Abstract
Background
There is interest in assessing healthcare utilization and expenditures among new Medicaid enrollees after the 2014 Medicaid expansion. Recent studies have not differentiated between newly enrolled individuals and those returning after coverage gaps.
Objectives
To assess healthcare expenditures among Medicaid enrollees in the 24 months after Oregon’s 2014 Medicaid expansions and examine whether expenditure patterns were different among the newly, returning, and continuously insured.
Research Design
Retrospective cohort study using inverse-propensity weights to adjust for differences between groups.
Subjects
Oregon adult Medicaid beneficiaries insured continuously from 2014-2015 who were either newly, returning, or continuously insured.
Measures
Monthly expenditures for inpatient care, prescription drugs, total outpatient care, and subdivisions of outpatient care: emergency department (ED), dental, mental and behavioral health (MBH), primary care (PC), and specialist care.
Results
After initial increases, newly and returning insured outpatient expenditures dropped below continuously insured. Expenditures for ED and dental services among the returning insured remained higher than among the newly insured. Newly insured MBH, PC, and specialist expenditures plateaued higher than returning insured. Prescription drug expenditures increased over time for all groups, with continuously insured highest and returning insured lowest. All groups had similar inpatient expenditures over 24 months post-Medicaid expansion.
Conclusions
Our findings reveal that outpatient expenditures for new non-pregnant, non-dual-eligible Oregon Medicaid recipients stabilized over time after meeting pent-up demand, and prior insurance history affected the mix of services that individuals received. Policy evaluations should consider expenditures over at least 24 months and should account for enrollees’ prior insurance histories.
Keywords: Health insurance, Medicaid, medical expenditures, policy evaluation
INTRODUCTION
The Affordable Care Act (ACA) led to historic expansions in Medicaid to cover non-disabled adults with incomes up to 138% of the poverty line. These 2014 Medicaid expansions have enhanced healthcare access and reduced disparities in coverage by income, age, and race/ethnicity.1–2 There has been great interest in assessing healthcare utilization and expenditures among people who enrolled in Medicaid after the implementation of the 2014 expansions. Expenditures for the Medicaid population after 2014 cannot be predicted using pre-2014 data because the population gaining coverage in 2014 differed from the previously enrolled Medicaid population on a number of key characteristics, due to pre-ACA restrictions that limited eligibility to low-income individuals who were pregnant, parents of eligible children, or had specific disabilities.3 Thus, research is needed to understand the healthcare utilization and expenditure patterns of individuals who gained insurance within this new regulatory context.
A recent study reported a surge in demand for care post-ACA, including increased use of preventive services at community health centers (CHC).4 Yet, little is known about whether heightened demand for CHC services occurred in conjunction with demand for other healthcare services, and whether it represents an initial spike based on pent-up demand that resolves over time, or whether these enrollees have greater, sustained healthcare needs. Initial post-ACA studies suggest that newly insured individuals have lower healthcare needs than those insured continuously,5–6 with a decreasing reliance on emergency care over time5 as well as lower total monthly expenditures.6 These studies, however, were limited to 6 to 12 months of post-expansion data, and while they compare newly and continuously insured populations, they do not separate individuals who are completely new to Medicaid from those who have returned after coverage gaps (the ‘returning insured’). Understanding patterns among the returning insured and differentiating this group from the newly insured is particularly important given past evidence regarding how transitioning on and off Medicaid frequently (known as ‘churn’) is associated with higher rates of healthcare utilization.7–8
Oregon is the expansion state that experienced the fourth-highest coverage gain in the first year, from 14.7% uninsured in 2013 to 9.7% in 2014.9 Oregon Medicaid enrollment jumped from 614,183 enrollees in 2013 to over a million–a quarter of the state’s population–by the end of 2015.10 Thus, Oregon is an excellent setting in which to further examine the 2014 Medicaid expansion and study the effect of insurance gain on a large segment of the state’s population. To address gaps in current evidence stemming from short study periods and coarsely-defined insurance groups, we conducted a retrospective cohort study of Medicaid-insured adults who were insured for 24 months after the 2014 Oregon Medicaid expansion. We modeled monthly inpatient, prescription drug (Rx), total outpatient, and subdivisions of outpatient [emergency department (ED), dental, mental and behavioral health (MBH), specialist, and primary care (PC)] Medicaid expenditures over the two years following insurance gains, aiming to better understand the long-term healthcare utilization patterns of individuals as a function of their prior coverage histories.
METHODS
Study Population
Our study population included adults aged 19-64 insured by Oregon Medicaid continuously from January 2014 through December 2015.We obtained Oregon Medicaid enrollment data (01/01/2002-12/31/2015) and administrative claims (01/01/2014-12/31/2015) from the Oregon Health Authority that included both fee-for-service and managed care beneficiaries. We used the enrollment data to create the following insurance groups:
Newly insured patients did not have Medicaid coverage from 2002-2013 and had continuous coverage in 2014-2015;
Returning insured patients had Medicaid coverage sometime during 2002-2012, no coverage in 2013, and continuous coverage in 2014-2015;
Continuously insured patients had Medicaid coverage for all of 2013 and continuous coverage in 2014-2015.
