Abstract
Background:
The kidney failure risk equation (KFRE) provides an estimate of risk of progression to kidney failure, and may guide clinical care.
Objective:
We aimed to describe patient, family, and health care provider’s perspectives of the perceived benefits and challenges of using a risk-based approach to guide care delivery for patients with advanced chronic kidney disease (CKD), and refine implementation based on their input.
Methods:
We used qualitative methodology to explore perceived benefits and challenges of implementing a risk-based approach (using the KFRE) to determine eligibility for multidisciplinary CKD care in Southern Alberta. We obtained perspectives from patients and families through focus groups, as well as input from health care providers through interviews and open-ended responses from an online survey. Twelve patients/family members participated in 2 focus groups, 16 health care providers participated in an interview, and 40 health care providers responded to the survey.
Results:
Overall, participants felt that a KFRE-based approach had the potential to improve efficiency of the clinics by targeting care to patients at highest risk of kidney failure; however, they also expressed concerns about the impact of loss of services for lower risk individuals. Participants also articulated concerns about a perceived lack of capacity for adequate CKD patient care in the community. Our implementation strategy was modified as a result of participants’ feedback.
Conclusions:
We identified benefits and challenges to implementation of a risk-based approach to guide care of patients with advanced CKD. Based on these results, our implementation strategy has been modified by removing the category of referral back to primary care alone, and instead having that decision made jointly by nephrologists and patients among low-risk patients.
Keywords: chronic kidney disease, kidney failure, kidney failure risk, nondialysis care, qualitative research
Abrégé
Contexte:
La Kidney Failure Risk equation (KFRE), l’équation qui mesure le risque d’évolution vers la défaillance rénale, est susceptible d’orienter les soins prodigués en néphrologie.
Objectifs de l’étude:
Nous souhaitions savoir comment les patients, leurs proches et leurs fournisseurs de soins percevaient le recours à une approche de prédiction du risque pour répartir les patients atteints d’insuffisance rénale chronique (IRC) dans le système de soins. Plus précisément, nous nous sommes intéressés aux avantages et aux défis perçus face à une telle approche, et les commentaires recueillis se destinaient à en raffiner la mise en œuvre.
Méthodologie:
Nous avons utilisé une méthodologie qualitative pour étudier les avantages et les défis perçus de la KFRE comme outil d’évaluation de l’admissibilité de patients sud-albertains atteints d’IRC à la prise en charge par une équipe multidisciplinaire. Les perceptions des patients et de leurs proches ont été recueillies lors de groupes de discussion; les fournisseurs de soins ont quant à eux donné leur avis au moyen d’entrevues et d’un sondage en ligne à questions ouvertes. Au total, douze patients et membres de leurs familles ont participé aux groupes de discussion, 16 fournisseurs des soins ont été interviewés et 40 ont répondu au sondage en ligne.
Résultats:
Dans l’ensemble, les participants étaient d’avis que la KFRE avait le potentiel d’améliorer l’efficience des cliniques en néphrologie en canalisant les soins vers les patients à risque élevé de défaillance rénale. Les participants se sont toutefois dits préoccupés par les éventuelles conséquences d’une perte de services pour les patients à moindre risque. Ils appréhendaient également une capacité insuffisante du milieu communautaire à prendre en charge les patients atteints d’IRC. Nous avons modifié notre stratégie de mise en œuvre suivant les commentaires recueillis.
Conclusion:
Cette étude nous a permis de recenser les avantages et les défis perçus face à l’application d’une approche fondée sur la KFRE pour prodiguer des soins aux patients atteints d’IRC à un stade avancé. À la lumière des résultats, la stratégie de mise en œuvre a été modifiée. Nous avons notamment supprimé la catégorie de renvoi automatique aux seuls soins primaires pour faire en sorte que, dans le cas de patients à faible risque, le mode de prise en charge soit conjointement déterminé par le néphrologue et le patient.
What was known before
Risk prediction tools are used in a variety of clinical settings to guide patient care; however, their use in patients with chronic kidney disease (CKD) is limited. The kidney failure risk equation (KFRE) is being implemented to guide patient care decisions across Southern Alberta. A careful evaluation of patient and provider perceptions, as well as intended and unintended consequences, is needed.
What this adds
Our study provides a qualitative description of patients’, family members’, and providers’ perceived benefits and challenges of implementing a kidney failure risk–based approach to guide care decisions for patients with advanced CKD. This study outlines important considerations, particularly relating to the perceived needs of lower risk CKD patients, including access to preventive education and follow-up, as well as concerns about primary care capacity to manage the complex needs of CKD patients. This study provides a practical approach to evaluating KFRE suitability for multidisciplinary CKD clinics.
