Abstract
Implantanchorage continues to receive much attention as an important orthodontic anchorage. Since the development of orthodontic implants, the scope of applications has continued to increase. Although multiple reviews detailing implants have been published, no comprehensive evaluations have been performed. Thus, the purpose of this study was to comprehensively evaluate the effects of implants based on data published in review articles.
An electronic search of the Cochrane Library, Medline, Embase, Ebsco and Sicencedirect for reviews with “orthodontic” and “systematic review or meta analysis” in the title, abstract, keywords, or full text was performed. A subsequent manual search was then performed to identify reviews concerning orthodontic implants. A manual search of the orthodontic journals American Journal of Orthodontics and Dentofacial Orthopedics (AJODO), European Journal of Orthodontics (EJO), and Angle Othodontist was also performed. Such systematic reviews that evaluated the efficacy and safety of orthodontic implants were used to indicate success rates and molar movements.
A total of 23 reviews were included in the analysis. The quality of each review was assessed using a measurement tool for Assessment of Multiple Systematic Reviews (AMSTAR), and the review chosen to summarize outcomes had a quality score of >6. Most reviews were less than moderate quality. Success rates of implants ranged in a broad scope, and movement of the maxillary first molar was superior with implants compared with traditional anchorage.
Keywords: implant, molar movement, orthodontics, overview, success rate
1. Introduction
Orthodontic anchorage is used to resist the force applied to teeth. Thus, successful orthodontic treatments rely on the adequate control of anchorage. Anchorage can be divided into strong, moderate, and weak anchorage. Traditionally, strong and moderate anchorage requires a headgear, a Nance bow, or a transverse palatal bar (TPA); however, recently implant anchorage have been increasingly used because of their small size, simple operation, high efficacy, and low cost.[1]
Successful orthodontic treatments rely on the control of orthodontic anchorage; however, in many cases, traditional orthodontic anchorage cannot achieve satisfactory results. For example, headgear is dependent on patient appliance, the Nance bow is large and oppresses the mucosa, and TPA lacks sufficient strength.[2]
Recently, implant anchorages have been used for auxiliary anchorage reinforcement. The implant anchorage is typically made of stainless steel, commercially available titanium, or titanium alloy. The diameter of them is from 1 to 2 mm whereas the length is generally 8 to 20 mm. Implant anchorages and dental implants are different in that implant anchorages are not bone-binding, but instead, bind mechanically. Multiple types of implant anchorages are available, mostly including palatal plates, onplants, miniplates, and miniscrews.[3]
Palatal plates: The implant position is primarily on the maxillary hard palate, which is located in the median palatine suture or on either side of the median palatine suture behind the foramina incisivum. Most palatal implants are made of titanium alloy and are screw-like with a cylindrical surface. Following implantation in the oral cavity, impressions are obtained to produce the TPA, which connects the 2 sides of the maxillary teeth to the implant to strengthen the anchor.
Onplants: The onplant has the same role as the palatal plate and is implanted in the median palatine suture. Onplants are button shaped and implanted between the periosteum and jaw. Such implants require secondary surgeries, whereas palatal plates require a single surgery.
Miniplates: Miniplates are implanted on the apical buccal area of the upper and lower jaw, and are implanted following periosteum flap surgery. Titanium plates are fixed in dense buccal bone by miniscrews. Most of the implant is located under the periosteum. Miniplates and miniscrews are made of titanium alloy. Miniplates are applied immediately following implantation, and have better retention than other implants. Miniplates can also withstand large orthopedic forces, including front traction of the maxilla, or retraction of the overall dentition.
Miniscrews: Miniscrews are made of pure titanium or titanium alloy, with a diameter of 1 to 2 mm and a length of 10 mm. The shape of the implant below the bone surface is screw-like, and is not generally used for surface treatment. The advantage of the miniscrew is its simple operation. Miniscrews are self-drilling or auxiliary. Owing to their small size, microscrew implants can be applied to nearly all locations in the jaw or alveolar bone. The most common implant positions are between the buccal-apical side of the upper and lower teeth. The use of miniscrew implants (MIs) controls the movement of teeth in the mesial, distal, and vertical directions, without the need for additional anchorage.
Currently, orthodontists use various temporary anchorage devices (TADs) for anchorage. A considerable body of research has tested the efficacy and success rates of implant anchorages and the aim of this review was to provide information to orthodontists and balance the benefits and harms associated with orthodontic implants anchorage. In this overview, we address the following.
