Abstract
Background
Child maltreatment has been associated with a wide range of mental disorders in adulthood. Whether child maltreatment is specifically associated with psychosis risk in individuals at ultra-high risk (UHR) for psychosis, or leads to a general vulnerability for overall psychopathology in the UHR stage remains unclear. The present study examines the association between child maltreatment and transition to psychosis and other mental disorders.
Methods
The sample consisted of 259 UHR individuals from the EUropean network of national schizophrenia networks studying Gene-Environment Interactions (EU-GEI) study. Participants were followed-up for 2 years to assess clinical outcome. Clinical outcome was assessed at 6 months, 12 months, and 24 months after baseline. Child maltreatment before the age of 17 years was assessed at baseline.
Results
Our findings show that a history of emotional abuse was associated with an increased risk for transition to psychosis (OR = 3.78, 95% CI = 1.17 to 12.39, P = .027). Apart from psychosis, a history of physical abuse was associated with depressive disorder (OR = 4.92, 95% CI = 2.12 to 11.39, P = .001), post-traumatic stress disorder (OR = 2.06, 95% CI = 1.10 to 3.86, P = .023), panic disorder (OR = 2.00, 95% CI = 1.00 to 3.99, P = .048) and social phobia (OR = 2.47, 95% CI = 1.18 to 5.16, P = .016) at follow-up.
Conclusion
Our findings suggest that in the UHR stage child maltreatment is a pluripotent risk factor for developing psychosis, depressive disorder, post-traumatic stress disorder (PTSD), panic disorder, and social phobia in adulthood.
Keywords: child maltreatment, ultra high risk, psychosis, clinical outcome
Introduction
A history of childhood abuse and neglect (hereafter child maltreatment) has been associated with an increased risk of developing various mental disorders in adulthood.1 One group of severe mental illnesses that has been extensively examined in relation to child maltreatment is psychotic disorders.2 In both clinical and population based studies, child maltreatment has been found to substantially increase psychosis risk.3,4
In the last 2 decades research has increasingly focused on early detection of psychosis. Criteria have been established to identify individuals at increased risk for a first episode of psychosis.5 Using these ultra-high risk (UHR) criteria,5 initial transition-to-psychosis rates ranged around an average of approximately 40% within 2 years.5,6 However, the more recent UHR studies have shown a decline in transition rate, with meta-analytic evidence suggesting a transition rate of 20% at 2 years, increasing to 36% after 3 years.7,8 As 70% of individuals meeting UHR criteria will not go on to develop a psychotic episode it is important to search for additional factors that may contribute to psychosis risk. One of these factors that have widely been investigated in clinical samples is child maltreatment.3 The rate of child maltreatment in UHR populations is highly prevalent.9 The 4 UHR studies that examined the effect of child maltreatment on transition to psychosis risk have yielded inconsistent findings.10–13 While 2 studies found that a history of sexual abuse significantly increased the risk for transition to psychosis,12,13 these findings could not be replicated in 2 other UHR cohorts.10,11
In addition, the few UHR studies that did consider the effect of child maltreatment in prospective designs have rarely focused on outcomes other than transition to psychosis. Two recent reports tentatively suggest that UHR individuals with a history of child maltreatment report more persistent subclinical psychotic symptoms, depression, and impaired social functioning at follow-up.10,14 However, to the best of our knowledge there are no UHR studies that specifically examined whether child maltreatment also increases the risk of receiving a diagnosis other than psychosis (as defined by the Diagnostic and Statistical Manual of Mental Disorders IV [DSM-IV]).15 This is important, because studying comorbid diagnoses at follow-up may provide more insight into whether child maltreatment is associated with psychosis risk, or rather a pluripotent risk factor for developing general psychopathology in the UHR stage.
Our aims were to: (1) examine the prevalence of child maltreatment in UHR individuals compared to individuals from a control group, (2) examine the effect of child maltreatment on transition to psychosis at follow-up, and (3) examine the effect of child maltreatment on other Axis-I mental disorders other than psychosis at follow-up.
Methods
Sample
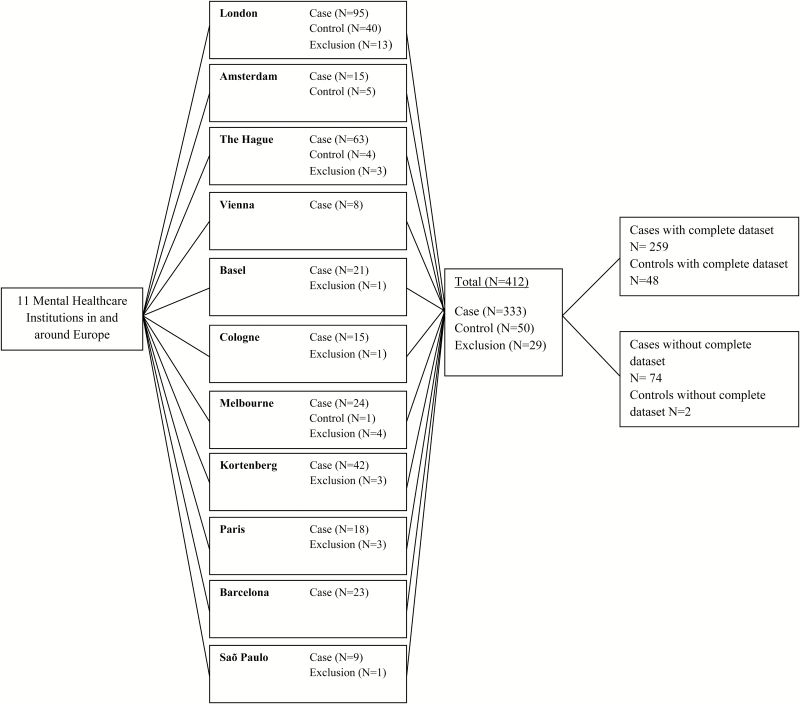
Participants were part of the prodromal work package of the EUropean network of national schizophrenia networks studying Gene-Environment Interactions (EU-GEI) cohort.16 EU-GEI is a naturalistic prospective multicenter study that aimed to identify the interactive genetic, clinical and environmental determinants of schizophrenia. A sample of UHR individuals and controls was recruited from 11 centers (figure 1).