We excluded patients without coverage on 1/1/2014 and those with coverage gaps during the study period, so that changes in mean monthly expenditures would reflect changes in utilization among enrolled individuals rather than changes in enrollment. Because we had no access to Medicare data, we excluded patients with dual Medicaid and Medicare eligibility. We further excluded patients whose 2014-2015 eligibility did not depend on FPL (e.g. pregnant women), as coverage for these patients was not related to the Medicaid expansion. Of 622,513 adults aged 19-64 with any 2014 Medicaid enrollment, 230,602 (37%) remained in our sample. See Appendix Exhibit 1 for details on exclusions.
Propensity Score Weighting
Because the insurance groups differed on a number of characteristics that affect medical expenditure, we used inverse-probability of treatment weighting (IPTW) to adjust for observable differences between groups. Specifically, we implemented a generalized boosted model that included the patient’s age, sex, racial and ethnic background, rural setting, and comorbidity level as assessed by the enhanced Charlson comorbidity index11 to generate weights.12 Average treatment effect (ATE) propensity weights were specified using the twang13 (toolkit for weighting and analysis of nonequivalent groups) package in R (version 3.4.0). We calculated absolute standardized mean differences (ASMD) between insurance groups before and after weighting to assess propensity score performance; standardized differences of less than 0.10 suggest good balance.
Cost Assignment
Alternative payment methods, implemented in Oregon in 2012 when Medicaid Coordinated Care Organizations (CCOs) moved from a fee-for-service model to a global budget, are known to generate ‘shadow claims’ that include diagnosis and procedure information but record the paid amount as zero; therefore, expenditure estimates based on paid amounts fail to account for payments made outside of a fee-for-service system.14 Therefore, to ensure outpatient services were associated with appropriate and consistent costs, we repriced them by connecting procedure codes with Oregon Medicaid fee schedule amounts.14 We also created standardized expenditures for inpatient and prescription drug claims. For inpatient, we multiplied the diagnosis-related group (DRG) weight of a service by a constant to reprice the claim. Finally, we calculated the 30-day cost associated with each National Drug Code (NDC). For details on the creation of outpatient, inpatient, and medication standardized expenditures, see Appendix Exhibit 2.
Statistical Analysis
We used administrative claims to generate the dependent variables: standardized expenditures for inpatient care, prescription drugs, and total outpatient care in addition to subdivisions of outpatient: outpatient claims were classified as either ED, dental, MBH, PC evaluation, management, and procedures (EM+P), specialist EM+P, and PC/specialist imaging or tests based on a hierarchical system involving procedure code, provider type, provider specialty, place of service, and associated costs (Appendix Exhibit 3).
The primary independent variables were insurance group, time, and their interaction terms. We summarized enrollee utilization outcomes as mean monthly expenditures, running a separate hurdle model for each type. A hurdle is a type of two-part model often used by economists because it addresses zero values in the data incompatible with an assumed continuous distribution of costs.15 In hurdle models, a) the probability of a positive value and b) the actual value, given that it is positive, are assumed to be governed by separate processes. Under the assumption that non-zero values occur once a threshold for any utilization is crossed, a) and b) are combined to yield more accurate predictions of expected costs.
We generated all monthly expenditure estimates and standard errors with churdle, an implementation of Cragg’s exponential hurdle16 in Stata 14.2, using restricted cubic splines17 to capture the differential variation in expenditures over time by insurance cohort. We report 95% confidence intervals on all unadjusted and covariate-adjusted estimates (Appendix Exhibits 4–5).
RESULTS
Covariate Balance
Prior to weighting, the insurance groups differed on multiple demographic characteristics (Table 1). The newly insured (NI) were more likely to be older, male, Hispanic, live in a non-rural location, and have fewer co-morbidities. The returning insured (RI) and continuously insured (CI) were more likely to be younger, female, non-Hispanic white, live in a rural location, and have more comorbidities, with many of these differences especially marked for the continuously insured. Balance improved for all covariates and the effective sample sizes (ESS, the approximate number of observations under simple random sampling that would produce variation equivalent to the weighted sample) after weighting were as follows: 37,821 for the CI, 49,009 for the RI, and 91,951 for the NI, for a total ESS of 178,782.
Table 1.
Characteristics of newly insured, returning insured, and continuously insured.