Success rates vary widely among reviews, with no clear conclusions.
The success application of implant anchorages is based on comparisons with traditional anchors, and the movement of teeth. Thus, the overall effectiveness of implant anchorage remains unknown.
Since the advent of orthodontic implant anchorages, multiple reviews have been published; however, only 1 is included in the Cochrane Library database. The remaining reviews are published in magazines and have unknown qualities.
2. Material and methods
2.1. Inclusion criteria for review articles
2.1.1. Types of studies
In accordance with the standard criteria for reviews of orthodontic implant anchorages, we included studies using trials to estimate molar movement and success rates.
2.1.2. Types of participants
All orthodontic implant-based reviews were included and comprised data for teenagers and adults from both sexes and different nationalities and ethnicities.
2.1.3. Types of interventions
Interventions included palatal plates, onplants, miniplates, and miniscrews. Such interventions were delivered as monotherapies or combinations. Success rates and molar movements were evaluated for different orthodontic implants.
2.1.4. Types of outcomes
The primary outcome was success rates of orthodontic implants (i.e., implants remained in the position in which they were implanted). Secondary outcomes included the mean loss of molar anchorage and molar destabilization.
2.2. Search methods to identify reviews
The Cochrane Library, Medline, Embase, Ebsco, and Sicencedirect were searched for reviews with “orthodontic$” and “systematic review or meta-analysis” in the title, abstract, keywords, or full text. A subsequent manual search was then performed to identify reviews concerning orthodontic implants. A manual search of the 3 orthodontic journals AJODO, EJO, and Angle Orthodontist was also performed. The search was performed in September 2016, and the inclusion and exclusion criteria were as follows:
Inclusion criteria:
Systematic reviews or meta-analysis
Randomized controlled clinical trials (RCTs)
Prospective controlled clinical trials (CCTs)
Retrospective controlled cohort studies
Other human studies
No restrictions were applied concerning the publication year or status.
Exclusion criteria:
Studies that failed to perform systematic reviews or meta-analyses.
Studies contains animal studies or corpse research
2.3. Data collection and analysis
2.3.1. Selection of reviews
Two authors (XZ and YS) independently assessed all reviews identified by the search strategy.
2.3.2. Data extraction and management
The data extraction form summarizes the key information obtained from each review, including the participant details, the interventions, comparisons, and outcomes. One author (XZ) extracted the data, whereas the second (YS) verified the extracted information. Disagreements were referred to a third author (YZ) for discussion and resolution.
2.3.3. Assessments of methodological quality of reviews
We used the AMSTAR measurement tool[4] to assess the quality of the reviews. The modified assessment comprised the following 11 factors:
-
1.
Was an “a priori” design provided?
-
2.
Were study-selection and data-extraction methods duplicated?
-
3.
Was a comprehensive literature search performed?
-
4.
Were published and unpublished studies eligible, irrespective of language of publication?
-
5.
Was a list of studies (included and excluded) provided?
-
6.
Were the characteristics of the included studies provided?
-
7.
Was the scientific quality of the included studies assessed and documented?
-
8.
Was the scientific quality of the included studies used appropriately when formulating conclusions?
-
9.
Were appropriate methods used to combine results?
-
10.
Was the likelihood of publication bias assessed?
-
11.
Was a conflict of interest disclosed?
Each criterion was rated as “Yes” (done), “No” (not done), “Can’t answer” (unclear), or “Not applicable.” A “Yes” rating indicated adequate quality and was given a score of 1. Criteria rated as “Not applicable” were not counted against the review, but were removed from the denominator with appropriate adjustment to the ranking. A “No,” “Can’t answer,” and “Not applicable” were given a score of 0. The sum of the scores provided the overall quality score.
All reviews were ranked as being of high quality (scoring 8–11), of medium quality (scoring 4–7), or of low quality (scoring 0–3). Reviews were not excluded based on AMSTAR rankings.
2.4. Data synthesis
To analyze the success rates of implant anchorages and the levels of molar movement compared to traditional anchorage, we analyzed the outcomes of reviews. Owing to the large number of reviews pertaining to orthodontic implants and the complex definition of outcomes, we did not analyze the outcomes by network meta-analysis, but instead extracted high quality data of orthodontic implants for clinicians’ use.
To assess the efficacy of orthodontic implants, we performed this overview at the review level, and did not reanalyze the studies. Although we intended to update the overview immediately using the Cochrane policy, this was not added to the reviews included.[5] Additionally, our decision to update the overview depended on whether the reviews could essentially change the findings from the previous overview.