Fig. 1.
Flowchart of participants who reached follow-up assessment by site.
UHR participants, aged 15–35 years (18–35 years in the centers of Cologne, Parnassia, Basel, Vienna, Paris, and London), were eligible to participate if they met at least one of the UHR criteria as defined by the Comprehensive Assessment of At Risk Mental State (CAARMS)5: (1) Vulnerability Group: a first-degree relative with a psychotic disorder or diagnosed with schizotypal personality disorder in combination with a significant drop in functioning during at least 1 month in the previous year, (2) Attenuated Psychotic Symptoms (APS) Group: the presence of sub-threshold positive psychotic symptoms for at least 1 month during the past year, or (3) Brief Limited Intermittent Psychotic Symptoms (BLIPS) Group: an episode of frank psychotic symptoms that lasted no longer than 1 week, which abated spontaneously. Exclusion criteria were: (1) presence of a current or past psychotic disorder, (2) symptoms relevant for inclusion are explained by a medical disorder or drugs or alcohol dependency, (3) IQ < 60.
Controls were recruited from the same geographical catchment area as the UHR group. Exclusion criteria for controls were similar to those for UHR participants. Additionally, controls were excluded when there was presence of an UHR status as defined by the CAARMS.5
Design
Individuals with UHR symptoms were referred to the EU-GEI study by their local mental health care institution. If they agreed to participate, detailed information on the study procedure was provided and the participant was asked to sign informed consent.
Control participants were recruited from 3 centers: the Institute of Psychiatry (IoP) in London, the Personal Assessment and Crisis Evaluation (PACE) clinic in Melbourne, and the Amsterdam Medical Center (AMC)/Parnassia The Hague (figure 1). At the IoP, controls were recruited using GP lists (including all registered patients for whom the practice is responsible for providing primary medical services) and the national postal address file as sampling frames.17 Additionally, controls were recruited from another study at the IoP that recruited controls from the internet (using a website called Gumtree). A few other controls were PhD students from the IoP. At the AMC and Parnassia controls were recruited using a website (Proefbunny). The PACE clinic recruited controls by online advertisement.
Participants were followed up for 2 years and interviewed at 4 time points. Clinical (outcome) measures were assessed at baseline, 12 months and 24 months after baseline (or earlier if they transitioned to psychosis). In addition, 6 months after baseline a brief assessment was conducted. During this assessment changes in subclinical psychotic symptoms and global functioning were assessed. By the time of analyzing the data, some of the follow-up assessments were not finished yet.
If UHR participants made a transition to psychosis during the follow-up period, they were interviewed with the CAARMS. Transition to psychosis was defined as the development of full threshold psychotic disorder according to the CAARMS.5 Where possible, subjects were assessed with the Structured Clinical Interview (SCID-I) to establish a formal diagnosis according to DSM-IV criteria.15 When this was not possible (ie, subjects did not want to attend follow-up assessment) clinical notes were used.
Assessments
All participants completed a detailed sociodemographic schedule. Data on baseline demographic characteristics (eg, age, gender, ethnicity) were assessed using the modified Medical Research Council socio-demographic schedule.16,18
The CAARMS5 was used to assess subclinical psychotic symptoms in the year prior to assessment. The CAARMS is a semi-structured interview conducted to determine presence, severity (0–6), frequency (0–6), distress (0–100) and type of UHR symptoms. The CAARMS consists of 7 subscales: 4 positive symptoms items, 2 cognitive symptom items, 3 emotional disturbance items, 3 negative symptoms items, 4 behavioral change items, 4 motor changes items and 8 general psychopathology items. Criteria for UHR are based on the 4 positive symptoms items only (unusual thought content, non-bizarre ideas, perceptual abnormalities and disorganized speech). This instrument uses the severity and frequency of UHR symptoms to discriminate between status groups (meeting UHR criteria, psychosis, or not at risk).
The SCID-I19 is a standardized interview extensively used in research and clinical settings. This interview assesses current and lifetime Axis I mental disorders using criteria in accordance with the DSM-IV.15 This questionnaire was used to assess clinical outcome.