Introduction
Chronic kidney disease (CKD) is a significant contributor to morbidity and mortality and affects approximately 12% of adults in Canada.1 Despite effective therapies, studies show that patients with CKD often receive suboptimal care.2 This is in part due to a mismatch between the intensity of care that CKD patients receive compared with what they need, and may result in an overuse of testing and treatments in lower risk patients and an underuse of evidence-based treatments in higher risk patients.2 Identifying patients at highest risk of progression to kidney failure is challenging.3 Although methods to predict CKD and CKD progression have existed for a number of years,4 the recent development5 and validation6 of the 4-variable kidney failure risk equation (KFRE) permits a more accurate assessment of individual risk and, since it is based on routinely collected laboratory data, can be easily incorporated into clinical practice. The KFRE, accessible at www.kidneyfailurerisk.com, has been implemented in a variety of clinical settings.7-9
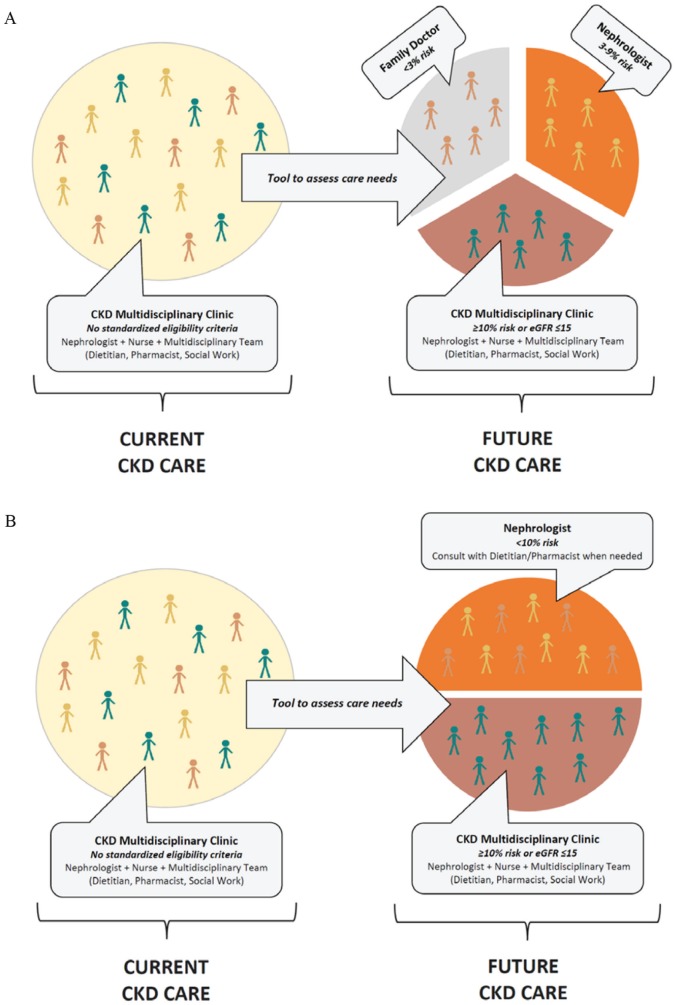
The purpose of this qualitative study was to describe perceived benefits and challenges that may arise following implementation of a KFRE-based approach to guide CKD care delivery in Southern Alberta and modify our implementation strategy if needed. Currently, patients with advanced CKD are cared for in team-based multidisciplinary clinics, involving nephrologists, nurse case managers, dietitians, pharmacists, and social workers. At this time, these multidisciplinary clinics do not use standardized risk-based criteria for referral to multidisciplinary clinics and, as a result, patients with varying levels of kidney failure risk attend these clinics, a model which is not sustainable. The proposed revised model of care includes use of the KFRE, with patients at higher risk of kidney failure receiving multidisciplinary care, including a nurse case manager, while lower risk patients would transition to receive care from either general nephrology (without multidisciplinary care) or their primary care provider (Figure 1A). The aim of this study was to understand patient and provider perspectives prior to implementation of the risk-based approach to CKD care, and refine implementation based on their input.
Figure 1.
(A) KFRE-based stratification, as presented to focus group and interview participants and (B) modified KFRE-based stratification based on findings from this qualitative study.
Note. KFRE = kidney failure risk equation; CKD = chronic kidney disease; eGFR = estimated glomerular filtration rate.
Methods
This qualitative study is part of a larger multiphase mixed-methods study evaluating a risk-based approach to guide CKD care using the KFRE; see overview of mixed-methods protocol published separately.10 The goal of this phase is to review our proposed implementation strategy and make modifications if necessary based on perceptions collected from patients, family members, and health care providers. Hence, we sought to determine the perceived benefits and challenges that may arise following implementation of a KFRE-based approach to guide CKD care. We used a qualitative descriptive methodology11 to explore the views of patients with advanced CKD, family members, and health care providers with regard to the perceived benefits and challenges of implementing KFRE-based eligibility criteria in multidisciplinary CKD clinics in Southern Alberta. This included obtaining perspectives from patients and their family members through focus groups, as well as input from health care providers through interviews and open-ended responses from an online survey. Ethics approval was received from the University of Calgary Conjoint Health Research Ethics Board.