3. Results
3.1. Description of included reviews
In this study, we screened 2253 articles of all the orthodontic systematic reviews and meta-analyses electronically. And we manually searched 38 reviews concerning orthodontic implants in those 2253 articles beyond the consideration of language, style or if the experiment in the review is about animals but strictly follow our criteria. Then we screened the 38 reviews last time and chose 23 reviews in the 38 articles according to our criteria. A flow chart detailing the articles included is shown in Figure 1. The characteristics of all the 23 reviews are listed in Table 1.[2,3, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26]
Figure 1.
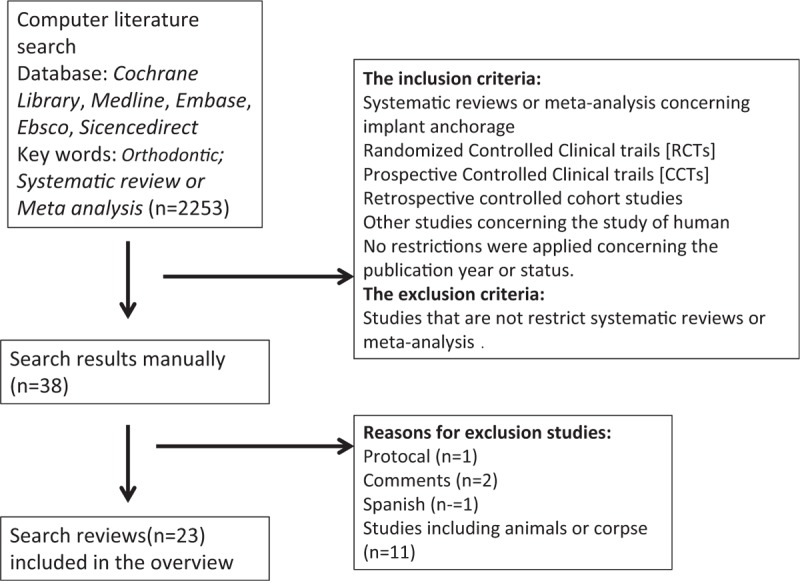
Flowchart illustrating the selection of relevant articles.
Table 1.
PICO of the 23 reviews.
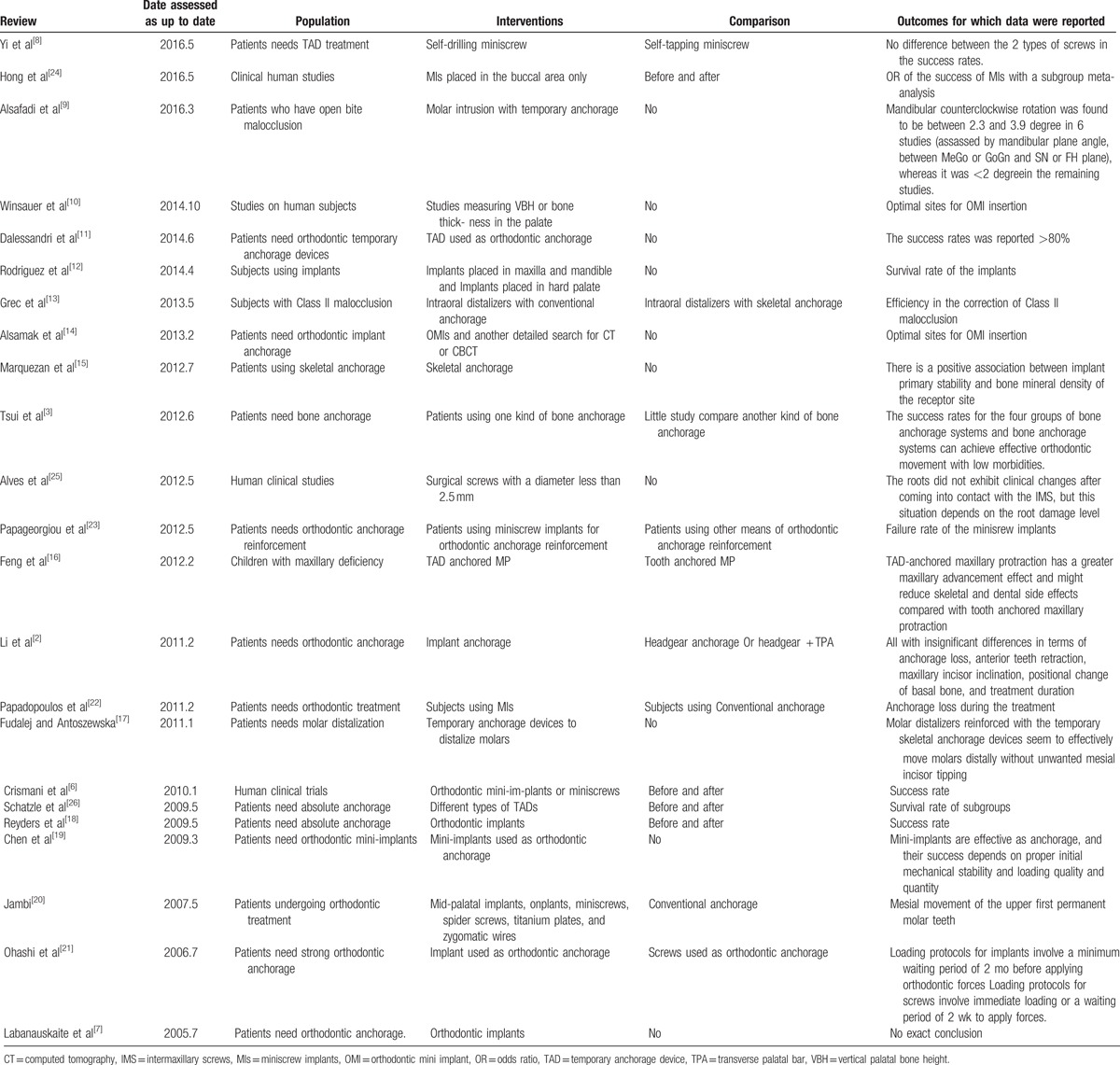
Of the 23 articles selected, the most recent were published in 2016. Among the reviews, some were restricted and included RCT, CCT, and retrospective studies. All others included live