Child maltreatment was retrospectively assessed with the Child Trauma Questionnaire (CTQ).20 This 25-item self-report questionnaire assesses traumatic events before the age of 17. The CTQ consists of 5 domains: emotional abuse, emotional neglect, sexual abuse, physical abuse, and physical neglect. All items range from 1 (never) to 5 (almost always). Validated cut-off scores of the CTQ were used to evaluate whether participants with a history of maltreatment had worse clinical outcome than participants without a history of maltreatment. The CTQ subscales were dichotomized by the following cut-off scores: physical abuse ≥8, sexual abuse ≥6, emotional abuse ≥9, physical neglect ≥8 and emotional neglect ≥10.21 The subscales were considered as present when scores were above low to moderate. Total maltreatment score was cut-off by the median.
A modified version of the Cannabis Experience Questionnaire22 was administered to asses cannabis (ab)use. In the present study we controlled for current cannabis use, which was assessed with one item: “are you currently using cannabis (yes/no).”
Procedure
EU-GEI was conducted in accordance with the Declaration of Helsinki. The Medical Ethics Committees of all participating sites approved the study protocol. Participants were included after written informed consent. Participants younger than 18 years of age signed for assent, while their parents signed for informed consent. Assessments were conducted by trained psychiatrists, psychologists or research assistants. A web-based training environment was developed in which research assessors had to complete a training module at the start of EU-GEI. To assess interrater reliability, research assessors had to complete online training videos every 12 months. Rating of the online training videos was mandatory; only researchers that succeeded in passing the reliability checks were permitted to assess participants included in EU-GEI.
Statistical Analysis
All analyses were performed in Stata 13. Cases and controls were compared on baseline characteristics using chi-square analysis for categorical dependent variables and independent t tests for continuous dependent variables. Fisher’s exact test was used to compare the prevalence of child maltreatment between cases and controls.
The data has a multilevel structure, because multiple observations are nested within participants (level 1) and participants are nested within sites (level 2). Therefore, multilevel models were used to control for within person level of clustering and clustering within countries. The effect of child maltreatment on transition to psychosis was estimated using multilevel logistic regression (XTMELOGIT). The dependent variable was transition to psychosis (0/1), independent variables were the dichotomized total score of child maltreatment. The dichotomized subscales of child maltreatment were examined in a separate model. Dichotomized scores of child maltreatment were used to place all risk factors (psychopathological symptoms and the various types of maltreatment) on the same (0/1) scale for better comparability and ease of interpretation.
Subsequently, we estimated the effect of child maltreatment on clinical outcome measures according to DSM-IV criteria.15 In these models (XTMELOGIT), binary dependent variables were depressive disorder, panic disorder, social anxiety disorder, obsessive-compulsive disorder (OCD) and post-traumatic stress disorder (PTSD) (SCID-I). Independent variables were dichotomized total maltreatment score. In a separate model the dichotomized sub domains of child maltreatment were examined.
All analyses were adjusted for age, gender and current cannabis use. A significance level of P < .05 was considered statistically significant.
Results
Sample Characteristics
Demographic, clinical and functional baseline data were available for 304 UHR individuals and 50 controls. Of subjects who reached follow-up assessment by the time of analyzing, data on child maltreatment and clinical and functional follow-up data were available for 259 UHR individuals (53.9% male, mean age 22.7, SD 4.5) and 48 controls (55.0% male, mean age 23.98, SD 4.33). These subsamples were used in the present study (table 1). Cases and controls did not significantly differ in terms of age (t = 1.73, P = .084), gender (X2 = 0.36, P = .545) and cannabis use (X2 = 4.68, P = .096). Of subjects with child maltreatment data and follow-up data available, the number of UHR individuals that transitioned to psychosis was 31 (11.9%). Eleven of those 31 made a transition to psychosis within the first 6 months, 13 at 12 months and 7 at 24 months).
Table 1.
Baseline Characteristics for UHR Participants (N = 259)
| Mean age in years (SD) | 22.7 (4.5) |
| Gender male, N (%) | 139 (53.9) |
| Current cannabis use, N (%) | 62 (24.0) |
| UHR intake group, N (%) | |
| APS | 203 (78.7) |
| Genetic risk | 22 (8.4) |
| BLIPS | 15 (5.7) |
| APS and genetic risk | 19 (7.2) |
| SCID depressive disorder, N (%) | 72 (30.4) |
| SCID PTSD, N (%) | 26 (10.1) |
| SCID social disorder, N (%) | 50 (19.4) |
| SCID panic disorder, N (%) | 48 (18.6) |
| SCID OCD, N (%) | 22 (8.5) |
| Total maltreatment mean score, (SD) | 46.8 (15.2) |
| Emotional abuse mean score, (SD) | 11.6 (5.2) |
| Sexual abuse mean score, (SD) | 6.9 (4.0) |
| Physical abuse mean score, (SD) | 7.2 (3.5) |
| Physical neglect mean score, (SD) | 8.1 (3.1) |
| Emotional neglect mean score, (SD) | 13.1 (4.9) |
Note: Demographics of subjects who reached follow-up assessment. OCD, Obsessive Compulsive Disorder; SCID, Structured Clinical Interview; PTSD, posttraumatic stress disorder; UHR, ultra-high risk; APS, attenuated psychotic symptoms; BLIPS, brief limited intermitted psychotic symptoms.
