Abstract
Trans-esophageal endoscopic ultrasound with fine-needle aspiration (EUS-FNA) is widely used to assess mediastinal masses. Common complications are self-limiting bleeding or pain, but occasionally, more serious accidents have been reported. A 54-year-old woman with a huge mass located in the left middle mediastinum presented 2 days after an EUS-FNA with dyspnea and chest pain. Computed tomography scan showed a massive left pleural effusion. A chest tube was inserted revealing a chylothorax (1800 ml). Over the following days, the pleural effusion did not diminish, requiring a left mini-thoracotomy. Intraoperative findings showed a pedunculated mass arising from the upper lobe. A wedge resection and a ligation of a large lymphatic vessel were performed. Postoperative course was regular. Histology showed a solitary fibrous tumor of the pleura. To our knowledge, the case we describe is the first reported chylothorax after EUS-FNA. Despite the demonstrated safety, particular care is mandatory in case of large, vascular, and heterogeneous masses.
Keywords: Chylothorax, endoscopic ultrasound with fine-needle aspiration, fibrous tumor, migrating tumor
Trans-esophageal endoscopic ultrasound with fine-needle aspiration (EUS-FNA) is widely used for the diagnosis and staging of mediastinal masses. It is a minimally invasive procedure which is effective and generally safe.[1] The vast majority of complications are ascribed to self-limiting bleeding or pain, but occasionally, more serious accidents have been reported.[2] We describe a case of a massive left chylothorax, which occurred following EUS-FNA of a suspected mediastinal mass.
Case Report
A 54-year-old woman was incidentally found to have a 63 mm × 57 mm × 46 mm mass located in the left middle mediastinum [Figure 1], adjacent to the trachea and esophagus. As a collateral finding, she was found to have a right aortic arch; until now, she is asymptomatic. An EUS-FNA was performed in order to obtain a histological diagnosis [Figures 2 and 3]. Two days later, the patient presented to the emergency department with dyspnea and chest pain. Chest X-ray followed by computed tomography (CT) scan showed the presence of a massive left pleural effusion [Figure 4]. A chest tube was inserted, putting in evidence the presence of a chylothorax (1800 ml). Thereafter, following 3 days of a fat-free diet and intravenous antibiotics, pleural effusion did not diminish, requiring a left mini-thoracotomy. Intraoperative findings showed a pedunculated mass arising from the visceral pleura of the upper lobe. A wedge resection and ligation of a large lymphatic vessel located in the left mediastinal fat pad were performed. The patient recovered completely within 4 days and was discharged. Histology showed the presence of “spindle cells” with a low cellularity and low mitotic rate, in keeping with a diagnosis of a solitary fibrous tumor of the pleura.
Figure 1.

Magnetic resonance imaging showing the mass located in the left middle mediastinum
Figure 2.
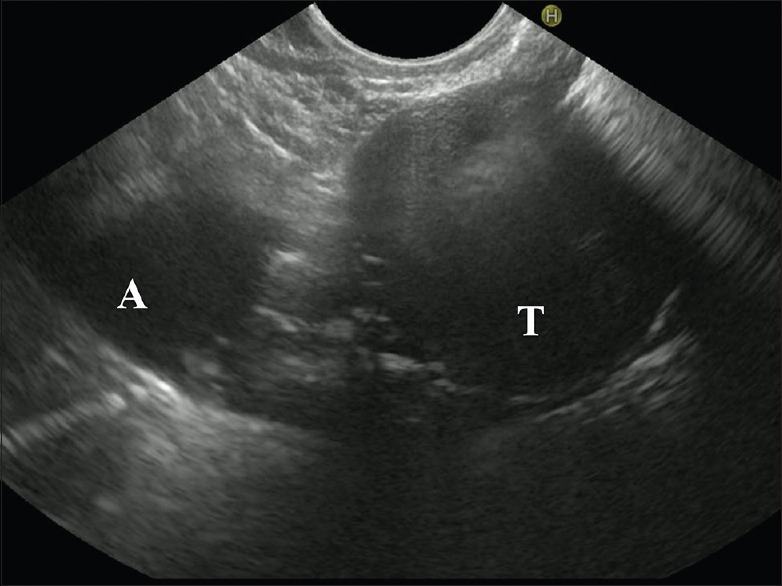
Endoscopic ultrasound images showing the aorta (A), the inhomogeneous appearance of the tumor (T)
Figure 3.