humans. The written language was English. The outcomes of the reviews were broad, and included success rates for orthodontic implants and the degrees of molar movements. The remaining outcomes detailed the probability of implants to contact the root, or have front traction in the maxilla. Owing to the small number of articles analyzed, we focused on the success rates and the level of molar movement between implant anchorages and traditional anchorages.
3.2. Methodological quality of the reviews
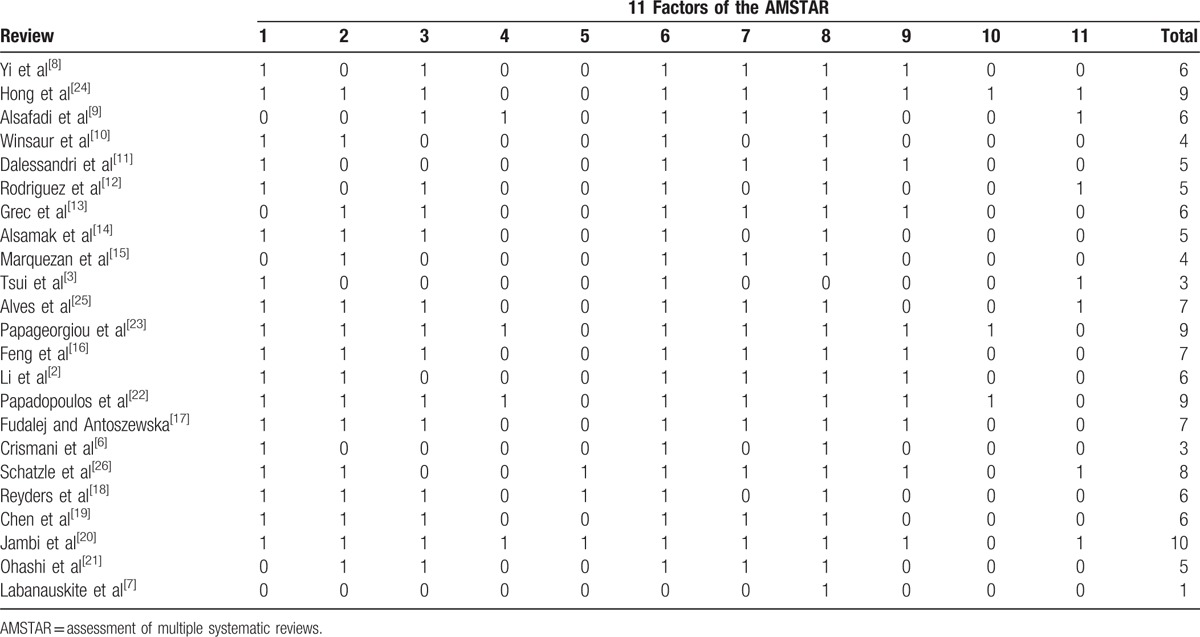
AMSTAR ratings for the reviews are summarized in Table 2.[2,3, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26] All 23 reviews were classified as high, medium, or low quality based on 11 domains. Following our previous classification criteria, a grade of 0 to 3 was considered low quality, 4 to 7 was considered medium quality, and 8 to 11 was considered high quality. A total of 3 articles were deemed to be of low quality,[3,6,7] whereas 15 were of medium quality,[2,8–21] and 5 were of high quality.[22–26]
Table 2.