Prevalence of Child Maltreatment in UHR Individuals and Controls
We examined the difference in prevalence of child maltreatment between UHR individuals and controls. Fifty-four percent of the UHR individuals had experienced at least one form of maltreatment during childhood compared to 17.4% of the control sample (P < .001). This difference was apparent for each form of child maltreatment: emotional abuse; cases = 62.5%, controls = 27.1% (P < .001); emotional neglect; cases = 76.4%, controls = 33.3% (P < .001); physical abuse; cases = 24.3%, controls = 8.3% (P = .014); physical neglect; cases = 47.2%, controls = 20.8% (P = .001); sexual abuse; cases = 29.9%, controls = 10.4% (P = .005).
Child Maltreatment and Transition to Psychosis
None of the univariate odds ratios for the association between each individual subtype of maltreatment and transition to psychosis was statistically significant (table 2). In addition, total child maltreatment did not increase the risk for transition to psychosis (OR = 2.46, 95% CI = 0.95 to 6.41, P = .065).
Table 2.
The Effect of Child Maltreatment on Transition to Psychosis
| Adjusted Odds Ratio | 95% CI | P-value | Unadjusted Odds Ratio | 95% CI | P-value | |
|---|---|---|---|---|---|---|
| Emotional abuse | 3.78 | 1.17–12.39 | .027 | 2.14 | 0.79–5.78 | .134 |
| Sexual abuse | 1.67 | 0.66–4.20 | .280 | 1.77 | 0.73–4.25 | .204 |
| Physical abuse | 1.08 | 0.42–2.82 | .869 | 1.39 | 0.58–3.33 | .458 |
| Emotional neglect | 0.26 | 0.09–0.77 | .015 | 0.48 | 0.20–1.16 | .104 |
| Physical neglect | 0.76 | 0.29–1.99 | .575 | 0.89 | 0.39–2.01 | .779 |
Note: Transition to psychosis was controlled for the effect of age, gender and cannabis use. Child Trauma Questionnaire (CTQ) scales were treated as dichotomized variables. In the adjusted column all subscales were entered in one model, in the unadjusted column subscales of maltreatment were entered separately.
The bold values indicate significance level P < .05.
Examination of the adjusted odds ratios showed that, while controlling for the other subtypes, a history of emotional abuse significantly contributes to transition (OR = 3.78, 95% CI = 1.17 to 12.39, P = .027), while the adjusted odds ratio of emotional neglect protects against transition (OR = 0.26, 95% CI = 0.09 to 0.77, P = .015). These findings could be caused by co linearity, and therefore the variance inflation factor (VIF) was determined. A VIF of 1.22 was found, which is below the critical value of 10. This indicates that the findings of the adjusted ORs are not a statistical artifact.
Child Maltreatment and Clinical Outcome
Table 3 presents findings on the association between a history of child maltreatment and DSM-IV disorders. Our results show that a history of overall child maltreatment was positively associated with depressive disorder (OR = 4.92, 95% CI = 2.12 to 11.39, P = .001). Examination of the sub domains of child maltreatment revealed that a history of emotional abuse (OR = 2.76, 95% CI = 1.01 to 7.55, P = .048) accounted for most of this association. Additionally, a history of physical abuse was positively associated with PTSD (OR = 2.06, 95% CI = 1.10 to 3.86, P = .023), panic disorder (OR = 2.00, 95% CI = 1.00 to 3.99, P = .048) and social phobia (OR = 2.47, 95% CI = 1.18 to 5.16, P = .016).
Table 3.
Associations Between Child Maltreatment and DSM-IV Disorders
| Odds Ratio | 95% CI | P-value | ||
|---|---|---|---|---|
| Depressive disorder | Total child maltreatment | 4.92 | 2.12–11.39 | .001 |
| Emotional abuse | 2.76 | 1.01–7.55 | .048 | |
| Sexual abuse | 0.95 | 0.42–2.14 | .895 | |
| Physical abuse | 1.38 | 0.59–3.20 | .454 | |
| Emotional neglect | 2.11 | 0.66–6.77 | .209 | |
| Physical neglect | 1.97 | 0.84–4.62 | .117 | |
| PTSD | Total child maltreatment | 1.60 | 0.87–2.95 | .130 |
| Emotional abuse | 0.73 | 0.37–1.42 | .352 | |
| Sexual abuse | 0.91 | 0.52–1.62 | .761 | |
| Physical abuse | 2.06 | 1.10–3.86 | .023 | |
| Emotional neglect | 0.95 | 0.45–2.05 | .905 | |
| Physical neglect | 1.80 | 0.99–3.26 | .054 | |
| Panic disorder | Total child maltreatment | 0.64 | 0.35–1.19 | .164 |
| Emotional abuse | 0.81 | 0.40–1.65 | .564 | |
| Sexual abuse | 0.85 | 0.46–1.58 | .615 | |
| Physical abuse | 2.00 | 1.00–3.99 | .048 | |
| Emotional neglect | 0.67 | 0.30–1.49 | .329 | |
| Physical neglect | 1.31 | 0.69–2.46 | .399 | |
| Social phobia | Total child maltreatment | 0.94 | 0.45–1.97 | .877 |
| Emotional abuse | 0.57 | 0.26–1.22 | .145 | |
| Sexual abuse | 0.83 | 0.42–1.61 | .578 | |
| Physical abuse | 2.47 | 1.18–5.16 | .016 | |
| Emotional neglect | 2.02 | 0.83–4.92 | .122 | |
| Physical neglect | 0.96 | 0.49–1.90 | .915 | |
| OCD | Total child maltreatment | 1.11 | 0.64–1.93 | .714 |
| Emotional abuse | 0.73 | 0.40–1.33 | .299 | |
| Sexual abuse | 1.02 | 0.61–1.72 | .932 | |
| Physical abuse | 1.22 | 0.69–2.15 | .498 | |
| Emotional neglect | 1.73 | 0.85–3.52 | .130 | |
| Physical neglect | 1.02 | 0.60–1.73 | .943 |
Note: PTSD, post-traumatic stress disorder; OCD, obsessive compulsive disorder. Child Trauma Questionnaire (CTQ) scales were treated as dichotomized variables. All maltreatment subscale scores were entered in the same model. A separate model was conducted to examine the combined effect of child maltreatment on transition to psychosis using the child maltreatment sum score.
