ethnicity-related differences in HPV vaccination in a large cohort of women in Denmark born from 1985 to 1992.
2. Methods
2.1. Data sources
We used the Danish Vaccination Registry (DDV) to conduct a nationwide retrospective cohort study. Vaccination data and socio-demographic variables were linked through the civil registration number. All citizens residing in Denmark are registered with a unique personal identifier (CPR-number), where individual information such as name, gender, date of birth, vital status, country of birth, citizenship and address is registered.
2.2. Study period
The temporary free-of-charge HPVV catch-up programme was offered from August 27th 2012 to December 31st 2013 to all women born from 1985 to 1992 and registered as citizens in Denmark. The CPR-registry data was last updated in June 27th 2013, six months before the catch-up programme concluded. Therefore, women arriving in Denmark after this date were not included in this study.
2.3. Outcome variable
The outcome under study was the uptake of the first dose of the HPVV (HPV1) during the temporary free-of-charge catch up programme among the cohort of women born from 1985 to 1992, as well as prior to it, i.e. HPV1 uptake when the vaccine was medically prescribed and subject to self-payment.
For the purpose of this study, only HPV vaccination initiation, measured as the uptake of the first HPVV dose out of the three scheduled, was examined.
Data on HPV vaccines administered outside Denmark were not available, the result being that women who have initiated the vaccination programme outside Denmark were registered as non-vaccinated. While this is not assumed to be a major concern for most of the population under study, it is possible that there is an overrepresentation of these cases among immigrants on short-term stays in Denmark (e.g. students), particularly if they have a similar level of access to the vaccine in their home countries. Therefore, women living in Denmark for less than 6 years from the end of the free-of-charge vaccination programme were removed from the logistic regression models, assuming that the number of women in this age group vaccinated against HPV by December 31st 2007 in their countries of origin is low.
2.4. Predictor variables
The variables under study were all socio-demographic variables registered in the CPR-registry that either provide a measure of ethnicity or are shown to be related to the uptake of the HPVV [10], [16], [18], [19], [20], [21], [22], [23], [24].
2.4.1. Main predictor variable
-
•
Ethnic background, categorised into four groups according to women’ and parents’ country of origin: Denmark-born women with both parents Denmark-born, Denmark-born women with one parent Denmark-born, Denmark-born women with both parents of foreign origin (descendants) and women of foreign origin (immigrants). For descendants, further divisions were made by grouping women according to parents’ region/country of origin. Immigrants were also further categorized according to their region/country of origin.
Countries with a representative population of 800 women or more were categorized independently, and countries with smaller populations were grouped together according to region of origin.
2.4.2. Other predictor variables (control variables)
-
•
Year of birth: women were categorized in eight groups by year of birth, from 1985 to 1992.
-
•
Civil status: Women were divided into two categories: Married, which includes married women and women in a registered partnership, and not married, which accounts for single, divorced, widows and women whose registered partnership finished.
-
•
Area of residence: based on their address, the women were grouped in eleven specific areas of residence in Denmark.
-
•
Years lived in Denmark: The years spent in Denmark were grouped in periods of five years, except from the last category in which 8 years were grouped together (6–10 years, 11–15 years, 16–20, 21–28 years).
2.5. Statistical analysis
First, descriptive analyses were conducted to calculate HPVV initiation both during and before the launch of the free-of-charge catch-up programme. Then, univariable logistic regression was performed to investigate any association between each of the socio-demographic variables and HPV1 uptake. Variables displaying significance in the univariable analysis were included in the multivariable model and logistic regression was conducted. All data cleaning, management and analysis were done using the statistical software package STATA 12.
2.6. Ethical considerations
No ethical approval was needed for this study since it is a register based study and thus does not involve human subjects or human biological material such as tissue, ovums or cells [25]. The study was notified to the Danish data protection agency under the record number 2008-54-0474.
3. Results
A total of 274,154 women born from 1985 to 1992 were registered in the CPR-system until June 27th 2013. Of these, 44,122 women had already initiated the HPV vaccination programme before the free-of-charge programme was launched, i.e. when it was subject to self-payment, representing a 16.1% of the total population. Subsequently, the remaining 230,032 women born between 1985 and 1992 could have initiated the free-of-charge HPVV programme. Of these, 158,380 (68.9%) were ethnic Danish women with both parents Denmark-born, 13,957 (6.1%) were ethnic Danish women with one parent Denmark-born, 9314 (4.0%) were Denmark-born women of foreign descent (descendants) and immigrant women represented one fifth (20.8%) of the cohort under study (47,790 out of 230,032 women).