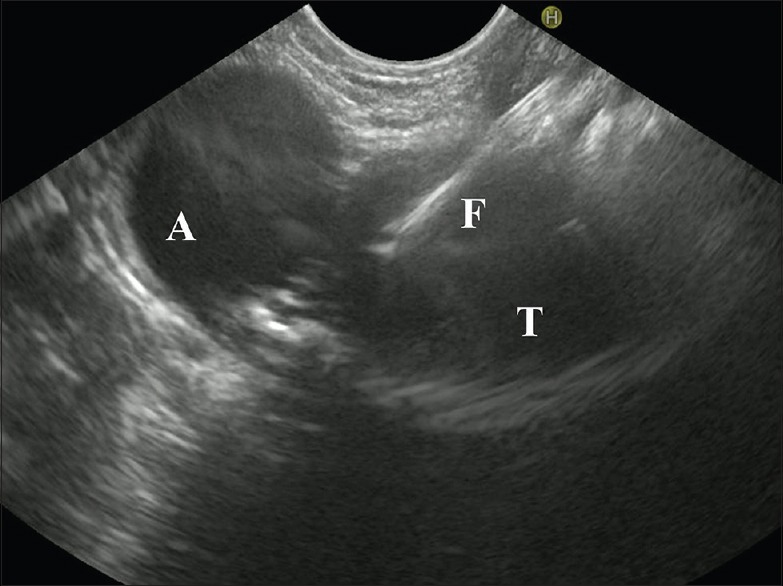
Endoscopic ultrasound-guided-fine-needle aspiration images showing the aorta (A), the inhomogeneous appearance of the tumor (T), and the needle for biopsies (F)
Figure 4.

Computed tomography multiplanar reconstruction showing a massive left pleural effusion
Discussion
To our knowledge, the case we describe is the first reported chylothorax after EUS-FNA. The large pleural effusion following EUS-FNA initially forced us to consider the presence of a hemothorax which is possible, following biopsies of vascularized masses.
EUS-FNA is a minimally invasive technique demonstrated to be accurate in obtaining reliable samples for diagnoses and is considered the gold standard and the first-line investigation for staging of lung cancer. These procedures are not only safe but also cost-effective.[3] However, serious complications after EUS-FNA have been described, such as mediastinitis, pneumonia, pericarditis, cyst infection, and sepsis.[4] Ceuterick et al. reported two cases of esophageal rupture.[5]
The aim of this case report is to highlight a rare serious complication after a routine procedure. Solitary fibrous tumors of the pleura arise from the pleural surface, attached by a broad base or with a small pedicle. CT findings typically demonstrate homogeneous, well-defined, and noninvasive masses, usually adjacent to the chest wall. However, when located near the mediastinum, it can be indistinguishable from other mediastinal neoplasms. The onset of the effusion probably caused a partial compression of the lung and changed the radiological appearance of the tumor which seemed to have a migrating behavior.
Moreover, the presence of the right aortic arch anatomical variant may have created the condition for the onset of the chylothorax, due to a hypothetical distortion of the normal lymphatic network. The fat-free diet was ineffective after 3 days, and due to the suspicion of a large lymphatic vessel injury, a surgical intervention was indicated. The intraoperative findings were favorable for a diagnostic and potentially curative surgical resection of the mass without the need for surgical biopsy.
We can conclude that, despite the demonstrated safety of the EUS-FNA, particular care is mandatory in the case of large, vascular, and heterogeneous masses with the necessity of meticulous attention, when the anatomy and their relationship with the neighboring organs is not clear.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Al-Haddad M, Wallace MB, Woodward TA, Gross SA, Hodgens CM, Toton RD, et al. The safety of fine-needle aspiration guided by endoscopic ultrasound: A prospective study. Endoscopy. 2008;40:204–8. doi: 10.1055/s-2007-995336. [DOI] [PubMed] [Google Scholar]
- 2.Aerts JG, Kloover J, Los J, van der Heijden O, Janssens A, Tournoy KG, et al. EUS-FNA of enlarged necrotic lymph nodes may cause infectious mediastinitis. J Thorac Oncol. 2008;3:1191–3. doi: 10.1097/JTO.0b013e3181872752. [DOI] [PubMed] [Google Scholar]
- 3.Hegde PV, Liberman M. Mediastinal staging: Endosonographic ultrasound lymph node biopsy or mediastinoscopy. Thorac Surg Clin. 2016;26:243–9. doi: 10.1016/j.thorsurg.2016.04.005. [DOI] [PubMed] [Google Scholar]
- 4.Asano F, Aoe M, Ohsaki Y, Okada Y, Sasada S, Sato S, et al. Complications associated with endobronchial ultrasound-guided transbronchial needle aspiration: A nationwide survey by the Japan Society for Respiratory Endoscopy. Respir Res. 2013;14:50. doi: 10.1186/1465-9921-14-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ceuterick V, Decaluwé H, Coosemans W, Nafteux P, Van Veer H, Van Raemdonck D, et al. Esophageal wall rupture after EUS-FNA for mediastinal staging: Report of two cases. Acta Chir Belg. 2016;116:48–50. doi: 10.1080/00015458.2016.1139825. [DOI] [PubMed] [Google Scholar]