The bold values indicate significance level P < .05.
Discussion
Main Findings
In congruence with earlier reports, our findings clearly indicate that child maltreatment is significantly more prevalent in young individuals who present with UHR symptoms compared to controls. Examining the different sub domains of child maltreatment separately, a history of emotional abuse held as a significant predictor of transition to a first episode of psychosis. We also examined whether a history of child maltreatment was associated with mental disorders, other than psychosis. Positive associations were found between a history of child maltreatment and depressive disorder, PTSD, panic disorder and social phobia. In sum, our findings suggest that in UHR cohorts, child maltreatment is a pluripotent risk factor for various psychopathological symptoms in adulthood.
The Effect of Child Maltreatment in the UHR Stage
In the current study we partly confirmed earlier findings pointing to a significant association between a history of child maltreatment and an increased risk for transitioning to psychosis.12,13 While in previous reports associations were strongest for sexual abuse, our findings showed an effect for emotional abuse. However, this effect was only apparent when controlling for the effects of other types of maltreatment. Interestingly, emotional neglect significantly protected against transition to psychosis. This is in line with a study in patients with first episode psychosis, showing that emotional abuse was significantly associated with positive symptoms, while (although not significantly) a negative effect was found for emotional neglect.23 It might be that childhood without emotional comfort or protection teaches the child that he can stand being neglected and survive on its own. Interestingly, these findings suggest that different types of child maltreatment might have different effects on developing psychosis. However, it should also be noted that different types of child maltreatment are likely to co-occur, and further research is needed to explore the effects of child maltreatment. Although our findings on transition to psychosis are congruent with 2 studies from the PACE clinic,12,13 these findings were not confirmed by 2 other recent UHR studies.10,11 An explanation for the inconsistency could be that studies reporting no association between child maltreatment and psychosis used relatively small study samples.10 Another explanation might be that in the study of Stowkowy and colleagues11 continuous scores of child maltreatment were examined. In the present study, UHR individuals were grouped into those who had experienced less severe child maltreatment and those who had experienced more severe child maltreatment, showing an increased risk for psychosis for those with more severe child maltreatment. Thus, more severe child maltreatment may significantly affect psychosis risk in the UHR stage. However, significant associations were only found for emotional abuse and it might be that child maltreatment is a risk factor for UHR status but that its additional effect on transition to psychosis in the UHR stage is limited.
Our findings on the effect of child maltreatment on other outcome measures apart from psychosis are in line with previous research, showing an association between child maltreatment and depression and anxiety.24 Overall, our results suggest that a history of child maltreatment, and in particular physical abuse, is a risk factor for various anxiety disorders in the UHR stage. Although the UHR stage was originally designed as a risk stage for psychosis, our findings tentatively suggest that the UHR stage is a transdiagnostic stage for various clinical outcomes.25 Therefore, our findings emphasize that the focus in the UHR stage should be broader than psychosis outcome alone.26
Our findings could be explained by the fact that adverse events during child, a period of significant brain maturation, probably impacted neurodevelopment. Exposure to adverse events may result in an overactive stress regulation system and permanent changes in the hypothalamic-pituitary-adrenal (HPA) axis.27–29 An overactive HPA-axis causes increased cortisol levels in the brain, leading to increased distress in reaction to environmental stressors. Psychological processes could also explain the association between child maltreatment and psychopathology. For instance, it has been suggested that the experience of child maltreatment leads to the formation of negative self-schemas.30 Negative self-schemas could potentially lead to the formation of depressive symptoms. Additionally, these negative self-schemas have been suggested to lead to suspiciousness and hyper vigilance to environmental stressors, which in turn could lead to psychosis.30,31
Limitations and Strengths
There are several limitations to the present study that need to be acknowledged. First, the CTQ was used to assess child maltreatment. The CTQ is a retrospective self-report questionnaire and therefore the possibility of recall bias exists. However, previous research showed good reliability of recollection of adverse events in psychotic patients,32 and therefore we do not expect this affected our results to a large extent. Second, the CTQ does not examine important questions about specific details of the trauma. For instance, information on the perpetrator or distress or impact of the traumatic event is not examined with the CTQ. This additional information is needed because it might have important implications in the relation with psychosis. Third, the presence of depressive symptoms might have contributed to an overrepresentation of child maltreatment. Fourth, the 24-month assessment was not finished by the time of analyzing the data, which may have resulted in an underrepresentation of the transition rate. Fourth, in the present study we did not control for risk factors of psychosis such as ethnicity33 and socioeconomic status,34 which are both risk factors for psychosis. Fifth, other forms of child maltreatment (eg, bullying or witnessing domestic violence) that have been associated with psychosis risk35 were not analyzed in the present study. Sixth, previous research showed that recent life-events have been found to increase the risk for transition to psychosis36 but these were not taken into account in the present study. Seventh, the control group was small in comparison to the UHR group and controls were recruited in 3 of the 11 EU-GEI sites, therefore the findings should be interpreted with caution. Eighth, in the current study we controlled for current cannabis use but we did not control for type or quantity of cannabis. Because more frequent cannabis use has been associated with psychosis risk37 this is a limitation of the present study.