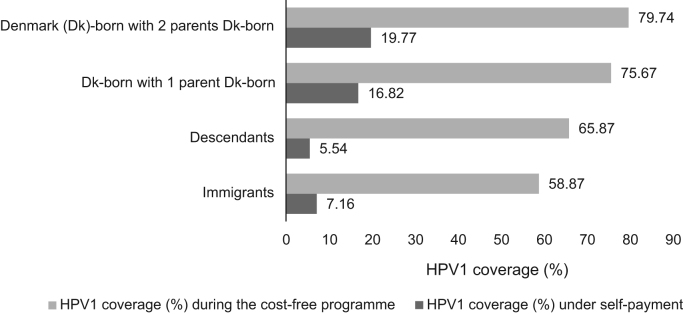
In terms of ethnic background, Denmark-born women with both parents Denmark-born had the highest HPV1 uptake (79.7%) in the free-of-charge HPVV programme, followed by Denmark-born women with one Denmark-born parent (75.7%), and descendants (65.9%). Meanwhile, overall HPV1 uptake was lower among immigrants (39.0%), being around half of the uptake among ethnic Danes. After excluding the immigrant population living in Denmark for less than six years from the end of the free-of-charge programme, the uptake of HPV1 in this group was 58.9%. Fig. 2 shows the HPV1 coverage during the free-of-charge programme and prior to it (subject to self-payment) in the main populations in the cohort after excluding immigrants in Denmark for less than six years from December 31st 2013.
Fig. 2.
HPV1 coverage by population group. The immigrant population living in Denmark for less than 6 years has been excluded.
A descriptive overview of HPV1 coverage in the whole cohort (N=274,154) before and after the introduction of the cost-free programme showed that the launch of the temporary free-of-charge catch-up programme served to raise total HPV1 coverage from 16.0% to 75.1%, and to decrease the relative difference in uptake between ethnic Danish women and non-Danish women for most of the minority groups. Descendants and immigrants constituted the low-uptake groups prior to the programme. With the introduction of the programme, there was a 12-fold increase in uptake percentage among descendants and an 11-fold increase in uptake percentage among immigrants. In comparison, a relatively smaller four-fold increase was observed for Denmark-born women with two parents Denmark-born, while there was a five-fold increase among Denmark-born women with one parent Denmark-born. If immigrants in Denmark for less than 6 years were excluded, total HPV1 coverage raised from 17.8% to 80.7%, and there was an 8-fold increase in uptake percentage among immigrants. Although HPV1 coverage for some low-uptake groups still remained low, the introduction of the free-of charge programme contributed to lift coverage among these groups, creating a slightly more equal total coverage profile. (Table 1).
Table 1.
Impact of the free-of-charge HPV vaccination programme in the main descendant and immigrant populations under study. Descriptive results for HPV1 uptake percentage before (vaccine subject to self-payment), during the free-of-charge programme, and in total.
| Variables |
Vaccination coverage in the whole cohort (%) |
Vaccination coverage in the cohort after excluding the immigrant population living in Denmark for less than 6 years (%) |
||||||
|---|---|---|---|---|---|---|---|---|
| N | HPV1 | HPV1 | HPV1 | N | HPV1 | HPV1 | HPV1 | |
| (Before) | (Programmea) | (Total) | (Before) | (Programmea) | (Total) | |||
| Number of doses/total population | 44,122/274,154 | 161,819/230,032 | 205,941/274,154 | 44,045/247,381 | 155,613/203,336 | 199,658/247,381 | ||
| Country of origin | ||||||||
| Denmark (Dk)- born w 2 parents Dk-born | 197,415 | 19.8 | 79.7 | 83.7 | (Same numbers as vaccination coverage in the column for the whole cohort. See left side of the table) | |||
| Dk-born w one parent Dk-born | 16,780 | 16.8 | 75.7 | 79.8 | ||||
| Descendantsb | 9860 | 5.5 | 65.9 | 67.7 | ||||
| Turkey | 3469 | 4.6 | 61.8 | 67.1 | ||||
| Pakistan | 1014 | 2.0 | 57.8 | 58.6 | ||||
| Lebanon | 956 | 3.4 | 65.6 | 63.1 | ||||