| Unweighted Sample, % | Inverse Propensity Weighted Sample, % | |||||||
|---|---|---|---|---|---|---|---|---|
| Newly Insured | Returning Insured | Cont. Insured | Max1 ASMD | Newly Insured | Returning Insured | Cont. Insured | Max1 ASMD | |
| Total N/ESS | 111,157 | 60,882 | 58,563 | 91,951 | 49,009 | 37,821 | ||
| Age group | ||||||||
| 19-29 | 22.9 | 31.2 | 31.7 | 0.1906 | 27.3 | 27.3 | 27.3 | 0.002 |
| 30-39 | 21.9 | 25.8 | 28.9 | 0.1586 | 24.7 | 24.7 | 24.7 | 0.0007 |
| 40-64 | 55.2 | 43.0 | 39.3 | 0.3235 | 48.0 | 47.9 | 48.1 | 0.0022 |
| Female | 44.7 | 54.1 | 68.1 | 0.4802 | 53.1 | 53.2 | 53.1 | 0.0021 |
| Ethnicity and Race2 | ||||||||
| Hispanic | 16.0 | 14.7 | 8.9 | 0.2216 | 13.9 | 13.8 | 13.8 | 0.0025 |
| Non-Hispanic Non-White | 8.8 | 9.7 | 8.7 | 0.0354 | 9.1 | 9.0 | 9.0 | 0.0018 |
| Non-Hispanic White | 52.0 | 69.6 | 75.7 | 0.5306 | 62.6 | 62.7 | 62.8 | 0.0027 |
| Non-Hispanic Unknown | 23.2 | 6.0 | 6.8 | 0.7056 | 14.5 | 14.4 | 14.5 | 0.0026 |
| Rural setting2 | 36.5 | 41.6 | 41.8 | 0.1058 | 39.2 | 39.2 | 39.2 | 0.0004 |
| Co-Morbidity Index3 | ||||||||
| 0 | 44.4 | 36.5 | 30.2 | 0.3018 | 38.7 | 38.6 | 38.7 | 0.0019 |
| 1 to 2 | 20.3 | 17.3 | 20.7 | 0.0875 | 19.6 | 19.6 | 19.6 | 0.0007 |
| 3 to 4 | 19.4 | 25.0 | 24.8 | 0.1304 | 22.2 | 22.3 | 22.3 | 0.0006 |
| 5 to 6 | 9.5 | 12.6 | 13.7 | 0.125 | 11.4 | 11.4 | 11.3 | 0.0013 |
| 7+ | 6.5 | 8.6 | 10.6 | 0.1391 | 8.1 | 8.1 | 8.1 | 0.0004 |
Maximum absolute standardized mean difference (ASMD) across all pairwise comparisons for each level of pretreatment covariate.
Rural defined by zip codes ten or more miles from the centroid of a population center of 40,000 people or more (Oregon Office of Rural Health).
Level of co-morbidity assessed by the enhanced Charlson comorbidity index.
Outpatient
Outpatient expenditures for NI and RI rise rapidly over the first seven months. Unadjusted estimates for NI and RI peak in July 2014 at $106 and $122, never reaching the monthly CI average of $139. Adjusted NI and RI estimates trend together, briefly reaching CI estimates before leveling off 15% lower (Figure 1).
Figure 1.
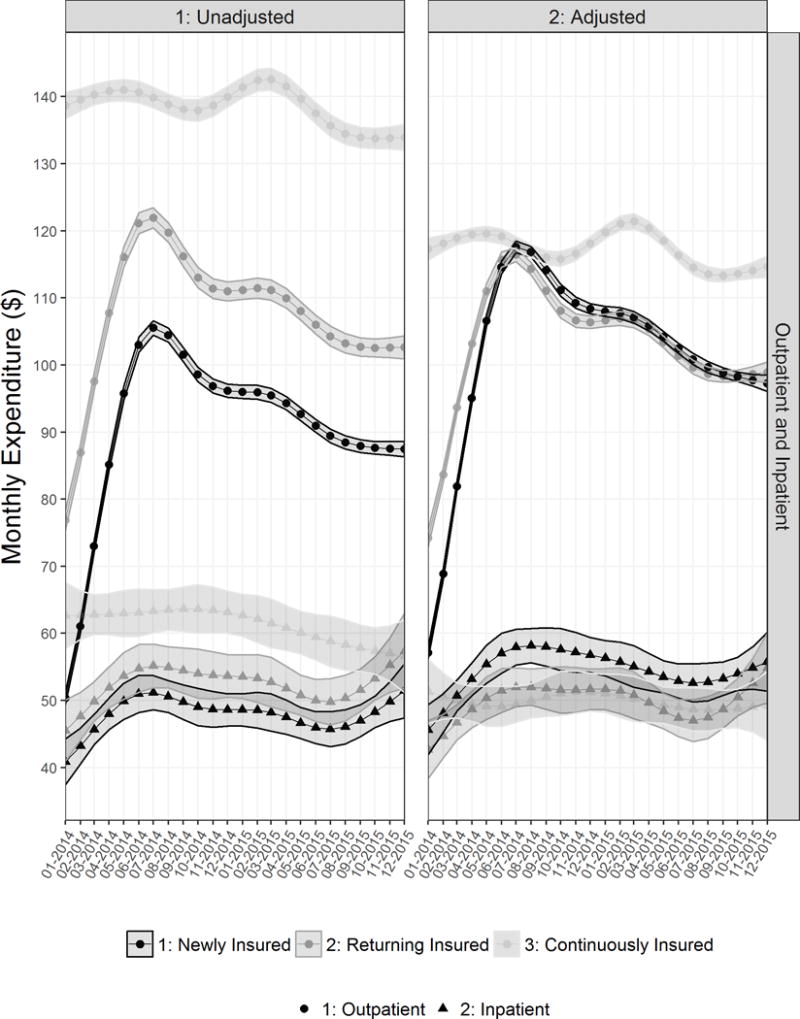
Outpatient and inpatient unadjusted and adjusted mean monthly expenditure estimates and 95% confidence intervals (shaded region) by insurance cohort
Inpatient
Inpatient RI and NI expenditures also rise over the first seven months, though not as sharply. Unadjusted estimates then fluctuate between $50-$57 for RI and $46-$51 for NI, while CI estimates decline from $63 to $57. In the adjusted model, RI and CI levels are comparable, while NI estimates trend slightly higher, though not always significantly so (Figure 1).
Emergency
Emergency expenditures for RI and NI surge in the first half of 2014, then decline. In the unadjusted model, NI and RI peak at $14 and $21 before plateauing around $11 and $18, while CI estimates hover around $22. In the adjusted model, RI surpasses CI in mid-2014 before falling to a comparable level, with NI substantially lower throughout (Figure 2).