AMSTAR score of the 23 reviews included.
3.3. Effects of interventions
Orthodontic implants are palatal plates, onplants, miniplates, and miniscrews. All reviews concerning orthodontic implants illustrated the efficacy and application of the 4 implants. To summarize the outcomes of such studies, high-quality reviews were selected. For those studies, the AMSTAR score was 11. We used 50% as the reference and summarized reviews with scores >6. There were 22 outcomes, with most detailing the success rate for implantations and the level of molar movement. Other outcomes included the level of incisor movement, traction of the maxilla, and the rotation of the mandibular plane. Such outcomes were typically present in 1 to 2 reviews; however, most of those reviews were of low quality. Therefore, we focused on the outcomes that clinicians require, which is the success rate and level of molar movement.
3.4. Success rate
The success of an implant is determined by its shedding after implantation. A total of 7 reviews were selected with an AMSTAR score >6. The success rates for those studies are shown in Table 3. All 7 articles were published after 2009.[8,18,19,22–24,26] Only Schatzle et al[26] discussed the success rate of all 4 implant types. The success rate of onplant was 82.8% (64.2%, 94.1%), whereas that of the palatal implant was 89.5% (81.9%, 93.9%), the midplate 92.7% (90.1%, 94.6%), and the miniscrew 83.6% (70.9%, 86.6%). Most other studies evaluated the success rate of miniscrews. For example, Papageogiou et al[23] revealed a miniscrew success rate of 87.7% (83.3%, 91.1%), whereas Papadopoulos et al[22] revealed a similar miniscrew success rate of 84.4% (81.9%, 86.7%). Reynders et al and Chen et al identified a success rate that differed substantially,[18,19] whereas Chen et al and Hong et al did not perform meta-analyses.[19,24]
Table 3.
Outcomes of success rate of the 7 reviews whose AMSTAR score higher than 6.
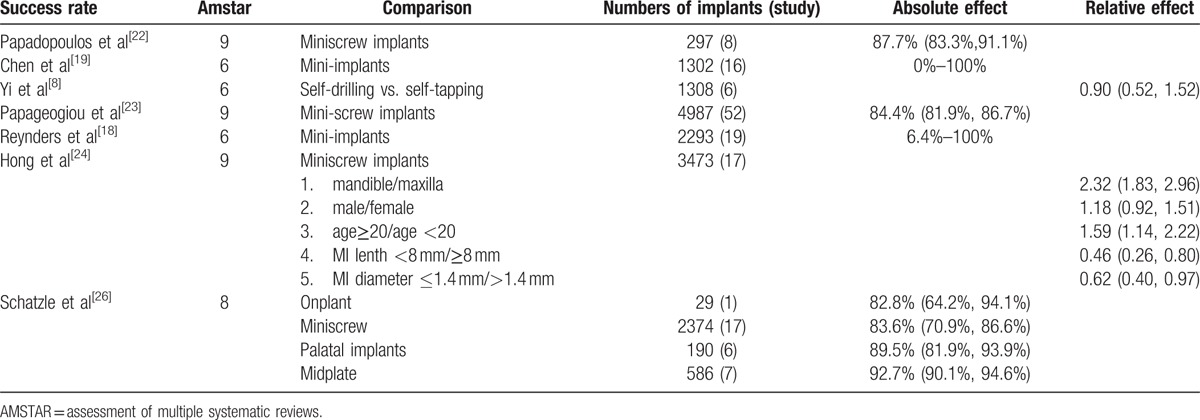
A review by Hong et al, 2016, also performed subgroup analyses; the success rates between different groups were analyzed based on implant position, sex, age, and the length/diameter of miniscrews.[24] They concluded that success rates differed minimally with gender and age; however, the success rate was higher when miniscrews were implanted in the maxilla compared with the mandible. Higher success rates were also observed with longer and larger miniscrews.