| Immigrants | 49,495 | 3.4 | 39.0 | 41.1 | 22,722 | 7.16 | 58.87 | 61.82 |
| Norway | 2572 | 3.5 | 55.3 | 56.9 | 802 | 10.4 | 67.7 | 71.1 |
| Sweden | 1655 | 4.9 | 51.6 | 54.0 | 761 | 9.7 | 63.9 | 67.4 |
| Faroe Islands | 1349 | 4.5 | 72.7 | 73.9 | 767 | 6.8 | 75.4 | 77.1 |
| Greenland | 1020 | 6.6 | 63.3 | 65.7 | 993 | 6.3 | 63.1 | 65.5 |
| Germany | 2394 | 3.3 | 24.5 | 26.9 | 900 | 8.6 | 48.9 | 53.2 |
| Spain | 895 | 2.0 | 15.3 | 17.0 | 137 | 13.1 | 44.5 | 51.8 |
| France | 832 | 3.3 | 11.8 | 14.7 | 168 | 14.9 | 40.6 | 49.4 |
| USA | 1,04 | 7.1 | 21.8 | 27.4 | 387 | 18.4 | 51.0 | 60.0 |
| Poland | 2817 | 0.9 | 26.7 | 27.3 | 847 | 2.6 | 42.2 | 43.7 |
| Rumania | 2372 | 1.0 | 18.2 | 19.0 | 338 | 6.5 | 40.5 | 44.4 |
| Lithuania | 1624 | 0.6 | 22.4 | 22.8 | 298 | 2.7 | 41.0 | 42.6 |
| Bosnia-Herzegovina | 1394 | 6.1 | 67.0 | 69.0 | 1321 | 6.4 | 69.2 | 71.2 |
| Latvia | 814 | 0.9 | 22.7 | 23.3 | 133 | 2.3 | 39.2 | 40.6 |
| Ukraine | 1183 | 0.9 | 23.6 | 24.2 | 300 | 3.7 | 45.3 | 47.3 |
| The Philippines | 2554 | 0.5 | 25.7 | 26.0 | 291 | 3.4 | 57.3 | 58.8 |
| China | 1358 | 1.6 | 40.0 | 41.0 | 497 | 4.0 | 56.4 | 58.2 |
| South Korea | 980 | 17.1 | 70.8 | 75.8 | 848 | 19.5 | 80.1 | 84.0 |
| India | 851 | 12.8 | 50.5 | 56.9 | 498 | 21.7 | 79.2 | 83.7 |
| Iraq | 1692 | 1.3 | 55.2 | 55.8 | 1565 | 1.4 | 56.8 | 57.4 |
| Afghanistan | 1220 | 1.6 | 65.4 | 65.9 | 1006 | 1.9 | 68.3 | 68.9 |
| Turkey | 1076 | 2.0 | 40.3 | 41.5 | 721 | 2.8 | 48.9 | 50.4 |
| Somalia | 959 | 0.4 | 31.6 | 31.9 | 811 | 0.5 | 34.9 | 35.3 |
Vaccination coverage during the the free-of-charge programme (27/08/2012 to 31/12/2013) after removing from the total population every woman that received any dose of the vaccine prior to the free-of-charge programme.
Descendants: Denmark-born women with both parents Denmark-born.
Table 2 shows crude and adjusted results for the association between region of origin and the initiation of the free-of-charge programme. Descendants from East Asia were the most likely to initiate the programme, the likelihood being higher than for the reference group (Denmark-born women with two parents Denmark-born). Descendants with origin in Central-Eastern Europe were more likely than descendants of the MENA-PAT (Middle-East, North-Africa, Pakistan, Afghanistan and Turkey) region to start the programme. Immigrants from the Indian Subcontinent, other Nordic countries and East Asia were the most likely to initiate the HPVV programme, whereas immigrants from Oceania, North America and Sub-Saharan Africa were the least likely. (Table 2).
Table 2.
Association between region of origin and free-of-charge HPV vaccine programme initiation after removing from the model the immigrant population living in Denmark for less than 6 years.
| Variables | Vaccination initiation | Vaccination initiation | ||||||
|---|---|---|---|---|---|---|---|---|
|
CRUDE |
ADJUSTEDa |
|||||||
| Odds Ratio | P-value | [95% Conf. | Interval] | Odds Ratio | P-value | [95% Conf. | Interval] | |
| Region of origin | ||||||||
| Denmark (Dk)-born w 2 parents Dk-born | Ref. | Ref. | ||||||
| Dk-born w one parent Dk-born | 0.79 | <0.0001 | 0.76 | 0.82 | 0.83 | <0.0001 | 0.80 | 0.87 |
| Descendants | ||||||||
| Other Nordic countries | 0.76 | 0.131 | 0.53 | 1.086 | 0.84 | 0.361 | 0.59 | 1.21 |
| Greenland | 0.20 | 0.001 | 0.08 | 0.52 | 0.20 | 0.001 | 0.08 | 0.52 |
| Other West. Eur. Countries | 0.46 | <0.0001 | 0.33 | 0.65 | 0.49 | <0.0001 | 0.35 | 0.69 |
| North America | – | – | – | – | – | – | – | – |