Figure 2.
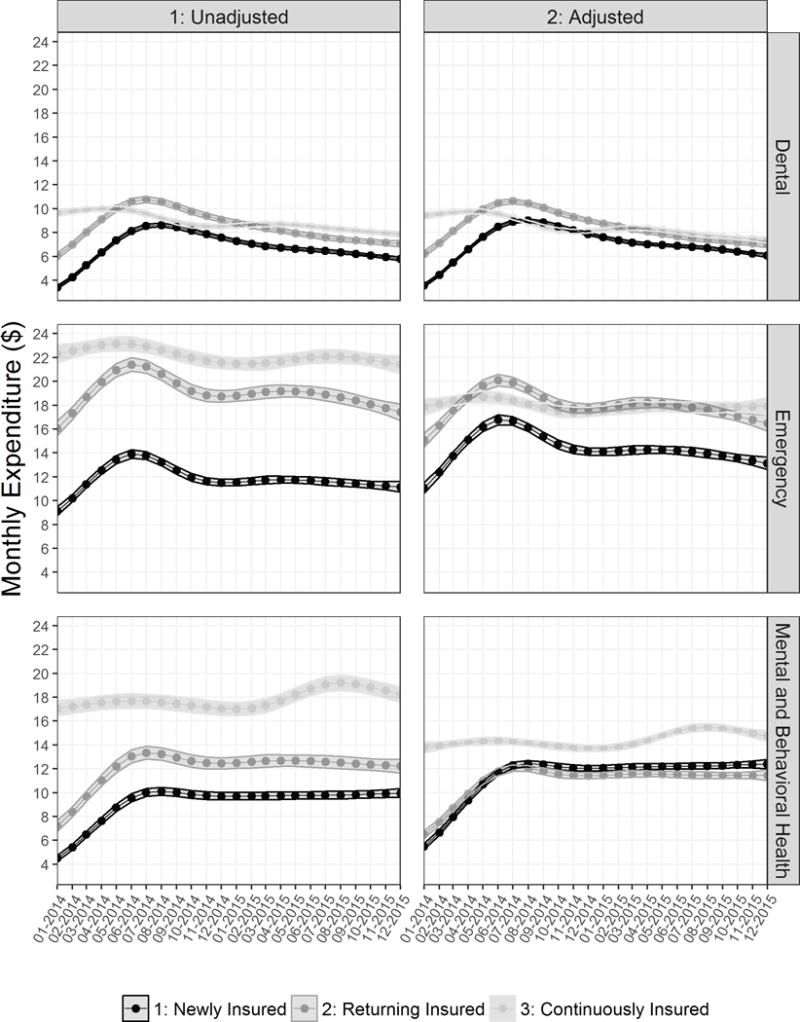
Emergency, dental, and mental and behavioral health unadjusted and adjusted mean monthly expenditure estimates and 95% confidence intervals (shaded region) by insurance cohort
Dental
RI and NI dental expenditures increase during the first half of 2014, then steadily decline. RI peaks above CI at $11 in both adjusted and unadjusted models, which show similar trends. By late 2015, RI and CI have similar adjusted estimates, with NI about 15% lower. (Figure 2).
Mental and Behavioral Health (MBH)
RI and NI MBH expenditures increase sharply in the first half of 2014. After plateauing, unadjusted expenditures average $10 for NI and $13 for RI compared to $18 for CI. Adjusted NI and RI estimates are similar throughout, significantly lower than CI estimates (Figure 2).
Specialist Care: Evaluation, Management and Procedures
Specialist EM + P expenditures for RI and NI more than double over the first half of 2014. In the unadjusted model, NI and RI levels peak at $31 and $33, never reaching the $38 CI monthly average. In the adjusted model, RI catches up to and NI surpasses CI for several months in the latter half of 2014. RI, NI and CI adjusted expenditures all steadily decrease in late 2015, with CI and NI estimates higher than RI (Figure 3).
Figure 3.