3.5. Molar movement
A total of 5 reviews had AMSTAR scores >6 and discussed molar movements in Table 4.[2,13,17,20,22] Papadopoulos compared MIs to traditional anchorages and found that the mean anchor loss of MI was 0.05 (95% confidence interval [CI] = −0.3 to 0.4 mm), while the mean difference in the anchorage-loss ratio was −0.5 (95% CI = −0.6 to 0.3). Papadopoulos et al[22] also performed subgroup analyses between implants in different positions, numbers, ages, or whether they were performed directly or indirectly. However, meta-analyses were not performed.
Table 4.
Outcomes of molar movement of the 6 reviews whose AMSTAR is >6.
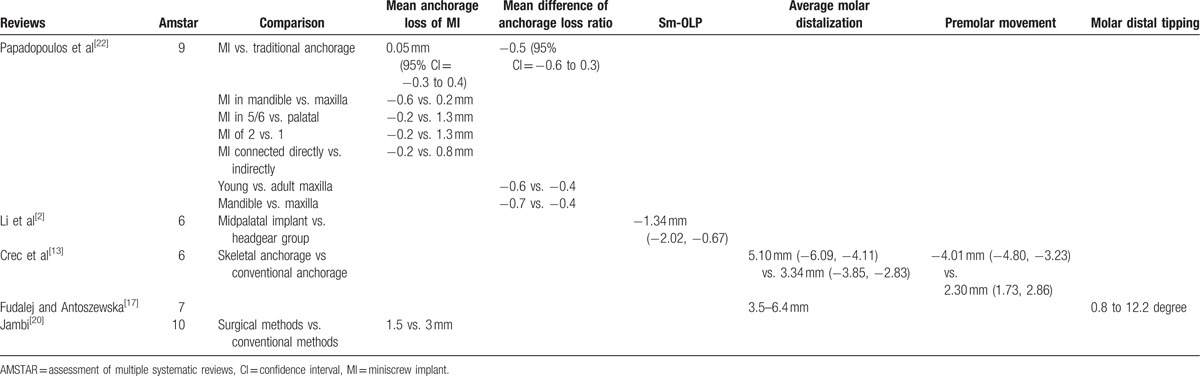
Jambi revealed in the Cochrane Library that the anchorage loss of MI was 1.5 mm, whereas that of traditional anchorages was 3 mm. Additionally, the MI reduced anchorage consumption.[20] Li et al[2] compared midpalatal implants to headgear and concluded that the sm-OLP (the distance of the mesial contact point of the maxillary first permanent molar) was −1.34 mm (−2.02, −0.67), whereas Grec et al compared MIs to traditional anchorage and measured the distilizing distance between the upper first molars and premolars.[13] The distance of the distal molar was 5.10 mm (−6.09, −4.11) when implant anchorages were used, whereas the distance of the distal molar using traditional anchorage was 3.34 mm (−3.85, −2.83). The distance of the distal premolar to the implant was −4.01 mm (−4.80, −3.32) and from the distal premolar to the traditional anchor was 2.30 mm (1.73, 2.86). Fudalej and Antoszewska[17] revealed the inclination of the anchorage molar as 0.8 to 12.2 degree when using implant anchorage.
4. Discussion
This study summarized reviews detailing orthodontic implants. Thus, this overview provides a comprehensive analysis of multiple systematic reviews and meta-analyses of orthodontic implants. When performing an overview, the literature must meet the inclusion criteria and cannot be simply excluded or included based on their quality. As overviews summarize all reviews, even low-quality reviews should be included. An inherent limitation to overviews is that not all reviews will be updated as is desired.
There are multiple sources of bias in the overview process. Studies were screened by the Cochrane assessment and were assumed to represent the most comprehensive and consistent evidence. The underlying weakness is that three authors (ZX, SY, ZY) contributed to the comments outlined in this summary, or provided editorial contributions. To reduce this weakness, we used independent objective criteria, including the modified AMSTAR scale to assess the quality and limitations of the included assessments.