| Oceania | – | – | – | – | – | – | – | – |
| Central Eastern Eur, | 0.54 | <0.0001 | 0.46 | 0.62 | 0.63 | <0.0001 | 0.54 | 0.73 |
| Former USSR | 0.25 | 0.093 | 0.05 | 1.26 | 0.30 | 0.138 | 0.06 | 1.47 |
| Lat. Amer. & Caribb. | 1.52 | 0.435 | 0.53 | 4.40 | 1.81 | 0.274 | 0.63 | 5.22 |
| East Asia | 1.37 | 0.012 | 1 | 1.76 | 1.47 | 0.002 | 1.15 | 1.88 |
| Indian Subcontinent | 0.76 | 0.013 | 0.61 | 0.94 | 0.75 | 0.013 | 0.60 | 0.94 |
| MENA-PATb | 0.44 | <0.0001 | 0.42 | 0.46 | 0.51 | <0.0001 | 0.48 | 0.54 |
| Sub-Saharan Africa | 0.53 | <0.0001 | 0.38 | 0.73 | 0.61 | 0.003 | 0.44 | 0.85 |
| Immigrants | ||||||||
| Other Nordic Countries | 0.55 | <0.0001 | 0.51 | 0.60 | 0.60 | <0.0001 | 0.55 | 0.65 |
| Greenland | 0.43 | <0.0001 | 0.38 | 0.50 | 0.43 | <0.0001 | 0.37 | 0.49 |
| Other West. Eur. Countries | 0.29 | <0.0001 | 0.27 | 0.32 | 0.30 | <0.0001 | 0.28 | 0.33 |
| North America | 0.24 | <0.0001 | 0.20 | 0.29 | 0.26 | <0.0001 | 0.21 | 0.32 |
| Oceania | 0.12 | <0.0001 | 0.08 | 0.16 | 0.12 | <0.0001 | 0.09 | 0.17 |
| Central and East. Eur. | 0.30 | <0.0001 | 0.28 | 0.32 | 0.31 | <0.0001 | 0.29 | 0.33 |
| Former USSR | 0.28 | <0.0001 | 0.24 | 0.32 | 0.31 | <0.0001 | 0.27 | 0.36 |
| Latin America & Carib. | 0.48 | <0.0001 | 0.41 | 0.57 | 0.51 | <0.0001 | 0.43 | 0.60 |
| East Asia | 0.52 | <0.0001 | 0.47 | 0.56 | 0.56 | <0.0001 | 0.52 | 0.61 |
| Indian Subcontinent | 0.64 | <0.0001 | 0.55 | 0.75 | 0.68 | <0.0001 | 0.58 | 0.80 |
| MENA-PATb | 0.35 | <0.0001 | 0.33 | 0.37 | 0.38 | <0.0001 | 0.36 | 0.40 |
| Sub-Saharan Africa | 0.26 | <0.0001 | 0.24 | 0.28 | 0.27 | <0.0001 | 0.25 | 0.30 |
Adjusted for year of birth, civil status and area of residence in Denmark (Number of observations in the model=202,159).
MENA-PAT=Middle-East North-Africa-Pakistan, Afghanistan and Turkey.
HPV1 coverage was higher among immigrants who have lived in Denmark for a greater number of years. For instance, HPV1 coverage was 69.6% for immigrants living in Denmark for 21–28 years, 65.3% for immigrants in Denmark for 16–20 years, and 59.3% and 43.2% for immigrants in Denmark for 11–15 years and 6–10 years, respectively. Similarly, immigrants living in Denmark for longer periods of time were the most likely to initiate the HPVV programme (aOR=2.88; 95% CI: 2.67–3.12 for those who have lived in Denmark for 21–28 years compared to those living in the country for 6–10 years, which form the reference group). Immigrants living in Denmark for 16–20 years were more than twice as likely to initiate the free-of-charge programme as the reference group, and immigrants in Denmark for 11–15 years were also more likely than the reference group to initiate it (aOR=1.77; 95% CI: 1.63–1.93).
Comparing adjusted likelihoods of initiating the HPVV programme prior to and during the free-of-charge catch-up programme, a considerable increase in vaccination likelihood was seen, relative to ethnic Danes, for women of most countries in the free-of-charge programme (Table 3). This is particularly the case for descendants from Pakistan and Lebanon, and for immigrants from Afghanistan, Somalia and Iraq. At the same time, no clear increase relative to ethnic Danes was seen among immigrants from other Western European countries or the USA.
Table 3.
Association between country of origin and HPV vaccine programme initiation both before (subject to self-payment) and during the free-of-charge programme after excluding the immigrant population living in Denmark for less than 6 years.