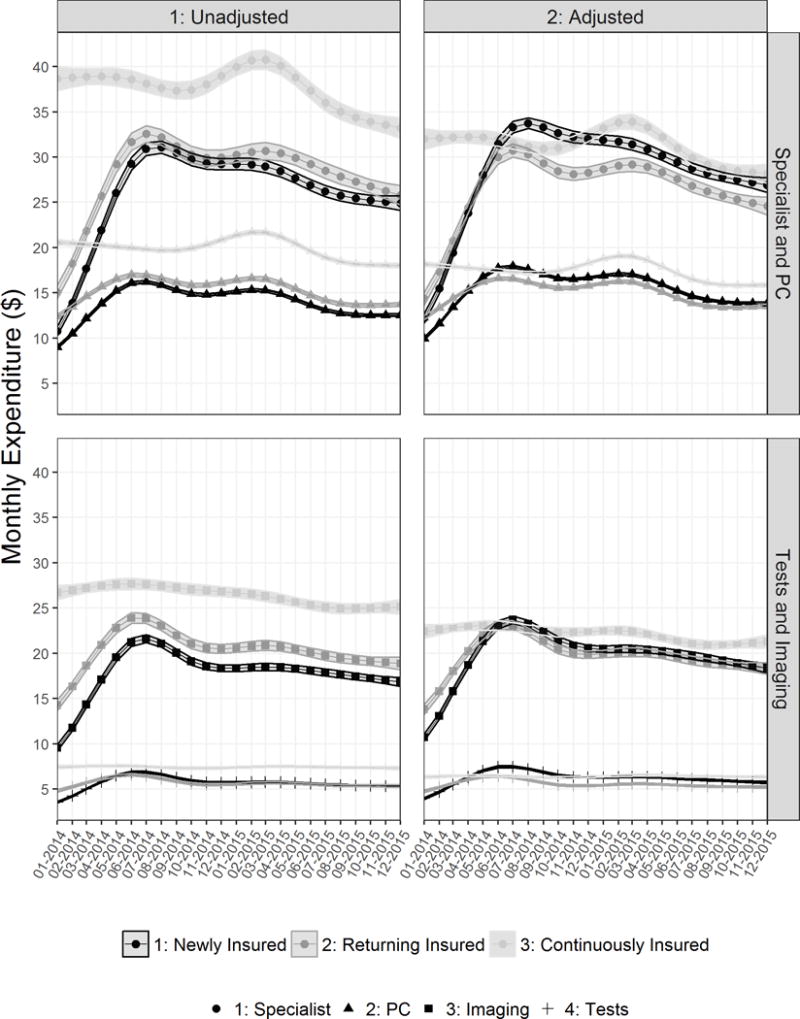
Primary care (PC) and specialist evaluation, management, and procedures (EM+P), imaging, and tests unadjusted and adjusted mean monthly expenditure estimates and 95% confidence intervals (shaded region) by insurance cohort.
Primary Care: Evaluation, Management and Procedures
RI and NI primary care expenditures rise in the first half of 2014 before leveling off. In the unadjusted model, NI and RI levels peak at $16 and $17, never reaching the $20 CI monthly average. In the adjusted model, NI catches up to CI briefly before decreasing below, with RI less than NI. (Figure 3).
PC + Specialist Imaging
Imaging expenditures for RI and NI increase sharply in the first half of 2014 before leveling off. In the unadjusted model, NI and RI levels peak at $22 and $24, never reaching the $26 CI monthly average. In the adjusted model, NI and RI trend together, catching up to CI before decreasing to a level below. (Figure 3).
PC + Specialist Tests
RI and NI test expenditures rise at the start of 2014. Though in the unadjusted model they never quite reach CI levels of $7-$8, in the adjusted model they do, with NI peaking above the others in mid-2014 before all three groups plateau (Figure 3).
Prescription Drugs
Expenditures increase for all three groups throughout, though at a lower rate in 2015 than 2014. Unadjusted expenditures for CI increase from $101 to $116, RI from $22 to $69, and NI from $17 to $69, with RI and NI consistently about $50 less than CI. Adjusted, NI surpasses RI but never reaches CI, staying 20% different from RI and 25% from CI (Figure 4).
Figure 4.
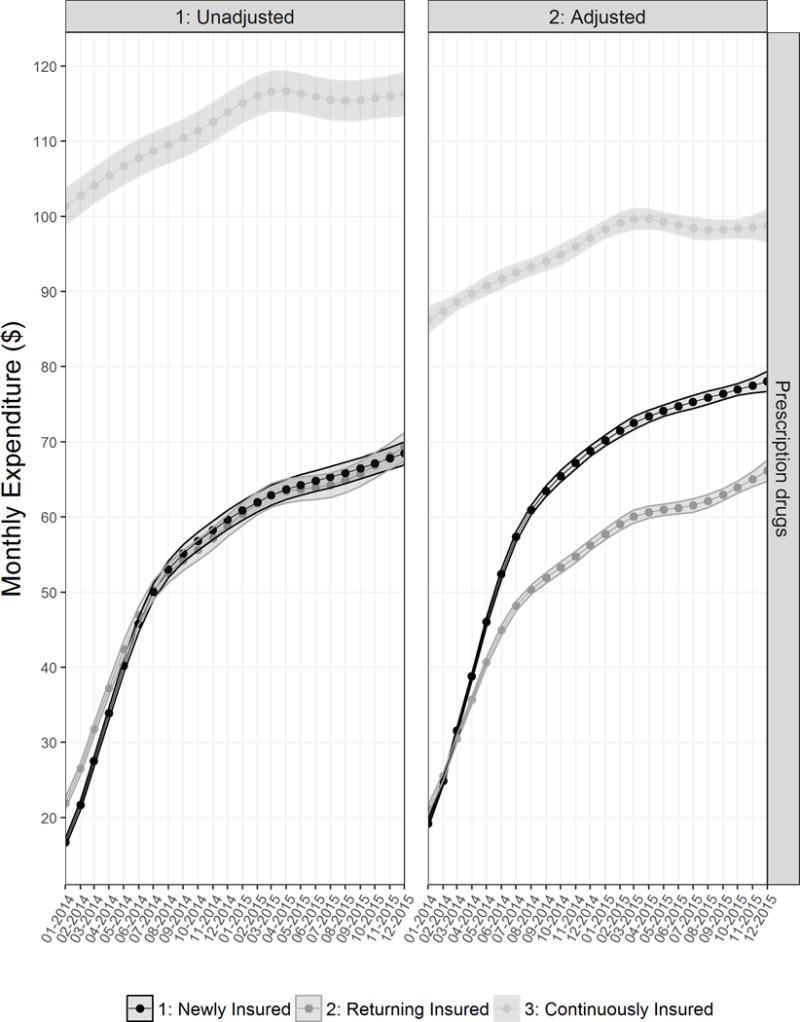
Total prescription drugs mean monthly expenditure estimates and 95% confidence intervals (shaded region) by insurance cohort
DISCUSSION
Our findings confirm and greatly expand on those from a smaller, lottery-based expansion of Medicaid in Oregon in 2008, known as the Oregon Health Insurance Experiment (OHIE), which showed differing effects over time across a variety of healthcare settings for the newly insured, returning insured, and continuously insured.7,18 Our studies examine the effects of expansion in the presence of an insurance mandate, while the OHIE expansion was limited to individuals who were motivated to register for the possibility of obtaining coverage. We complement these analyses of the OHIE expansion by looking at a longer time period, including a greater range of services (dental, inpatient, and prescription drugs), and focusing on monthly expenditures rather than visit rates.