Participant Selection and Recruitment
Patients and family members
English-speaking, adult (age 18 and older) nondialysis patients with CKD and their family members who attended a CKD multidisciplinary clinic in Calgary, Canada, were eligible to participate in a focus group. Recruitment took place between November 2016 and January 2017. Nurse clinicians from the 2 multidisciplinary CKD clinics screened patients for eligibility and obtained their consent for study coordinators to contact them during their regular clinic visit. The coordinator subsequently contacted potential patient participants to obtain informed consent.
Health care providers
All staff (nephrologists, nurses, and allied health care professionals) who worked at the 2 multidisciplinary CKD clinics in Calgary, Alberta, were invited via an email invitation letter to participate in a semistructured, one-on-one interview. Two follow-up reminders were provided 1 month after the initial invitation. All interviews were completed in person or by telephone.
All CKD clinic multidisciplinary staff were also invited to complete an online anonymous survey, distributed via email link from November 2016 through January 2017. An initial invitation was sent in November 2016, and a reminder was sent 1 month after the initial invitation. The qualitative responses from the open-ended survey questions were incorporated in this work.
Participant Characteristics
Patients and family members
The majority of focus group participants were male greater than 65 years of age with advanced CKD (Table 1). Most participants had attended the CKD multidisciplinary clinic for greater than 5 years, and reported their health status as fair or good.
Table 1.
Demographic Characteristics of Patient/Family Caregiver Participants in Focus Groups (n = 12).
| Characteristic | n (%) |
|---|---|
| Participant type | |
| Patient | 9 (75.0) |
| Family member | 3 (25.0) |
| Gender | |
| Male | 7 (58.3) |
| Female | 5 (41.7) |
| Age | |
| <50 | 0 (0.0) |
| 50-64 | 1 (8.3) |
| 65-74 | 6 (50.0) |
| ≥75 | 4 (33.3) |
| Did not answer | 1 (8.3) |
| Years at CKD clinic | |
| <1 | 0 (0.0) |
| 1-5 | 5 (41.7) |
| >5 | 7 (58.3) |
| Marital status | |
| Single | 2 (16.6) |
| Married | 6 (50.0) |
| Other | 3 (25.0) |
| Did not answer | 1 (8.3) |
| Employment status | |
| Full-time or part-time | 0 (0.0) |
| Retired | 8 (66.7) |
| Not employed | 2 (16.6) |
| Did not answer | 2 (16.6) |
| Level of education | |
| <Grade 12 | 2 (16.6) |
| High school diploma | 3 (25.0) |
| College, trade school, or university | 4 (33.3) |
| Graduate school | 2 (16.6) |
| Did not answer | 1 (8.3) |
| Self-reported health Status (patients only, n = 9) | |
| Poor | 0 (0.0) |
| Fair | 4 (44.4) |
| Good | 3 (33.3) |
| Very good | 1 (11.1) |
| Excellent | 0 (0.0) |
| Did not answer | 1 (11.1) |
Note. CKD = chronic kidney disease.
Health care providers
Sixteen health care providers participated in an interview (Table 2). The majority of participants had worked in their profession for greater than 10 years and spent greater than 5 years working at the CKD clinic. The majority of interviews occurred in person, with an average duration of ~30 minutes.
Table 2.
Demographic Characteristics of Clinician Participants in Interviews (n = 16).
| Characteristic | n (%) |
|---|---|
| Gender | |
| Male | 8 (50.0) |
| Female | 8 (50.0) |
| Clinic role | |
| Nephrologist | 10 (62.5) |
| Nurse | 5 (31.3) |
| Other | 1 (6.3) |
| Years in profession | |
| <5 | 4 (25.0) |
| 5-10 | 3 (18.8) |
| >10 | 9 (56.3) |
| Years at CKD clinic | |
| <1 | 2 (12.5) |
| 1-5 | 4 (25.0) |
| >5 | 10 (62.5) |
Note. CKD = chronic kidney disease.
Thirty-six of the forty health care providers who completed the anonymous survey completed the open-ended questions. Overall, we received a response rate of 48% (36 of 75; Table 3). The majority of participants were female, had worked in their profession for greater than 10 years, and spent greater than 5 years with the CKD clinic.
Table 3.
Demographic Characteristics of Clinician Participants in Survey (n = 40).
| Characteristic | n (%) |
|---|---|
| Gender | |
| Male | 11 (27.5) |
| Female | 29 (72.5) |
| Clinic role | |
| Nephrologist | 15 (37.5) |
| Nurse | 14 (27.5) |
| Allied health/other | 11 (22.5) |
| Years in profession | |
| <5 | 7 (17.5) |
| 5-10 | 7 (17.5) |
| >10 | 26 (65.0) |
| Years at CKD clinic | |
| <1 | 1 (2.5) |
| 1-5 | 13 (32.5) |
| >5 | 26 (65.0) |
Note. CKD = chronic kidney disease.
Data Collection
We collected demographic information from all participants. Three of the investigators (M.D.S., J.F., and H.T.) with experience conducting qualitative research and not affiliated with the CKD clinics facilitated the patient/family focus groups. The 2 focus groups were held in person for approximately 2 hours each at one of the CKD clinics in Calgary; the location was selected to ensure ease of patient/family access. One investigator (M.D.S.) conducted all provider interviews either in person at the provider’s workplace or over the telephone.