| Variables | Vaccination initiation | Vaccination initiation | ||||||
|---|---|---|---|---|---|---|---|---|
| ADJUSTEDa | ADJUSTEDa | |||||||
|
(SELF-PAYMENTb) |
(FREE PROGRAMMEc) |
|||||||
| Odds Ratio | P-value | [95% Conf. | Interval] | Odds Ratio | P-value | [95%Conf. | Interval] | |
| Country of origin | ||||||||
| Denmark (Dk)-born with 2 parents Dk-born | Ref. | Ref. | ||||||
| Dk-born with 1 parent Dk-born | 0.72 | <0.0001 | 0.69 | 0.75 | 0.83 | <0.0001 | 0.80 | 0.87 |
| Descendants | ||||||||
| Turkey | 0.19 | <0.0001 | 0.16 | 0.22 | 0.56 | <0.0001 | 0.52 | 0.60 |
| Pakistan | 0.06 | <0.0001 | 0.04 | 0.10 | 0.44 | <0.0001 | 0.38 | 0.50 |
| Lebanon | 0.10 | <0.0001 | 0.07 | 0.14 | 0.44 | <0.0001 | 0.38 | 0.50 |
| Immigrants | ||||||||
| Norway | 0.48 | <0.0001 | 0.38 | 0.61 | 0.58 | <0.0001 | 0.49 | 0.67 |
| Sweden | 0.42 | <0.0001 | 0.33 | 0.54 | 0.49 | <0.0001 | 0.42 | 0.58 |
| Faroe Islands | 0.31 | <0.0001 | 0.23 | 0.41 | 0.83 | 0.031 | 0.70 | 0.98 |
| Greenland | 0.28 | <0.0001 | 0.21 | 0.36 | 0.43 | <0.0001 | 0.37 | 0.49 |
| Germany | 0.41 | <0.0001 | 0.32 | 0.52 | 0.24 | <0.0001 | 0.21 | 0.28 |
| Spain | 0.60 | 0.05 | 0.36 | 1.00 | 0.23 | <0.0001 | 0.16 | 0.33 |
| France | 0.60 | 0.024 | 0.39 | 0.93 | 0.20 | <0.0001 | 0.14 | 0.28 |
| USA | 0.78 | 0.067 | 0.60 | 1.02 | 0.29 | <0.0001 | 0.23 | 0.36 |
| Poland | 0.15 | <0.0001 | 0.10 | 0.23 | 0.20 | <0.0001 | 0.17 | 0.23 |
| Rumania | 0.39 | <0.0001 | 0.25 | 0.61 | 0.18 | <0.0001 | 0.14 | 0.22 |
| Lithuania | 0.15 | <0.0001 | 0.07 | 0.29 | 0.19 | <0.0001 | 0.15 | 0.24 |
| Bosnia-Herzegovina | 0.31 | <0.0001 | 0.24 | 0.38 | 0.57 | <0.0001 | 0.51 | 0.65 |
| Latvia | 0.12 | <0.0001 | 0.04 | 0.38 | 0.17 | <0.0001 | 0.12 | 0.25 |
| Ukraine | 0.27 | <0.0001 | 0.15 | 0.50 | 0.23 | <0.0001 | 0.18 | 0.30 |
| The Philippines | 0.17 | <0.0001 | 0.09 | 0.32 | 0.39 | <0.0001 | 0.31 | 0.50 |
| China | 0.21 | <0.0001 | 0.13 | 0.32 | 0.40 | <0.0001 | 0.33 | 0.48 |
| South Korea | 1.15 | 0.117 | 0.97 | 1.37 | 1.08 | 0.426 | 0.89 | 1.30 |
| India | 1.20 | 0.10 | 0.97 | 1.50 | 1.00 | 0.999 | 0.78 | 1.28 |
| Iraq | 0.06 | <0.0001 | 0.04 | 0.09 | 0.35 | <0.0001 | 0.32 | 0.39 |
| Afghanistan | 0.07 | <0.0001 | 0.05 | 0.12 | 0.56 | <0.0001 | 0.49 | 0.64 |
| Turkey | 0.17 | <0.0001 | 0.11 | 0.26 | 0.29 | <0.0001 | 0.25 | 0.34 |
| Somalia | 0.02 | <0.0001 | 0.01 | 0.05 | 0.14 | <0.0001 | 0.12 | 0.16 |
Adjusted for year of birth, civil status and area of residence in Denmark
Number of observations in the model=234,023
Number of observations in the model=190,974
4. Discussion
4.1. Main findings
Ethnic Danish women were the most likely group to initiate the HPVV programme. Overall, there was significant variation in HPVV programme initiation among descendant and immigrants from different regions and countries, both during and prior to the cost-free programme. The number of years lived in Denmark was found to be a determinant of HPVV initiation likelihood among immigrants, with a greater number of years associated with higher likelihood of starting the programme. Finally, it was found that while descendants and immigrants remained less likely than ethnic Danes to start HPVV programme also during the cost-free programme, the introduction of the programme contributed to a relatively greater lift in coverage among these groups.