Confirming findings from the OHIE cohort, returning and newly insured individuals in the 2014 expansion population differed from each other substantially in their adjusted ED utilization. Expenditures for both groups jumped initially, but returning insured plateaued at a level comparable to continuously insured, while newly insured estimates were typically about 20% less. Dental expenditures showed similar patterns, with an initial surge followed by returning and continuously insured trending together as newly insured leveled off lower. Oregon Medicaid does not offer comprehensive dental coverage but does cover urgent treatment, which may explain similar patterns for ED and dental care. Our weighting controlled for higher levels of comorbidity among the returning insured relative to the newly insured; however, persistently higher ED and dental expenditures suggest that individuals with Medicaid ‘churn’ in their histories may be more likely to suffer complications from chronic diseases. Their higher medical and social complexity may have led to issues with maintaining coverage in the first place.7
In contrast to previous findings regarding ED utilization in the OHIE population, returning insured expenditures were not higher than (and newly insured expenditures were significantly lower than) continuously insured estimates. Adjusted estimates for both types of new enrollees, while showing the same relationship to one another, were shifted down in relation to corresponding cohorts within the OHIE population (with the continuously insured functioning as a control group, not likely to have changed substantially over this time period). Individuals who gained Medicaid coverage in 2014 likely had a level of baseline need lower than that of the 2008 cohort, which had been found to be older and sicker than the target Oregon Health Plan population.3 The OHIE cohort likely had higher medical needs than the ACA cohort due to the ACA’s individual insurance mandate.
Patterns for mental and behavioral health, specialist, and primary care seem consistent with the pent-up demand hypothesis; after a surge in 2014, newly and returning insured expenditures in these categories fell to a level significantly below the continuously insured. Interestingly, for all MBH/PC/specialist models, returning insured adjusted estimates plateaued lower than newly insured, most markedly in the case of specialist care. We hypothesize that the medical and social complexity leading to coverage instability in the returning insured may present barriers to managing chronic conditions with regular visits, leading to more emergency encounters. Average unadjusted monthly costs in all outpatient categories were greater for returning than newly insured, but their adjusted outpatient expenditures in 2015 were quite similar (both leveling off about 15% below the continuously insured), with ED/dental and PC/MBH/specialist differences roughly cancelling out.
Inpatient expenditures, while showing moderate initial increases for returning and newly insured, did not show strong evidence of an over-time decrease. while absolute costs were greatest for the continuously insured, all three groups had similar adjusted expenditure levels, with the newly insured slightly higher than the others at a number of points. Inpatient costs do not seem to be particularly influenced by insurance coverage history, though perhaps future studies can explore what services may be driving marginally higher newly insured levels. It may be that this group has a higher percentage of undiagnosed conditions requiring hospitalization once diagnosed (e.g., surgeries for cancer discovered after a past-due screening).
Finally, prescription drug expenditures for the returning and newly insured did not plateau or decrease with time after the initial surge; rather, they increased over the entire study period, though at a slower rate after the first seven months. Estimates for the continuously insured, consistently higher than those for the other groups, also increased. This result aligns with studies of national Medicaid expenditures that point to increases in medication costs, with sharper increases in 2014 than 2015.19–20 Though newly and returning insured prescription drug expenditures were indistinguishable after the first half of 2014 in the unadjusted model, newly insured adjusted estimates were greater than those of the returning insured throughout the study period; this result is consistent with past research that showed individuals with insurance discontinuities fill their prescriptions less often.8
Our approach lends additional support to the conclusion that the 2014 Medicaid expansion population had lower average monthly outpatient expenditures than those previously eligible for Medicaid. Confirming results from an earlier study that used survey data,6 we found that the healthier population of newly insured individuals had substantially lower unadjusted monthly expenditures. After adjusting for comorbidity level and other characteristics, we found that new enrollees were still less costly. Our findings are relevant to policymakers in states that have implemented Medicaid expansions and those that have not yet expanded their programs. The data suggest that program evaluators in expansion states should factor enrollees’ prior insurance histories into their assessment, considering Medicaid expenditures over at least 24 months to capture initial and long-term expenditure patterns. Policymakers planning future expansions should prepare for a spike in expenditure from new enrollees, but can expect demand for services to level off. Further, newly insured expenditures likely cannot be predicted from utilization patterns of current or ‘churning’ Medicaid enrollees.