The major strengths of the current study were the large sample of UHR individuals and the longitudinal design.
Conclusion
Our findings suggest that in the UHR stage child maltreatment is a pluripotent risk factor for psychosis, depressive disorder, PTSD, panic disorder and social phobia in adulthood. Although the main focus of outcome in UHR studies has been transition to psychosis, our findings show that the focus should be broader than psychosis outcome in the UHR stage. These findings support the notion that the UHR stage is a transdiagnostic stage25 for developing various psychiatric symptoms instead of a risk stage for psychosis outcome alone. Importantly, these findings emphasize the need for reducing the harmful effects of emotional and physical abuse during childhood. Because in particular the combination of child maltreatment and the presence of attenuated psychotic symptoms seems a precursor for severe and complex psychopathology,38 it is warranted to screen for UHR status and childhood abuse in mental health care settings.
Funding
This study is supported by the European Union (European Community’s Seventh Framework Program [grant agreement no. HEALTH-F2-2009–241909; Project EU-GEI]). E.V. is supported by grant 916-15-005 from the Netherlands Organization for Scientific Research. M.J.K. is supported by a Medical Research Council Fellowship (grant MR/J008915/1).
Acknowledgment
The authors have declared that there are no conflicts of interest in relation to the subject of this study.
EU-GEI High Risk Study—Group Author List
Authors
Philip McGuire1, Lucia R. Valmaggia2, Matthew J. Kempton1, Maria Calem1, Stefania Tognin1, Gemma Modinos1, Lieuwe de Haan3, Mark van der Gaag4,5, Eva Velthorst3,6, Tamar C. Kraan3, Nadine Burger5, Daniella S. van Dam3, Neus Barrantes-Vidal7,8,9,10, Tecelli Domínguez-Martínez7, Paula Cristóbal-Narváez7, Thomas R. Kwapil8, Manel Monsonet-Bardají7, Lídia Hinojosa7, Anita Riecher-Rössler11, Stefan Borgwardt11, Charlotte Rapp11, Sarah Ittig11, Erich Studerus11, Renata Smieskova11, Rodrigo Bressan12, Ary Gadelha12, Elisa Brietzke13, Graccielle Asevedo12, Elson Asevedo12, Andre Zugman12, Stephan Ruhrmann14, Dominika Gebhard14, Julia Arnhold15, Joachim Klosterkötter14, Dorte Nordholm16, Lasse Randers16, Kristine Krakauer16, Tanya Louise Naumann16, Louise Birkedal Glenthøj16, Merete Nordentoft16, Marc De Hert17, Ruud van Winkel17, Barnaby Nelson18, Patrick McGorry18, Paul Amminger18, Christos Pantelis18, Athena Politis18, Joanne Goodall18, Gabriele Sachs19, Iris Lasser19, Bernadette Winklbaur19, Mathilde Kazes20, Claire Daban20, Julie Bourgin20, Olivier Gay20, Célia Mam-Lam-Fook20, Marie-Odile Krebs20, Bart P. Rutten21, Jim van Os1,22
Affiliations
1Department of Psychosis Studies, Institute of Psychiatry, King’s College London, London, United Kingdom; 2Department of Psychology, Institute of Psychiatry, Psychology & Neuroscience, King’s College London, London, United Kingdom; 3Department of Psychiatry, Academic Medical Center, University of Amsterdam, Amsterdam, The Netherlands; 4Department of Clinical Psychology, VU University and Amsterdam Public Mental Health research institute, Amsterdam, The Netherlands; 5Department of Psychosis Research, Parnassia Psychiatric Institute, The Hague, The Netherlands; 6Department of Psychiatry, Icahn School of Medicine at Mount Sinai, New York, United States of America; 7Departament de Psicologia, Clínica i de la Salut, Universitat Autònoma de Barcelona, Barcelona, Spain; 8Departament de Salut Mental, Sant Pere Claver-Fundació Sanitària, Barcelona, Spain; 9Spanish Mental Health Research Network, CIBERSAM, Spain; 10Department of Psychology, University of North Carolina at Greensboro, Greensboro, United States of America; 11Center for Gender Research and Early Detection, Psychiatric University Clinics Basel, Basel, Switzerland; 12LiNC - Lab Interdisciplinar Neurociências Clínicas, Depto Psiquiatria, Escola Paulista de Medicina, Universidade Federal de São Paulo – UNIFESP, São Paulo, Brazil; 13Pogram for cognition and Intervention in Individuals in At-Risk Mental States (PRISMA), Department of Psychiatry, Universidade Federal de São Paulo, São Paulo, Brazil; 14Department of Psychiatry and Psychotherapy, University of Cologne, Cologne, Germany; 15Psyberlin, Berlin, Germany; 16Mental Health Center Copenhagen and Center for Clinical Intervention and Neuropsychiatric Schizophrenia Research, CINS, Mental Health Center Glostrup, Mental Health Services in the Capital Region of Copenhagen, University of Copenhagen, Copenhagen, Denmark; 17Department of Neuroscience, University Psychiatric Centre, Catholic University Leuven, Leuven, Belgium; 18Centre for Youth Mental Health, University of Melbourne, Melbourne, Australia; 19Department of Psychiatry and Psychotherapy, Medical University of Vienna, Vienna, Austria; 20University Paris Descartes, Hôpital Sainte-Anne, C’JAAD, Service Hospitalo-Universitaire, Inserm U894, Institut de Psychiatrie, Paris, France; 21Department of Psychiatry and Neuropsychology, School for Mental Health and Neuroscience, Maastricht University Medical Centre, Maastricht, The Netherlands; 22Department of Psychiatry and Psychology, Maastricht University Medical Center, Maastricht, The Netherlands.