Based on the standards of the Cochrane Library, most reviews that met the inclusion criteria were of moderate quality, whereas 1 article was of high quality. In general, the overall quality of implant reviews was low. Additionally, not all studies of medium quality (or higher) collected meta-data. The reason the quality of reviews pertaining to orthodontic implants was low was because the study design of the orthodontic implants was RCT and most were from perspective and retrospective clinical trials. Thus, trials were unlikely to be blind. Additionally, the duration of orthodontic treatment was long and variable.
Here, we discuss implant success rates and molar movements. We chose a literature score of >6 points and summarized 2 outcomes. High-quality studies were identified that some of them perform meta-analyses. The success rates in high-quality studies were mostly >80%. What's more, although Reynder et al and Chen et al[18,19] give the results of a large range. Some of them did show extreme circumstance such as very poor bone density and very small sample size that cause the success rate to reach 0. Of course, the immature surgery of implantation is also one of the reasons that cause the total failure. So we can conclude that clinicians can refer the conclusion of the success rate of orthodontic implantation to reach 80%. Additionally, molar movements were superior when implant anchorages were used, compared with those associated with the use of traditional anchorages. Thus, when the planting sites and bones are suitable, orthodontists should use implant anchorages. However, when the patient has poor hygiene and the bone of the implantation site is not sufficiently dense, we recommend a different approach for reinforcing the anchorage.
The high-quality studies analyzed in this research suggest that molar movement is reduced by implants and is superior to traditional anchoring techniques. Thus, if implantation conditions permit, it is recommended that implant anchorages be used.
5. Conclusion
Multiple systematic reviews and meta-analyses have been published on orthodontic implants; however, their qualities vary and only a single review is published in the Cochrane Library database. In this overview, we assessed the quality of such systematic reviews and found that most were of moderate quality. The number of high quality studies was small. Thus, clinicians should use caution when reviewing such studies. Additionally, the success rates reported between studies were highly variable. Notably, molar movement was reduced when orthodontic implants were used, compared with when traditional anchorages were used.
Author contributions
Conceptualization: F. Sun, J. Lin, T. Cai, X. Zheng, Y. Sun.
Data curation: J. Lin, X. Zheng, Y. Sun, Y. Zhang.
Formal analysis: J. Lin, Y. Sun.
Investigation: J. Lin.
Methodology: F. Sun, J. Lin, T. Cai, X. Zheng, Y. Sun, Y. Zhang.
Project administration: J. Lin, Y. Sun.
Resources: Y. Zhang.
Supervision: J. Lin.
Writing – original draft: X. Zheng.
Writing – review & editing: F. Sun, J. Lin, T. Cai, Y. Sun, Y. Zhang.
Footnotes
Abbreviations: AMSTAR = assessment of multiple systematic reviews, TPA = transverse palatal bar.
XZ and YS contributed equally to the study.
The English in this document has been checked by at least two professional editors, both native speakers of English. For a certificate, please see: http://www.textcheck.com/certificate/index/yjAXlS.
Funding: No funding was provided for this study.
The authors report no conflicts of interest.
References
- [1].Feldmann I, Bondemark L. Orthodontic anchorage: a systematic review. Angle Orthod 2006;76:493–501. [DOI] [PubMed] [Google Scholar]
- [2].Li F, Hu HK, Chen JW, et al. Comparison of anchorage capacity between implant and headgear during anterior segment retraction. Angle Orthod 2011;81:915–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Tsui WK, Chua HD, Cheung LK. Bone anchor systems for orthodontic application: a systematic review. Int J Oral Maxillofac Surg 2012;41:1427–38. [DOI] [PubMed] [Google Scholar]
- [4].Shea BJ, Grimshaw JM, Wells GA, et al. Development of AMSTAR: a measurement tool to assess the methodological quality of systematic review. BMC Med Res Methodol 2007;7:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Smith V, Devane D, Begley CM, et al. Methodology in conducting a systematic review of systematic reviews of healthcare interventions. BMC Med Res Methodol 2011;11:15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Crismani AG, Berti MH, Celar AG, et al. Miniscrews in orthodontic treatment: review and analysis of published clinical trials. Am J Orthod Dentofacial Orthop 2011;137:108–13. [DOI] [PubMed] [Google Scholar]