Limitations of our study include the inability to completely characterize healthcare costs for all Medicaid members. Our sample excludes pregnant women and the dual-eligible, both known to have high expenditures, and we did not have access to claims associated with long-term services and support (LTSS), which includes nursing home care. Despite representing almost 30% of 2014-2015 Oregon Medicaid expenditures,21 LTSS likely plays a limited role for the newly enrolled, as utilizers typically have severe health limitations and would have qualified for Medicaid before the expansion. We excluded emergency and non-emergency transportation costs, durable medical equipment (DME), visual aids, and hearing devices. DME, visual aids, and hearing devices are likely to consist largely of one-time expenditures not appropriate for a time course analysis, and transportation rates are difficult to capture via standardized expenditures and cannot be generalized to other states.14 Though they were included in overall outpatient modeling, we did not separately model expenditures for physical therapists, chiropractors, or other ancillary services. Our repricing algorithm did not account for changes in reimbursement rates, nor did we factor in additional payments to providers for meeting quality targets. Despite adjusting for a number of covariates, including comorbidity, it is likely that we were not able to capture group differences on measures of more subtle ailments that may drive up healthcare utilization. Importantly, since our data source was limited to Medicaid claims and enrollment data, we were unable to determine whether new Medicaid enrollees (newly and returning) had other forms of insurance (e.g. private insurance) before 2014. Before 2014, however, there were few comprehensive private coverage options affordable to low-income Americans,22 and recent studies of prior Medicaid expansions have found the ‘crowd-out’ effect on private insurance to be weaker than expected.23–24 Although we were unable to determine whether new enrollees had pre-ACA Medicaid coverage in other states, migrants to Oregon from other states represented only about 3% of the 2014 Oregon population.25 Finally, our study was limited to Oregon Medicaid enrollees and trends may not extend to states with different social resources.
Conclusions
Individuals who gained Medicaid in the 2014 expansion in Oregon showed sharp increases in all outpatient healthcare expenditure categories during the first seven months after the expansion, followed by either a decrease or plateau for the remainder of the study period. After initially catching up with continuously insured levels, adjusted outpatient expenditures for the expansion population (newly and returning insured) were substantially lower than for the continuously insured by the end of the second year post-ACA. These findings suggest that, among our subset of relatively healthier Medicaid recipients, continued healthcare needs were lower among Oregon’s Medicaid expansion population than among the already-insured. Emergency and dental care expenditures among the returning and continuously insured were similar, with significantly higher expenditures in these two groups compared to the newly insured even after covariate-adjustment; in contrast, the newly insured utilized more mental health, specialist, and primary care. The newly insured had higher adjusted estimates for prescription drugs than the returning insured, while both had lower prescription drug expenditures than the continuously insured. These findings suggest that the 2014 Medicaid expansion population likely had an initial spike in expenditures from pent-up demand, but were overall less costly than those already insured by Medicaid. Further, persistent differences between newly and returning insured expenditures in adjusted models suggest that insurance history affects the mix of healthcare services that an individual gaining coverage is likely to need initially and over the long-term. For an accurate understanding of long-term spending for healthcare services, longitudinal studies should consider expenditures over at least 24 months. Evaluations of future healthcare policies should consider enrollees’ prior insurance histories and the over-time stabilization of expenditures when estimating costs.
Supplementary Material
Acknowledgments
This study was approved by the Institutional Review Board at Oregon Health and Sciences University. All authors listed meet the three authorship requirements as stated in the Uniform Requirements for Manuscripts Submitted to Biomedical Journals, and all those who are qualified to be authors are listed in the author byline. To the best of our knowledge, no conflict of interest, financial or other, exists. We thank the Oregon Health Authority for providing the Medicaid data used in this analysis. This work was supported by the Agency for Healthcare Research and Quality (AHRQ), grant number R01HS024270 and by the National Cancer Institutes (NCI) grant numbers R01CA204267 and R01CA181452. This publication was also made possible by Cooperative Agreement Number U18DP006116 jointly funded by the U.S. Centers for Disease Control and Prevention and the National Institute of Diabetes and Digestive and Kidney Disease, and PCORI. The views presented in this article are solely the responsibility of the authors and do not necessarily represent the views of the funding agencies.
Footnotes
Conflict of interest: No financial disclosures were reported by the authors of this paper. The funding agency had no role in study design; collection, analysis, and interpretation of data; writing or submission for publication.
References
- 1.Shartzer A, Long S, Anderson N. Access To Care And Affordability Have Improved Following Affordable Care Act Implementation; Problems Remain. Health Affairs. 2015 doi: 10.1377/hlthaff.2015.0755. [DOI] [PubMed] [Google Scholar]
- 2.Heintzman B, DeVoe J, Cowburn S, et al. In Low-Income Latino Patients, Post-Affordable Care Act Insurance Disparities May Be Reduced Even More than Broader National Estimates: Evidence from Oregon. Journal of Racial and Ethnic Health Disparities. 2016;4(3):329–336. doi: 10.1007/s40615-016-0232-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.The Oregon Health Insurance Experiment. Health Affairs Health Policy Brief. 2015 Jul; http://www.healthaffairs.org/do/10.1377/hpb20150716.236899/full/ Accessed 11/3/2017.
