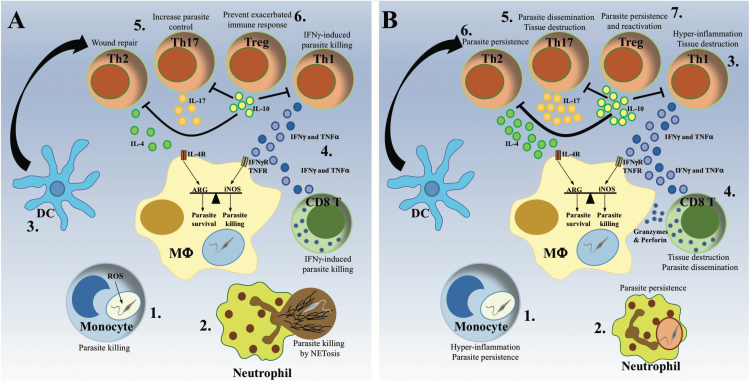
Fig. 3.
Protective and pathological anti-Leishmania immune responses. The same cell types have been associated with either host protection or disease progression depending on parasite species and host immune-competence. (A) The protective immune response. Monocytes (1) and neutrophils (2) are rapidly recruited to the infection site, where they clear Leishmania parasites via ROS production or NET formation, respectively. Subsequently, dendritic cells (DC) migrate to the lymph node (3), where they activate and polarize T cells into different Th populations. The development of a predominant Th1 immune response, characterized by production of IFN-γ and TNF-α by CD4+ and CD8+ T cells (4), activates infected macrophages to kill intracellular parasites via production of NO., while a moderate Th2 and Th17 response has been shown to promote the control of the parasite and the resolution of the infection (5). The subsequent development of IL-10-producing Treg cells ensures the dampening of the immune response, avoiding the development of chronic inflammation (6). (B) The pathological immune response. The excessive recruitment of cytokine-producing monocytes causes hyper-inflammation, which favors parasite persistence (1). Inefficient parasite killing by neutrophils hides parasites from macrophages, interfering with the development of the immune response and favoring parasite persistence (2). Exaggerated IFN-γ and TNF-α production by CD4+ Th1 cells causes hyper-inflammation resulting in tissue destruction (3), whereas the addition of cytotoxic granzymes and perforin by CD8+ T cells promotes parasite dissemination (4). Similarly, a disproportionate Th17 response induces tissue destruction and parasite dissemination, resulting in the formation of metastatic lesions (5). In contrast, an excessive Th2 response promotes parasite persistence and the development of chronic infection (6), while high numbers of IL-10-producing Treg cells promote parasite persistence and re-activation following the resolution of the disease (7).