We used open-ended questions during focus groups and interviews to explore perceived barriers and facilitators to implementing the KFRE-based approach to guide CKD care (Supplementary Material, Appendices 1 and 2). We asked probing questions to encourage participants to think about benefits and challenges of the risk-based approach to guide CKD care.
We ceased participant recruitment once we reached data saturation (when we did not attain new additional concepts). All interviews and focus group discussions were audio recorded and transcribed verbatim. Similar to the focus group and interview questions, health care provider participants were asked 3 open-ended questions relating to perceived benefits and challenges to using KFRE to guide clinic eligibility criteria (Supplementary Material, Appendix 3). Written responses were collected online through SimpleSurvey.12
Analysis
We aggregated and summarized patients’, family members’, and health care providers’ perspectives from all data sources (patient/family focus groups, provider interviews, and open-ended responses from provider surveys). Focus group and interview transcripts and open-ended survey responses were imported into NVivo software to assist with data analysis.13 We used a conventional content analysis approach to inductively analyze the transcripts.14 Codes and themes were derived directly from the text data; we did not employ a theory to guide data analysis. Three investigators (M.D.S., J.F., and H.T.) reviewed transcripts independently to identify codes and coding categories, which were subsequently developed into a coding scheme. The investigators discussed preliminary themes to ensure the full range and depth of data was captured (investigator triangulation), resulting in a final coding scheme. All investigators reached consensus on the major themes and subthemes and worked together to interpret linkages across participant groups of the overarching perceived benefits and challenges in transitioning from the existing CKD multidisciplinary clinic model to the proposed risk-stratified model. Major themes were reported back to focus group participants (patients and family members) for feedback. We did not receive additional feedback.
Results
Participant Perspectives
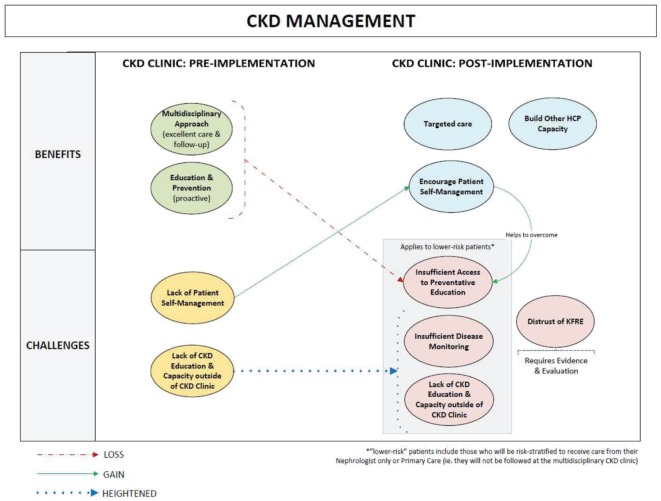
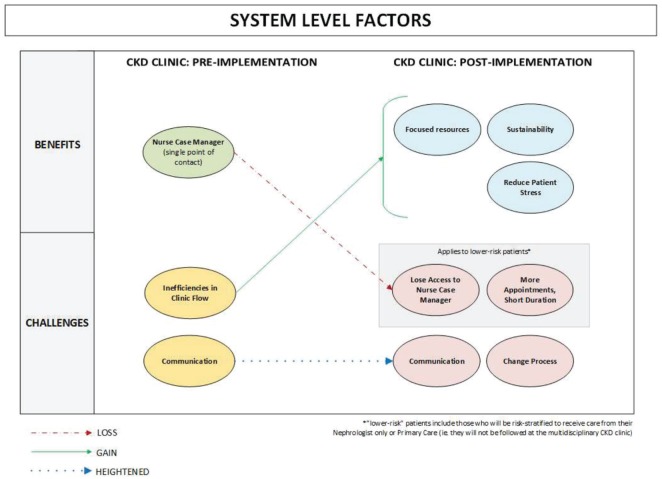
We categorized participant perspectives into 2 themes: CKD management and system-level factors. Within these themes, we describe the perceived benefits and challenges of the KFRE-based approach, as well as subthemes and interrelationships within each primary theme (Figures 2 and 3). An expanded table of exemplary quotes is included in the supplementary material (Appendix 4).
Figure 2.
Relationships between patient and provider perceived CKD management factors, pre- and anticipated post-implementation of the KFRE-based approach to guide CKD care.
Note. CKD = chronic kidney disease; KFRE = kidney failure risk equation; HCP = health care provider.
Figure 3.
Relationships between patient and provider perceived system-level factors, pre- and anticipated post-implementation of the KFRE-based approach to guide CKD care.
Note. CKD = chronic kidney disease; KFRE = kidney failure risk equation.
CKD Management
The CKD management theme included challenges and benefits related to CKD prevention, management, and progression (Figure 2).