- 4.Hoopes M, Angier H, Gold R, et al. Utilization of Community Health Centers in Medicaid Expansion and Nonexpansion States, 2013–2014. J Ambul Care Manage. 2016;39(4):290–298. doi: 10.1097/JAC.0000000000000123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fertig A, Carlin C, Ode S, et al. Evidence of pent-up demand for care after Medicaid expansion. Medical Care Research and Review. 2017 Mar; doi: 10.1177/1077558717697014. [DOI] [PubMed] [Google Scholar]
- 6.Jacobs P, Kenney G, Selden T. Newly Eligible Enrollees in Medicaid Spend Less and Use Less Care than Those Previously Eligible. Health Affairs. 2017;36(9):1637–1642. doi: 10.1377/hlthaff.2017.0252. [DOI] [PubMed] [Google Scholar]
- 7.O’Malley J, O’Keeffe-Rosetti M, Lowe R, et al. Healthcare Utilization Rates After Oregon’s 2008 Medicaid Expansion: Within-Group and Between-Group Differences over Time Among New, Returning, and Continuously Insured Enrollees. Medical Care. 2016;00(00):1–8. doi: 10.1097/MLR.0000000000000600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Banerjee R, Ziegenfuss J, Shah N. Impact of discontinuity in health insurance on resource utilization. BMC Health Services Research. 2010;10:195. doi: 10.1186/1472-6963-10-195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.U.S. Census Bureau. American Community Survey 1-Year Estimates, 2013 and 2014, Table GCT2701; generated using American FactFinder. http://factfinder.cencus.gov Accessed 11/6/2017.
- 10.Collins J. Oregon’s Health System Transformation: CCO Metrics 2015 Final Report. Oregon Health Authority. 2016 Jun; http://www.oregon.gov/oha/HPA/ANALYTICS-MTX/Documents/CCO-Metrics-2015-Final-Report.pdf Accessed 10/05/2017.
- 11.Charlson M, Charlson R, Peterson J, et al. The Charlson comorbidity index is adapted to predict costs of chronic disease in patients. J Clin Epidemiol. 2008;61(12):1234–1240. doi: 10.1016/j.jclinepi.2008.01.006. [DOI] [PubMed] [Google Scholar]
- 12.McCaffrey D, Griffin B, Almirall D, et al. A Tutorial on Propensity Score Estimation for Multiple Treatments Using Generalized Boosted Models. Statistics in medicine. 2013;32(19):3388–3414. doi: 10.1002/sim.5753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ridgeway G, McCaffrey D, Morral A, et al. twang: Toolkit for Weighting and Analysis of Nonequivalent Groups. R package version 1.5. 2007 https://CRAN.R-project.org/package=twang.
- 14.McConnell J, Renfro S, Lindrooth R, et al. Oregon’s Medicaid Reform And Transition To Global Budgets Were Associated With Reductions In Expenditures. Health Affairs. 2017;36(3):451–459. doi: 10.1377/hlthaff.2016.1298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mihaylova B, Briggs A, O’Hagan A, Thompson S. Review of statistical methods for analyzing healthcare resources and costs. Health Econ. 2011;20(8):897–916. doi: 10.1002/hec.1653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.StataCorp. churdle – Cragg hurdle regression. 2017 https://www.stata.com/manuals/rchurdle.pdf.
- 17.StataCorp. mkspline – Linear and restricted cubic spline construction. 2017 https://www.stata.com/manuals13/rmkspline.pdf.
- 18.Taubman S, Allen H, Wright B, et al. Medicaid increases emergency-department use: evidence from Oregon’s Health Insurance Experiment. Science. 2014;343(6168):263–268. doi: 10.1126/science.1246183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.MACPAC Issue Brief. Medicaid Spending for Prescription Drugs. 2016 Jan; https://www.macpac.gov/wp-content/uploads/2016/01/Medicaid-Spending-for-Prescription-Drugs.pdf Accessed 10/11/2017.
- 20.cms.gov. National Health Expenditures 2015 Highlights. 2015 https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-andReports/NationalHealthExpendData/downloads/highlights.pdf Accessed 10/11/2017.
- 21.Eiken S, Sredl K, Burwell B, et al. Medicaid Expenditures for Long-Term Services and Supports (LTSS) in FY 2015. 2017 https://www.medicaid.gov/medicaid/ltss/downloads/reports-and-evaluations/ltssexpendituresffy2015final.pdf Accessed 1/30/2018.
- 22.Broaddus M, Angeles J. Medicaid Expansion in Health Reform Not Likely to “Crowd Out” Private Health Insurance. 2010 Jun; https://www.cbpp.org/research/medicaid-expansion-in-health-reform-not-likely-to-crowd-out-private-insurance Accessed 1/19/2018.
- 23.Finkelstein A, Taubman S, Wright B, et al. THE OREGON HEALTH INSURANCE EXPERIMENT: EVIDENCE FROM THE FIRST YEAR. The quarterly journal of economics. 2012;127(3):1057–1106. doi: 10.1093/qje/qjs020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dague L, DeLeire T, Friedsam D, et al. What Fraction of Medicaid Enrollees Have Private Insurance Coverage at the Time of Enrollment? Estimates from Administrative Data. Inquiry. 2014 Oct; doi: 10.1177/0046958014544020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.census.gov. State-to-State Migration Flows. 2014 https://www.census.gov/data/tables/time-series/demo/geographic-mobility/state-to-state-migration.html Accessed 1/19/2017.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