4.2. Findings in relation to other studies
Our results are in accordance with a number of published studies showing that the majority ethnic population of a country is more likely to initiate a HPVV programme than minority groups in the same country [10], [11], [12], [14], [16], [26]. Beyond ethno-cultural reasons for non-participation that might affect ethnic majority and minority population to a greater or lesser extent, ethnic minorities face specific barriers compared to ethnic Danish groups. For instance, immigrants may be unfamiliar with the Danish healthcare system and may face a language barrier in the access to medical services [24]. A study conducted in the Netherlands [27] revealed, additionally, that communication between general practitioners and immigrants was different compared to communication with the ethnic majority population; the time of communication was shorter, with a verbal predominance of the doctor over the patient, and a poor mutual understanding often leading to a less demanding patient and lower compliance. In addition, differences in HPVV programme participation among the immigrant population might be partly explained by the reasons for migration. Denmark hosts a great number of workers from the new European Union member states to work in the construction, consumer industry, agriculture, or cleaning, with potentially lower wages than the Danish average income [28]. This type of migration might affect their possibilities of integration in the country, influencing their knowledge about for instance healthcare services [24], which may explain the low HPVV programme initiation among some of these specific minority populations.
The results in this study reveal that the introduction of the cost-free programme served to markedly increase total HPV1 coverage, especially lifting coverage among certain descendants and immigrants groups. One study [29] analysing equality in the use of healthcare services in Denmark reveal that, in general, non-Western descendants and immigrants are more likely than ethnic Danes to use free-of-charge healthcare services. However, reduced likelihoods among them are seen when it comes to visiting the dentist, which in Denmark requires co-payment, despite adjusting for the effect of socio-economic status [29]. This may be seen to indicate a low willingness among immigrants and descendants to pay for medical services and can be interpreted to explain why the introduction of a cost-free HPVV programme in particular had an impact among immigrants and descendants.
4.3. Limitations
Undocumented migrants, refugees and asylum seekers may be at high-risk of non-vaccination. However, they are not included in the register and are therefore not part of the study. As explained above, data on HPVV given outside Denmark were not retrieved. However, this information bias has been minimised by excluding immigrant women that have lived in Denmark for less than six years by the end of the free-of-charge programme. There might be an underreporting of vaccines administered, as general practitioners and private companies are responsible for registering administered vaccines. However, this potential bias is minimized as reimbursement of vaccines is made on the basis of the registration of the vaccine given. In addition, even if there is underreporting, there is no reason to expect that the underreporting should vary across the groups and variables that are compared in this study. The variable socio-economic status is one possibly important variable that is not included due to lack of accessible data.
5. Conclusion
Women with non-Danish background are less likely to initiate the HPVV programme than ethnic Danish women. Large differences in HPVV uptake are seen between different groups of descendants and immigrants across countries and regions. Furthermore, for immigrants, the likelihood of initiating the catch-up programme increases with the number of years lived in Denmark. Overall and for the large majority of groups, the relative difference in first vaccine dose coverage between ethnic Danish women and non-Danish women was smaller following the free-of-charge programme compared to the coverage prior to the self-payment programme. This suggests that a cost-free programme has a positive impact in specific minority populations, helping to overcome a possible economic barrier. However, significant disparities in HPVV uptake remain even after adjusting for the number of years lived in Denmark.
Preventive health, in this case in terms of preventive HPV vaccination, faces challenges that need to be addressed in order to make preventive programmes more efficient from a public health perspective. Ensuring that doctors and patients are able to communicate effectively may be essential to increasing the participation of women in preventive health. Therefore, measures such as increased use of translators or doctors with a similar language and cultural background to large groups of immigrants in a particular area could help to improve participation of hard to reach populations in future vaccination campaigns. However, the cost of such measures in a universal healthcare system can be high, and cost-effectiveness compared to other possible measures should first be analyzed. Furthermore, in order to promote health among all ethnic groups, health intervention should take ethno-cultural differences into consideration. This could include targeted awareness campaigns in areas with a high concentration of ethnic minority women, in media and institutions frequently used by ethnic minorities, and, more generally, the use of posters or other on-line campaign means that visibly promote the idea that health promotion is for all ethnic groups in society.
A future research priority should be to explore how to increase HPVV uptake among specific minority groups, as this study provides a solid indication of the key differences in HPVV initiation between groups and suggests possible explanatory factors. Additionally, conducting a similar quantitative study with relevant socio-economic variables is recommended.
Author contributions
All authors contributed to the conception, design, and drafting of the study. PVB was responsible for acquisition of data. VFC was responsible for the analysis and interpretation of data, and for drafting the article. All authors contributed to the analysis and interpretation of data. All authors revised it critically for important intellectual content. All authors have approved the final version submitted.
Conflict of interest statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgements
We would like to acknowledge Kåre Mølbak (Statens Serum Institut (SSI), Denmark) for his critical review, Susan Cowan (SSI) and Annika Wendland (SSI) for their helpful comments and Jens Nielsen (SSI) for his statistical advice.
Contributor Information
Victoria Fernández de Casadevante, Email: vfcm@ssi.dk.