Challenges
Lack of CKD education and capacity outside of the CKD clinic
All participant groups speculated that challenges related to lack of CKD knowledge and capacity outside of CKD clinics would be more pronounced following implementation of the risk-based approach for CKD care. Some participants expressed concern that following implementation of the risk-based model of care, there would be insufficient capacity or ability in other health care settings to effectively monitor and manage patients at lower risk of kidney failure. For example, one patient described how a perceived medication error affected her kidney disease: “The family doctor was the one who prescribed the medication [metformin] for diabetes . . . I was left on those medications and the pharmacist caught it, that I shouldn’t be taking it because my kidneys at that time had failed . . . ”
Providers in particular indicated that CKD clinics are currently operating beyond their intended scope, with CKD clinics fulfilling clinical roles that could be more appropriately performed by other providers. One provider for example expressed the need to improve CKD care outside of the clinic: “The CKD clinic should not do everything . . . [the clinic] should build capacity for other providers to provide better care for patients with CKD.”
Lack of patient self-management
Both patients and providers indicated that a lack of self-management strategies, advocacy, and poor health literacy of patients were challenges in the current CKD care model. This intensified concerns about the management of lower risk patients outside of multidisciplinary clinics following implementation of the KFRE-based care model. Providers in particular indicated this was a challenge: “If you don’t have that basic health literacy you don’t make full use of the clinic, or don’t understand even your health situation to a degree.”
Distrust of KFRE; insufficient disease monitoring; insufficient access to preventive education
For some participants, distrust of the KFRE’s predictive ability increased concerns about slowing disease progression in lower risk patients. All participant groups expressed concern that, with the risk-based model of CKD care, lower risk patients may have insufficient access to preventive education and inadequate disease monitoring, which may hasten disease progression. This unease was magnified by suspicion regarding the accuracy of the KFRE. One provider for example said, “I think the largest challenge would be identifying the correct patients, as there is always an exception to the rule,” while a patient also expressed his distrust indicating, “I am no great fan of medical prediction accuracy to put it mildly. I think only too often it is educated guess work at best.”
Benefits
Multidisciplinary approach; proactive education and prevention; targeted care
All participant groups indicated that comprehensive multidisciplinary care that includes access to a nephrologist, nurse, dietitian, pharmacist, and social worker was a key benefit of the current care model. While concern was expressed regarding lower risk patients losing access to the multidisciplinary team, many health care providers indicated that one of the potential benefits of the KFRE-based model was the opportunity to provide individualized care based on patients’ needs. Providers emphasized the importance of focusing resources on the patients who are at higher risk of progressing to kidney failure: “This is targeted care . . . you provide the resources where they’re most required . . . It allows us to flag patients that we know are at high risk of progressing so we know that we need to intervene.”
Providers also felt that the proposed KFRE-based model would help to ensure patients are seen in the most appropriate setting. As one provider indicated, “I think this is great because I think a lot of patients that are now being seen by the clinic don’t need to be seen by the clinic.”
Build other health care provider capacity
Although some patients and providers expressed concern about the capacity of providers to care for CKD patients outside of the CKD clinic, providers also perceived an opportunity for the KFRE-based model to motivate other providers (eg, internal medicine, primary care, community pharmacy) to expand their knowledge regarding kidney disease. Some providers also felt that providing the calculated KFRE value to primary care physicians in their correspondence with them would increase their confidence to manage lower risk CKD patients. A provider commented,
There are some family doctors who . . . would be very reassured and appreciative of knowing that [their patient’s] kidney failure risk is only 2% . . . That would be very reassuring and give them confidence that it’s appropriate for them to keep managing them in primary care. That they don’t have any need to see a nephrologist.
Encourage patient self-management
Some providers indicated that the KFRE-based approach may promote patient self-management and improve health literacy and suggested that the risk-based approach may provide an opportunity for the development of resources and provider-patient conversations that empower the patient to self-manage their kidney disease. “Patients will have a better understanding of their individual risk to progress to end-stage renal disease, and those resistant to engage in education/discussions may be more inclined to do so with this information” (provider).
System-Level Factors
The system-level factors theme included challenges and benefits related to resource use, sustainability, communication, and (in)efficiency of CKD care delivery. Subthemes and relationships are depicted in Figure 3.
Challenges
Communication
All participant groups indicated that effective communication was a challenge in the current CKD care model. This included patient-provider and provider-provider communication (type, amount, and timing of communication), as well as the appropriateness of information given: “There is so much information that it just goes, pop over the top of your head, you can’t remember what the doctor said” (patient). Another patient suggested providing information in stages:
The terminology of what a doctor says, they have got to turn around and put it in plain English to start with. But, they should put it in stages, they shouldn’t turn around and bombard you all at one time . . . when you first get diagnosed all hell lets loose, and you don’t know what to think. We are all flabbergasted.
Some patients and providers also expressed concern that communication-related issues may be heightened for lower risk patients in the risk-based model, particularly if they are returned to primary care.