References
- 1. Teicher MH, Samson JA. Childhood maltreatment and psychopathology: a case for ecophenotypic variants as clinically and neurobiologically distinct subtypes. Am J Psychiatry. 2013;170:1114–1133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Bendall S, Jackson HJ, Hulbert CA, McGorry PD. Childhood trauma and psychotic disorders: a systematic, critical review of the evidence. Schizophr Bull. 2008;34:568–579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Varese F, Smeets F, Drukker M et al. Childhood adversities increase the risk of psychosis: a meta-analysis of patient-control, prospective- and cross-sectional cohort studies. Schizophr Bull. 2012;38:661–671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Kelleher I, Harley M, Lynch F, Arseneault L, Fitzpatrick C, Cannon M. Associations between childhood trauma, bullying and psychotic symptoms among a school-based adolescent sample. Br J Psychiatry. 2008;193:378–382. [DOI] [PubMed] [Google Scholar]
- 5. Yung AR, Yuen HP, McGorry PD et al. Mapping the onset of psychosis: the Comprehensive Assessment of At-Risk Mental States. Aust N Z J Psychiatry. 2005;39:964–971. [DOI] [PubMed] [Google Scholar]
- 6. McGlashan TH, Zipursky RB, Perkins D et al. Randomized, double-blind trial of olanzapine versus placebo in patients prodromally symptomatic for psychosis. Am J Psychiatry. 2006;163:790–799. [DOI] [PubMed] [Google Scholar]
- 7. Fusar-Poli P, Bonoldi I, Yung AR et al. Predicting psychosis: meta-analysis of transition outcomes in individuals at high clinical risk. Arch Gen Psychiatry. 2012;69:220–229. [DOI] [PubMed] [Google Scholar]
- 8. Simon AE, Velthorst E, Nieman DH, Linszen D, Umbricht D, de Haan L. Ultra high-risk state for psychosis and non-transition: a systematic review. Schizophr Res. 2011;132:8–17. [DOI] [PubMed] [Google Scholar]
- 9. Kraan T, Velthorst E, Smit F, de Haan L, van der Gaag M. Trauma and recent life events in individuals at ultra high risk for psychosis: review and meta-analysis. Schizophr Res. 2015;161:143–149. [DOI] [PubMed] [Google Scholar]
- 10. Kraan T, van Dam DS, Velthorst E et al. Childhood trauma and clinical outcome in patients at ultra-high risk of transition to psychosis. Schizophr Res. 2015;169:193–198. [DOI] [PubMed] [Google Scholar]
- 11. Stowkowy J, Liu L, Cadenhead KS et al. Early traumatic experiences, perceived discrimination and conversion to psychosis in those at clinical high risk for psychosis. Soc Psychiatry Psychiatr Epidemiol. 2016;51:497–503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Bechdolf A, Thompson A, Nelson B et al. Experience of trauma and conversion to psychosis in an ultra-high-risk (prodromal) group. Acta Psychiatr Scand. 2010;121:377–384. [DOI] [PubMed] [Google Scholar]
- 13. Thompson AD, Nelson B, Yuen HP et al. Sexual trauma increases the risk of developing psychosis in an ultra high-risk “prodromal” population. Schizophr Bull. 2014;40:697–706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Yung A, Cotter J, Wood S, McGorry P, Thompson A, Nelson B, Lin A. Childhood maltreatment and transition to psychotic disorder independently predict long-term functioning in young people at ultra-high risk for psychosis. Psychol Med 2015;45:3453–3465. [DOI] [PubMed] [Google Scholar]
- 15. APA. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders IV (DSM-IV). Washington, DC: American Psychiatric Press Inc; 1994. [Google Scholar]
- 16. European Network of National Networks studying Gene-Environment Interactions in Schizophrenia. Identifying gene-environment interactions in schizophrenia: contemporary challenges for integrated, large-scale investigations. Schizophr Bull. 2014;40:729–736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Reininghaus U, Kempton MJ, Valmaggia L et al. Stress sensitivity, aberrant salience, and threat anticipation in early psychosis: an experience sampling study. Schizophr Bull. 2016;42:712–722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Mallett R. Sociodemographic schedule. London, UK: Section of Social Psychiatry, Institute of Psychiatry; 1997. [Google Scholar]
- 19. First M, Spitzer R, Gibbon M, Williams JB.. Structured Clinical Interview for DSM-IV Axis I Disorders (SCID). New York, NY: New York State Psychiatric Institute Biometrics Research; 1995. [Google Scholar]