Lourdes Cantarero-Arévalo, Email: lou.cantarero@sund.ku.dk.
Julita Gil Cuesta, Email: giljulita@gmail.com.
Palle Valentiner-Branth, Email: PVB@ssi.dk.
References
- 1.WHO, Vaccinating against cervical cancer [Internet]. Available from: 〈http://www.who.int/bulletin/volumes/85/2/07-020207/en/〉, [cited 04.03.16].
- 2.European Medicines Agency – Find medicine – Gardasil 9 [Internet]. Available from: 〈http://www.ema.europa.eu/ema/index.jsp?curl=pages/medicines/human/medicines/003852/human_med_001863.jsp&mid=WC0b01ac058001d124〉, [cited 04.03.16].
- 3.Research C for BE and. Approved Products – Gardasil 9 [Internet]. Available from: 〈http://www.fda.gov/BiologicsBloodVaccines/Vaccines/ApprovedProducts/ucm426445.htm〉, [cited 04.03.16].
- 4.WHO Guidance Note: Comprehensive cervical cancer prevention and control: a healthier future for girls and women [Internet]. Available from: 〈http://apps.who.int/iris/bitstream/10665/78128/3/9789241505147_eng.pdf?ua=1〉, [cited 27.11.14].
- 5.CDC – Centers for Disease Control and Prevention, Morbidity and Mortality Weekly Report (MMWR)-Human Papillomavirus Vaccination: Recommendations of the Advisory Committee on Immunization Practices (ACIP) [Internet]. Available from: 〈http://www.cdc.gov/mmwr/preview/mmwrhtml/rr6305a1.htm〉. [PubMed]
- 6.Koutsky L. Epidemiology of genital human papillomavirus infection. Am. J. Med. 1997;102(5A):3–8. doi: 10.1016/s0002-9343(97)00177-0. [DOI] [PubMed] [Google Scholar]
- 7.Bonanni P., Levi M., Latham N.B., Bechini A., Tiscione E., Lai P. An overview on the implementation of HPV vaccination in Europe. Hum. Vaccin. 2011;7(Suppl. 1):S128–S135. doi: 10.4161/hv.7.0.14575. [DOI] [PubMed] [Google Scholar]
- 8.E.F. Dunne, A. Koch, HPV vaccines for circumpolar health: summary of plenary session, “Opportunities for Prevention: Global HPV Vaccine” and “Human Papillomavirus Prevention: The Nordic Experience”, International Journal of Circumpolar Health, [Internet]. Available from: 〈http://www.circumpolarhealthjournal.net/index.php/ijch/article/view/21070〉, [cited 24.11.14], 72(0), 19 June 2013. [DOI] [PMC free article] [PubMed]
- 9.Dorleans F., Giambi C., Dematte L., Cotter S., Stefanoff P., Mereckiene J. The current state of introduction of human papillomavirus vaccination into national immunisation schedules in Europe: first results of the VENICE2 2010 survey. Euro Surveill. 2010;15(47) doi: 10.2807/ese.15.47.19730-en. [DOI] [PubMed] [Google Scholar]
- 10.Rondy M., van Lier A., van de Kassteele J., Rust L., de Melker H. Determinants for HPV vaccine uptake in the Netherlands: a multilevel study. Vaccine. 2010;28(9):2070–2075. doi: 10.1016/j.vaccine.2009.12.042. [DOI] [PubMed] [Google Scholar]
- 11.Fisher H., Audrey S., Mytton J.A., Hickman M., Trotter C. Examining inequalities in the uptake of the school-based HPV vaccination programme in England: a retrospective cohort study. J. Public Health Oxf. Engl. 2014;36(1):36–45. doi: 10.1093/pubmed/fdt042. [DOI] [PubMed] [Google Scholar]
- 12.Spencer A.M., Roberts S.A., Brabin L., Patnick J., Verma A. Sociodemographic factors predicting mother's cervical screening and daughter's HPV vaccination uptake. J. Epidemiol. Community Health. 2014;68(6):571–577. doi: 10.1136/jech-2013-202629. [DOI] [PubMed] [Google Scholar]
- 13.Steens A., Wielders C.C.H., Bogaards J.A., Boshuizen H.C., de Greeff S.C., de Melker H.E. Association between human papillomavirus vaccine uptake and cervical cancer screening in the Netherlands: implications for future impact on prevention. Int. J. Cancer. 2013;132(4):932–943. doi: 10.1002/ijc.27671. [DOI] [PubMed] [Google Scholar]
- 14.Roberts S.A., Brabin L., Stretch R., Baxter D., Elton P., Kitchener H. Human papillomavirus vaccination and social inequality: results from a prospective cohort study. Epidemiol. Infect. 2011;139(3):400–405. doi: 10.1017/S095026881000066X. [DOI] [PubMed] [Google Scholar]