Inefficiencies in clinic flow
Participants identified multiple inefficiencies in the current CKD care model, which may be improved with the KFRE-based model. Providers noted existing inefficiencies, including duplication of services, overuse of resources, and reluctance to delegate to other health care practitioners, which increases frustration and decreases satisfaction for both patients and providers. Many providers felt that the risk-based model of care would reduce the impact of some of these inefficiencies. For example, a provider commented that they felt the KFRE-based approach would lead to greater “job satisfaction, better utilization of their skill set, improved patient flow, and staff [would be] better able to meet the needs of this patient population.”
Lost access to nurse case manager; more appointments, shorter duration; change process
Overall, many participants expressed concern about change to clinic processes, primarily relating to logistics and coordination. Some patients worried about losing access to the services they knew and trusted, particularly the connection to the nurse case manager. Patients and their family members preferred a “one-stop shop,” regardless of whether they require all the multidisciplinary resources; some preferred to have access to those services via the clinic rather than manage multiple appointments with a variety of specialists. There were also questions about how the tool would be applied, how often, who applies it, how reassessment occurs, and how often.
Benefits
Focused resources; sustainability; reduce patient stress
All participant groups perceived that access to a nurse case manager enhanced patient care, increased patient confidence, and streamlined communication and service delivery for patients. While concern was expressed regarding lost access to the nurse case manager for lower risk patients, many providers felt that focusing resources to allow the nurse case manager and multidisciplinary team to focus on higher risk patients would greatly enhance sustainability of the clinic and potentially lead to greater work satisfaction and reduced workload. In addition, a number of providers indicated that the KFRE-based model may lead to work that is more rewarding, a more appropriate use of clinical skills, and an opportunity to make a significant clinical impact. Providers also mentioned potential for the KFRE-based model to decrease the number of patients on their caseload, allowing time to focus attention on patients who are most at risk of progression: “This will allow for more time to be spent on the patients at the highest risk. Better quality in care if staff are able to spend more time in clinic and on telephone assessments instead of seeing more patients but [providing] less care or rushed care.”
Some patients and providers also suggested that the risk-based model may decrease burden on lower risk patient’s emotional/mental health and physical well-being, because they will be exposed to fewer unnecessary laboratory tests, follow-up visits, and will be aware that their disease trajectory will not likely require renal replacement therapy:
I think that for these low risk patients who aren’t necessarily mulitmorbid, its cutting down on the appointments, letting them live more life outside of clinics and doctors’ appointments, certainly would cut way down on lab work for a lot of patients. (Provider).
Implementation strategy
While we initially proposed 3 risk-based stratification groups (Figure 1A), as a result of feedback received from patients, family members, and health care providers, our implementation strategy was adapted to alleviate concerns regarding lower risk patients. Rather than transition to primary care, lower risk patients will continue to receive care from their nephrologist (Figure 1B).
Discussion
In this qualitative study, patients, family members, and health care providers identified several benefits and challenges related to implementation of a KFRE-based approach to guide CKD care. Overall, participants felt that a KFRE-based approach had the potential to improve efficiency and sustainability of the CKD clinics, but expressed concern about the impact of loss of services for lower risk individuals.
The primary concern identified by participant groups related to low-risk patients (those with a 2-year risk of kidney failure <3%) being risk-stratified to receive care in the community, thereby not receiving follow-up at the multidisciplinary CKD clinic. These concerns stem from perceptions of poor health literacy and poor self-management strategies within this low-risk population, as well as a perceived lack of CKD-specific knowledge and capacity in primary care settings. The concern regarding lack of self-management strategies and tools for patients with CKD is common, and consistent with other studies.15 A prior study has also reported on the challenges experienced by primary care physicians in management of patients with CKD.16
Two point-of-care tools were recently developed and implemented to address these preexisting challenges and build capacity in primary care. An online clinical pathway17 aims to build CKD-specific knowledge relating to patient identification, management, and appropriate referral targeting primary care and community pharmacy practitioners.18,19 In addition, the recent integration of electronic nephrology consultation,20 available to providers across the province, will facilitate access to nephrologist advice and enhance patient care.21 These interventions will support primary care providers and may address participant concerns regarding the management of CKD care for low-risk patients. It is also important to acknowledge participants’ concern regarding the ability of the KFRE to accurately predict patients at highest risk of kidney failure; ongoing evaluation of the KFRE implementation and associated clinical outcomes is a component of the overarching program of study.
Key perceived benefits of KFRE implementation relate to better quality care for those at higher risk of kidney failure, more appropriate use of limited resources, and improvements to overall health care capacity. While research suggests that multidisciplinary CKD team-based care leads to improved outcomes for patients, reduced hospitalizations, and reduced health care costs,22-25 a recent interprovincial Canadian study indicated that suboptimal dialysis initiation, resulting in increased mortality, occurred irrespective of whether a patient was referred to multidisciplinary care “early” or “late.”26 This may be related to the lack of ability to predict patients at highest risk of progression to kidney failure, a limitation that may be addressed through the use of the KFRE-based approach. Use of the KFRE may provide an additional level of clinical decision support to assist the provider to systematically identify patients who are most likely to progress to kidney failure, allowing them to focus resource-intensive multidisciplinary care on patients most likely to benefit from targeted intervention.