- 20. Bernstein DP, Stein JA, Newcomb MD et al. Development and validation of a brief screening version of the Childhood Trauma Questionnaire. Child Abuse Negl. 2003;27:169–190. [DOI] [PubMed] [Google Scholar]
- 21. Bernstein DP, Fink L.. Childhood Trauma Questionnaire: A Retrospective Self-Report: Manual. San Antonio, TX: Harcourt Brace & Company; 1998. [Google Scholar]
- 22. Barkus EJ, Stirling J, Hopkins RS, Lewis S. Cannabis-induced psychosis-like experiences are associated with high schizotypy. Psychopathology. 2006;39:175–178. [DOI] [PubMed] [Google Scholar]
- 23. Ramsay CE, Flanagan P, Gantt S, Broussard B, Compton MT. Clinical correlates of maltreatment and traumatic experiences in childhood and adolescence among predominantly African American, socially disadvantaged, hospitalized, first-episode psychosis patients. Psychiatry Res. 2011;188:343–349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Li M, D’Arcy C, Meng X. Maltreatment in childhood substantially increases the risk of adult depression and anxiety in prospective cohort studies: systematic review, meta-analysis, and proportional attributable fractions. Psychol Med. 2016;46:717–730. [DOI] [PubMed] [Google Scholar]
- 25. McGorry P, Nelson B. Why we need a transdiagnostic staging approach to emerging psychopathology, early diagnosis, and treatment. JAMA Psychiatry. 2016;73:191–192. [DOI] [PubMed] [Google Scholar]
- 26. Lin A, Wood SJ, Nelson B, Beavan A, McGorry P, Yung AR. Outcomes of nontransitioned cases in a sample at ultra-high risk for psychosis. Am J Psychiatry. 2015;172:249–258. [DOI] [PubMed] [Google Scholar]
- 27. Walker EF, Diforio D. Schizophrenia: a neural diathesis-stress model. Psychol Rev. 1997;104:667–685. [DOI] [PubMed] [Google Scholar]
- 28. Danese A, McEwen BS. Adverse childhood experiences, allostasis, allostatic load, and age-related disease. Physiol Behav. 2012;106:29–39. [DOI] [PubMed] [Google Scholar]
- 29. Day FL, Valmaggia LR, Mondelli V et al. Blunted cortisol awakening response in people at ultra high risk of developing psychosis. Schizophr Res. 2014;158:25–31. [DOI] [PubMed] [Google Scholar]
- 30. Garety PA, Kuipers E, Fowler D, Freeman D, Bebbington PE. A cognitive model of the positive symptoms of psychosis. Psychol Med. 2001;31:189–195. [DOI] [PubMed] [Google Scholar]
- 31. Kilcommons AM, Morrison AP. Relationships between trauma and psychosis: an exploration of cognitive and dissociative factors. Acta Psychiatr Scand. 2005;112:351–359. [DOI] [PubMed] [Google Scholar]
- 32. Fisher HL, Craig TK, Fearon P et al. Reliability and comparability of psychosis patients’ retrospective reports of childhood abuse. Schizophr Bull. 2011;37:546–553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Selten J-P, Veen N, Feller W et al. Incidence of psychotic disorders in immigrant groups to The Netherlands. Br J Psych. 2001;178:367–372. [DOI] [PubMed] [Google Scholar]
- 34. Byrne M, Agerbo E, Eaton WW, Mortensen PB. Parental socio-economic status and risk of first admission with schizophrenia. Soc Psychiatry Psychiatr Epidemiol. 2004;39:87–96. [DOI] [PubMed] [Google Scholar]
- 35. van Dam DS, van der Ven E, Velthorst E, Selten JP, Morgan C, de Haan L. Childhood bullying and the association with psychosis in non-clinical and clinical samples: a review and meta-analysis. Psychol Med. 2012;42:2463–2474. [DOI] [PubMed] [Google Scholar]
- 36. Beards S, Gayer-Anderson C, Borges S, Dewey ME, Fisher HL, Morgan C. Life events and psychosis: a review and meta-analysis. Schizophr Bull. 2013;39:740–747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Di Forti M, Marconi A, Carra E et al. Proportion of patients in south London with first-episode psychosis attributable to use of high potency cannabis: a case-control study. Lancet Psychiatry. 2015;2:233–238. [DOI] [PubMed] [Google Scholar]
- 38. Okkels N, Trabjerg B, Arendt M, Pedersen CB. Traumatic stress disorders and risk of subsequent schizophrenia spectrum disorder or bipolar disorder: a Nationwide Cohort Study. Schizophr Bull. 2017;43:180–186. doi:10.1093/schbul/sbw1082 [DOI] [PMC free article] [PubMed] [Google Scholar]