- 15.Fernández de Casadevante V., Gil Cuesta J., Cantarero-Arévalo L. Determinants in the uptake of the human papillomavirus vaccine: a systematic review based on European studies. Front. Oncol. 2015;5:141. doi: 10.3389/fonc.2015.00141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Widgren K., Simonsen J., Valentiner-Branth P., Mølbak K. Uptake of the human papillomavirus-vaccination within the free-of-charge childhood vaccination programme in Denmark. Vaccine. 2011;29(52):9663–9667. doi: 10.1016/j.vaccine.2011.10.021. [DOI] [PubMed] [Google Scholar]
- 17.Slåttelid Schreiber S.M., Juul K.E., Dehlendorff C., Kjær S.K. Socioeconomic predictors of human papillomavirus vaccination among girls in the Danish childhood immunization program. J. Adolesc. Health Off. Publ. Soc. Adolesc. Med. 2015;56(4):402–407. doi: 10.1016/j.jadohealth.2014.12.008. [DOI] [PubMed] [Google Scholar]
- 18.Stöcker P., Dehnert M., Schuster M., Wichmann O., Deleré Y. Human papillomavirus vaccine uptake, knowledge and attitude among 10th grade students in Berlin, Germany, 2010. Hum. Vaccines Immunother. 2013;9(1):74–82. doi: 10.4161/hv.22192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ganry O., Bernin-Mereau A.-S., Gignon M., Merlin-Brochard J., Schmit J.-L. Vol. 61. 2013. Human papillomavirus vaccines in Picardy, France: coverage and correlation with socioeconomic factors; pp. 447–454. (Rev Dépidémiologie Santé Publique). [DOI] [PubMed] [Google Scholar]
- 20.Lefevere E., Hens N., De Smet F., Van Damme P. Dynamics of HPV vaccination initiation in Flanders (Belgium) 2007-2009: a Cox regression model. BMC Public Health. 2011;11:470. doi: 10.1186/1471-2458-11-470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sinka K., Kavanagh K., Gordon R., Love J., Potts A., Donaghy M. Achieving high and equitable coverage of adolescent HPV vaccine in Scotland. J. Epidemiol. Community Health. 2014;68(1):57–63. doi: 10.1136/jech-2013-202620. [DOI] [PubMed] [Google Scholar]
- 22.Rouzier R., Giordanella J.-P. Coverage and compliance of Human Papilloma Virus vaccines in Paris: demonstration of low compliance with non-school-based approaches. J. Adolesc. Health Off. Publ. Soc. Adolesc. Med. 2010;47(3):237–241. doi: 10.1016/j.jadohealth.2010.04.006. [DOI] [PubMed] [Google Scholar]
- 23.Donadiki E.M., Jiménez-García R., Hernández-Barrera V., Carrasco-Garrido P., López de Andrés A., Velonakis E.G. Human papillomavirus vaccination coverage among Greek higher education female students and predictors of vaccine uptake. Vaccine. 2012;30(49):6967–6970. doi: 10.1016/j.vaccine.2012.09.028. [DOI] [PubMed] [Google Scholar]
- 24.Norredam M., Nielsen S.S., Krasnik A. Migrants’ utilization of somatic healthcare services in Europe--a systematic review. Eur. J. Public Health. 2010;20(5):555–563. doi: 10.1093/eurpub/ckp195. [DOI] [PubMed] [Google Scholar]
- 25.Den Nationale Videnskabsetiske Komité [Internet]. Available from: 〈http://www.cvk.sum.dk/〉, [cited 28.11.14].
- 26.Brabin L., Roberts S.A., Stretch R., Baxter D., Chambers G., Kitchener H. Uptake of first two doses of human papillomavirus vaccine by adolescent schoolgirls in Manchester: prospective cohort study. BMJ. 2008;336(7652):1056–1058. doi: 10.1136/bmj.39541.534109.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.van Wieringen J.C.M., Harmsen J.A.M., Bruijnzeels M.A. Intercultural communication in general practice. Eur. J. Public Health. 2002;12(1):63–68. doi: 10.1093/eurpub/12.1.63. [DOI] [PubMed] [Google Scholar]
- 28.Denmark: Integrating Immigrants into a Homogeneous Welfare State | migrationpolicy.org [Internet]. Available from: 〈http://www.migrationpolicy.org/article/denmark-integrating-immigrants-homogeneous-welfare-state〉, [cited 08.12.14].
- 29.Nielsen S.S., Hempler N.F., Waldorff F.B., Kreiner S., Krasnik A. Is there equity in use of healthcare services among immigrants, their descendents, and ethnic Danes? Scand. J. Public Health. 2012;40(3):260–270. doi: 10.1177/1403494812443602. [DOI] [PubMed] [Google Scholar]