Participants also perceived an opportunity for the new KFRE-based model to improve patients’ understanding of their individual clinical situation. Providers saw an opportunity through the KFRE-based approach to focus on patients most likely to progress to kidney failure and therefore most likely to benefit from targeted interventions through the multidisciplinary CKD clinic.
Initially, our proposed implementation of KFRE-based criteria to guide care decisions included stratifying patients to 3 clinical groups based on their risk: patients at higher risk of kidney failure would receive multidisciplinary care, including a nurse case manager, and intermediate- and low-risk patients would receive care from general nephrology or their primary care provider, respectively. Based on the feedback received from patients, family members, and health care providers, our implementation strategy was modified to allocate patients currently in the multidisciplinary clinics to either remain in the multidisciplinary clinic or be followed by their primary nephrologist only. The decision to refer low-risk patients back to their primary care provider only will be made jointly by the nephrologist and the patient, and will not be included within the risk stratification at this point in time. Additional communication tools (letters and information sheets for patients and providers) were also developed based on feedback. New patients being referred to the CKD clinic will be considered using the KFRE-based approach.
A key strength of this study was the inclusion of a diversity of stakeholders’ perspectives (patients, family members, nurses, nephrologists, and allied heath) who provided critical considerations that helped tailor this intervention to the local context. It is important to address the potential limitation introduced by using different data collection methods (patient/family member focus groups vs provider interviews). While we desired to generate more ideas through group participation in focus groups, this method was not feasible for our provider participant group. When interpreting these results, it is also important to consider that this qualitative study involved a greater number of health care providers than patients/family members and that the transferability of our findings is specific to the local context.
Our study identified benefits and challenges to implementation of a KFRE-based approach to guide CKD care. This study is one component of a multiphase mixed-methods study investigating the implementation of a KFRE-based approach to CKD care in Calgary, Canada. In the post-implementation phase of this study, focus groups and interviews will be conducted a second time with patients and providers to further modify the KFRE-based approach if necessary.
Supplemental Material
Supplemental material, SupplMaterial_Risk-based_CKD_Care_CJKHD for Perceived Benefits and Challenges of a Risk-Based Approach to Multidisciplinary Chronic Kidney Disease Care: A Qualitative Descriptive Study by Michelle D. Smekal, Helen Tam-Tham, Juli Finlay, Maoliosa Donald, Eleanor Benterud, Chandra Thomas, Robert R. Quinn, Kin Tam, Braden J. Manns, Marcello Tonelli, Aminu Bello, Navdeep Tangri and Brenda R. Hemmelgarn in Canadian Journal of Kidney Health and Disease
Acknowledgments
The authors thank all research participants for their time and for sharing their perspectives. They acknowledge the chronic kidney disease (CKD) multidisciplinary clinic staff for their support with participant recruitment, and Patricia Wiebe and Corri Robb for assisting with interview and focus group transcriptions.
Footnotes
Ethics Approval and Consent to Participate: This study has been approved by the Conjoint Health Research Ethics Board (CHREB) at the University of Calgary. Informed consent was obtained from all focus group, interview, and survey participants.
Consent for Publication: All authors consent to the publication of this study.
Availability of Data and Materials: Supplementary data for this study is available online.
Author Contributions: All authors in this study have all contributed to this manuscript and approve of this submission. B.R.H., M.D.S., H.T., and J.F. contributed to the study design and drafted the article. All authors contributed to the design and provided critical revisions to this manuscript.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was supported by the Interdisciplinary Chronic Disease Collaboration (ICDC) and the Canadian Institutes of Health Research (CIHR).