- [7].Labanauskaite B, Jankauskas G, Vasiliauskas A, et al. Implant for orthodontic anchorage. Meta-analysis. Stomatologija 2005;7:128–32. [PubMed] [Google Scholar]
- [8].Yi J, Ge M, Li M, et al. Comparison of the success rate betweem self-drilling and self-tapping miniscrews: a systematic review and meta-analysis. Eur J Orthod 2016;10:287–93. [DOI] [PubMed] [Google Scholar]
- [9].Alsafadi AS, Alabdullah MM, Saltaji H, et al. Effect of molar intrusion with temporary anchorage devices in patients with anterior open bite: a systematic review. Prog Orthod 2016;17:9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Winsauer H, Vlachojannis C, Bumann A, et al. Paramedian vertical palatal bone height for mini-implant insertion: a systematic review. Eur J Orthod 2014;36:541–9. [DOI] [PubMed] [Google Scholar]
- [11].Dalessandri D, Salgarello S, Dalsessandri M, et al. Determinants for success rates of temporary anchorage devices in orthodontics: a meta-analysis (n>50). Eur J Orthod 2014;36:303–13. [DOI] [PubMed] [Google Scholar]
- [12].Rodriquez JC, Suarez F, Chan HL, et al. Implants for orthodontic anchorage: success rates and reasons. Implant Dent 2014;23:155–61. [DOI] [PubMed] [Google Scholar]
- [13].Grec RH, Janson G, Branco NC, et al. Intraoral distalizer effects with conventional and skeletal anchorage: a meta-analysis. Am J Orthod Dentofacial Orthop 2013;143:602–15. [DOI] [PubMed] [Google Scholar]
- [14].Alsamak S, Psomiadis S, Gkantidis M. Positional guidelines for orthodontic mini-implant placement in the anterior region: a systematic review. Int J Oral Maxillofac Implants 2013;28:470–9. [DOI] [PubMed] [Google Scholar]
- [15].Marquezan M, Osorio A, Sant’Anna E, et al. Does bone miner density influence the primary stability of dental implants? A systematic review. Clin Oral Implants Res 2012;23:767–74. [DOI] [PubMed] [Google Scholar]
- [16].Feng X, Li J, Li Y, et al. Effectiveness of TAD-anchored maxillary protraction in late mixed dentition. Angle Orthod 2012;82:1107–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Fudalej P, Antoszewska J. Are orthodontic distalizers reinforced with the temporary skeletal anchorage devices effective. Am J Orthod Dentofacial Orthop 2011;139:722–9. [DOI] [PubMed] [Google Scholar]
- [18].Reynders R, Ronchi L, Bipat S. Mini-implants in orthodontics: a systematic review of the literature. Am J Orthod Dentofacial Orthop 2009;135:564–5. [DOI] [PubMed] [Google Scholar]
- [19].Chen Y, Kyung HM, Zhao WT, et al. Critical factors for the success of orthodontic mini-implants: a systematic review. Am J Orthod Dentofacial Orthop 2009;135:284–91. [DOI] [PubMed] [Google Scholar]
- [20].Jambi S, Walsh T, Sandler J, et al. Reinforcement of anchorage during orthodontic brace treatment with implants or other surgical methods. Cochrane Database Syst Rev 2007;18:CD005098. [DOI] [PubMed] [Google Scholar]
- [21].Ohashi E, Pecho OE, Moron M, et al. Implant vs screw loading protocols in orthodontics. Angle Orthod 2006;76:721–7. [DOI] [PubMed] [Google Scholar]
- [22].Papadopoulos MA, Papageorgiou SN, Zogakis P. Clinical effectiveness of orthodontic miniscrew implants: a meta-analysis. J Dent Res 2011;90:969–76. [DOI] [PubMed] [Google Scholar]
- [23].Papageorgiou SN, Zogakis IP, Papadopoulos MA. Failure rates and associated risk factors of orthodontic miniscrew implants: a meta-analysis. Am J Orthod Dentofacial Orthop 2012;142:577–95. [DOI] [PubMed] [Google Scholar]
- [24].Hong SB, Kusnoto B, Kim EJ, et al. Prognostic factors associated with the success rates of posterior orthodontic miniscrew implants: A subgroup meta-analysis. Korean J Orthod 2016;46:111–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Alves M, Jr, Baratieri C, Araujo MT, et al. Root damage associated with intermaxillary screws: a systematic review. Int J Oral Maxillofac Surg 2012;41:1445–50. [DOI] [PubMed] [Google Scholar]
- [26].Schatzle M, Mannchen R, Zwahlen M, et al. Survival and failure rates of orthodontic temporary anchorage devices: a systematic review. Clin Oral Implants Res 2009;20:1352–9. [DOI] [PubMed] [Google Scholar]