ORCID iDs: Michelle D. Smekal  https://orcid.org/0000-0003-0960-3628
https://orcid.org/0000-0003-0960-3628
Navdeep Tangri  https://orcid.org/0000-0002-5075-6370
https://orcid.org/0000-0002-5075-6370
References
- 1. Arora P, Vasa P, Brenner D, et al. Prevalence estimates of chronic kidney disease in Canada: results of a nationally representative survey. CMAJ. 2013;185(9):E417-E423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Manns L, Scott-Douglas N, Tonelli M, et al. A population-based analysis of quality indicators in CKD. Clin J Am Soc Nephrol. 2017;12(5):727-733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Rigatto C, Sood MM, Tangri N. Risk prediction in chronic kidney disease: pitfalls and caveats. Curr Opin Nephrol Hypertens. 2012;21(6):612-618. [DOI] [PubMed] [Google Scholar]
- 4. Echouffo-Tcheugui JB, Kengne AP. Risk models to predict chronic kidney disease and its progression: a systematic review. PLoS Med. 2012;9(11):e1001344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Tangri N, Stevens LA, Griffith J, et al. A predictive model for progression of chronic kidney disease to kidney failure. JAMA. 2011;305(15):1553-1559. [DOI] [PubMed] [Google Scholar]
- 6. Tangri N, Grams ME, Levey AS, et al. Multinational assessment of accuracy of equations for predicting risk of kidney failure: a meta-analysis. JAMA. 2016;315(2):164-174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Tangri N, Ferguson T, Komenda P. Pro: risk scores for chronic kidney disease progression are robust, powerful and ready for implementation. Nephrol Dial Transplant. 2017;32(5):748-751. [DOI] [PubMed] [Google Scholar]
- 8. Tangri N, Inker LA, Hiebert B, et al. A dynamic predictive model for progression of CKD. Am J Kidney Dis. 2017;69(4):514-520. [DOI] [PubMed] [Google Scholar]
- 9. Whitlock RH, Chartier M, Komenda P, et al. Validation of the kidney failure risk equation in Manitoba Can. J Kidney Health Dis. 2017;4:1-9. doi: 10.1177/2054358117705372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Hemmelgarn B, Smekal M, Weaver R, et al. Implementation and evaluation of a risk-based approach to guide chronic kidney disease care: protocol for a multiphase mixed-methods study. Can J Kidney Health Dis. 2018;5:1-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Sandelowski M. Whatever happened to qualitative description? Res Nurs Health. 2000;23(4):334-340. [DOI] [PubMed] [Google Scholar]
- 12. SimpleSurvey. OutSideSoft Solutions Inc. Montreal, Quebec, Canada: OutSideSoft Solutions Inc; 2017. [Google Scholar]
- 13. NVivo Qualitative Data Analysis Software. Doncaster, Victoria, Australia: QSR International Pty Ltd.; Version 11, 2012. [Google Scholar]
- 14. Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005;15(9):1277-1288. [DOI] [PubMed] [Google Scholar]
- 15. Hemmelgarn BR, Pannu N, Ahmed SB, et al. Determining the research priorities for patients with chronic kidney disease not on dialysis. Nephrol Dial Transplant. 2017;32(5):847-854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Allen AS, Forman JP, Orav EJ, Bates DW, Denker BM, Sequist TD. Primary care management of chronic kidney disease. J Gen Intern Med. 2011;26(4):386-392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Donald M, McBrien K, Jackson W, et al. Development and implementation of an online clinical pathway for adult chronic kidney disease in primary care: a mixed methods study. BMC Med Inform Decis Mak. 2016;16(1):109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Curtis C, Balint C, Al Hamarneh YN, et al. Online clinical pathway for managing adults with chronic kidney disease. Can Pharm J (Ott). 2015;148(5):257-262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Donald M, King-Shier K, Tsuyuki RT, et al. Patient, family physician and community pharmacist perspectives on expanded pharmacy scope of practice: a qualitative study. CMAJ Open. 2017;5(1):E205-E212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Alberta Health Services. eRefferal nephrology advice bulletin, October 20, 2016. http://www.albertanetcare.ca/documents/Nephrology-eBulletin-Oct2016.pdf. Published 2016. Accessed October 20, 2016.
- 21. Bello AK, Molzahn AE, Girard LP, et al. Patient and provider perspectives on the design and implementation of an electronic consultation system for kidney care delivery in Canada: a focus group study. BMJ Open. 2017;7(3):e014784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Hemmelgarn BR, Manns BJ, Zhang J, et al. Association between multidisciplinary care and survival for elderly patients with chronic kidney disease. J Am Soc Nephrol. 2007;18(3):993-999. [DOI] [PubMed] [Google Scholar]
- 23. Dixon J, Borden P, Kaneko TM, Schoolwerth AC. Multidisciplinary CKD care enhances outcomes at dialysis initiation. Nephrol Nurs J. 2011;38(2):165-171. [PubMed] [Google Scholar]
- 24. Curtis BM, Ravani P, Malberti F, et al. The short- and long-term impact of multi-disciplinary clinics in addition to standard nephrology care on patient outcomes. Nephrol Dial Transplant. 2005;20(1):147-154. [DOI] [PubMed] [Google Scholar]
- 25. Goldstein M, Yassa T, Dacouris N, McFarlane P. Multidisciplinary predialysis care and morbidity and mortality of patients on dialysis. Am J Kidney Dis. 2004;44(4):706-714. [PubMed] [Google Scholar]
- 26. Mendelssohn DC, Curtis B, Yeates K, et al. Suboptimal initiation of dialysis with and without early referral to a nephrologist. Nephrol Dial Transplant. 2011;26(9):2959-2965. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, SupplMaterial_Risk-based_CKD_Care_CJKHD for Perceived Benefits and Challenges of a Risk-Based Approach to Multidisciplinary Chronic Kidney Disease Care: A Qualitative Descriptive Study by Michelle D. Smekal, Helen Tam-Tham, Juli Finlay, Maoliosa Donald, Eleanor Benterud, Chandra Thomas, Robert R. Quinn, Kin Tam, Braden J. Manns, Marcello Tonelli, Aminu Bello, Navdeep Tangri and Brenda R. Hemmelgarn in Canadian Journal of Kidney Health and Disease