Teaching clinical reasoning is an essential part of medical education. The methods used to teach clinical reasoning are varied, and the learner, teacher, context, and material all play an important role [1]. Here, the focus is on the use of mnemonic devices. After a brief discussion of teaching clinical reasoning and cognitive load theory, we share a mnemonic for remembering the structure-function relationship of the most common cognitive and other neuropsychiatric syndromes following traumatic brain injury (TBI) and their underlying neuroanatomical correlates: “Up is Down, Down is Up, Middle is Flat.”
Teaching Clinical Reasoning and Cognitive Load Theory
In psychiatry residency, as in all other specialties, considerable effort goes into teaching clinical reasoning. The clinical reasoning process is perhaps most simply defined as “including the physician’s integration of his/her own (biomedical and clinical) knowledge with initial patient information to form a case representation of the problem” [2]. There is considerable evidence that teaching clinical reasoning is highly content and context specific [1]. This means that solving a clinical problem in one medical discipline (e.g., surgery) does not predict ability to solve a problem in another area (e.g., psychiatry). In other words, research has consistently shown that clinical reasoning as a skill is not generalizable and that reasoning skills and critical thinking are perhaps less important than knowledge acquisition [2].
Cognitive load theory (CLT) suggests that the human brain is only able to process a certain amount of information at one time [1]. Classic teaching is that the human cognitive system has a limited working memory that can hold no more than five to nine information elements and actively process no more than two to four elements simultaneously [4]. CLT divides working memory load into the complexity of the information itself (intrinsic load) and the brain resources required to process the information (extrinsic load). Extrinsic load is further subdivided into the cognitive work of organizing new information into schemas (germane load) and the effort required to process new information due to the way in which it is presented (extraneous load) [3, 4]. Learning strategies based on CLT aim to prevent “overload” by decreasing extraneous load, managing intrinsic load, and optimizing germane load [4]. Although numerous teaching strategies exist based on this paradigm [4], here we discuss the use of mnemonics.
Mnemonic Devices
A mnemonic device is any learning technique that aids information retention. The goal is to encode information for easier and more efficient storage and retrieval [5]. There are numerous mnemonic types. Some common examples include: music mnemonics (e.g., singing the alphabet), name mnemonics (e.g., ROY G. BIV for the colors of the rainbow), expression or word mnemonics (e.g., My Very Educated Mother Just Showed Us Nine planets for the order of the planets from the sun), and image mnemonics (e.g., creating a mental image to remember a list of words). The planet mnemonic is an interesting example of what happens when knowledge changes, as Pluto is no longer a planet, but the “p” in “planet” is still part of the mnemonic. Within the CLT framework, there is empirical support for the use of mnemonics for optimization of germane load, a method for decreasing “overload” as described above [6].
Mnemonics devices are widely used in medicine and psychiatry is no exception. Perhaps one of the most widely taught mnemonics is the “SIGECAPS” mnemonic, developed by Dr. Carey Gross, to assist in remembering the eight neurovegetative symptoms of depression [7]. These symptoms are sleep (increased or decreased), interest (decreased), guilt (increased), energy (decreased), concentration (decreased), appetite (increased or decreased), psychomotor (decreased), and suicidal thoughts (increased). Although many residents know it as a name or word mnemonic, it was originally developed as an expression mnemonic referring to the prescription one might write for a depressed, anergic patient: SIG: Energy CAPSules. Additionally, numerous mnemonics have been developed for the Diagnostic and Statistical Manual (DSM) criteria for psychiatric disorders and substance-related disorders [8, 9, 10]. Similar to the planet / Pluto example above, criteria-based mnemonics may prove troublesome as criteria may change over time.
Below, we describe a novel expression mnemonic for remembering the structure-function relationship of the most common cognitive and other neuropsychiatric syndromes following traumatic brain injury (TBI) and their underlying neuroanatomical correlates. The relationship among mental life, behavior, neurologic symptoms, and brain disease is at the center of neuropsychiatric inquiry. An understanding of basic, and at times complex, brain circuitry is necessary. Brain circuitry and neuroanatomy represent just one aspect of a psychiatry resident’s training. Neuroanatomic correlates of psychiatric symptoms can be difficult to remember, and we feel a mnemonic is a welcome addition.
TBI and Neuroanatomy: Up is Down, Down is Up, Middle is Flat
The most recent consensus definition of TBI is that proposed by the Demographics and Clinical Assessment Working Group of the International and Interagency Initiative towards Common Data Elements for Research on Traumatic Brain Injury and Psychological Health, which posits TBI as “an alteration in brain function, or other evidence of brain pathology, caused by an external force [11].” Each year in the United States alone, it is estimated that up to 2.5 million civilians suffer TBI with approximately 5.3 million Americans living with a TBI-related disability, costing the nation over $76 billion in annual direct and indirect medical costs [12]. Cognitive, emotional, behavioral, neurological, and physical impairments are common sequelae of TBI, with some studies showing ~80% of individuals with TBI experiencing at least one neuropsychiatric symptom [13]. Here, the focus is on the most commonly affected neural circuits after TBI, and their associated presenting syndromes.
In actuality, almost any region of the brain could be damaged by trauma. However, certain brain regions are especially vulnerable to injury after TBI and are consistently associated with syndromal presentations. These include the frontal-subcortical networks. Although not discussed here, the rostral brainstem and temporal lobes are other vulnerable regions to consider.
Frontal-Subcortical Circuits
An understanding of frontal-subcortical circuitry is essential for a discussion of the most common syndromal manifestations after TBI. These circuits are intimately involved in regulating higher cerebral processes that control cognition (e.g., attention, planning, decision-making), behavior, and emotion [14]. The concept of parallel, segregated cortico-striatal-thalamic loops was originally proposed by Alexander et al. [15], and these loops have been implicated in several neurologic and psychiatric disorders. Two of these loops are related to motor function and influence musculoskeletal and oculomotor areas of the cortex [14]. The three cortico-striatal-thalamic loops relevant to the neuropsychiatric syndromes seen after TBI originate in the (1) dorsolateral prefrontal cortex, (2) lateral orbitofrontal cortex, and (3) anterior cingulate / medial orbitofrontal cortex and project to different areas of the basal ganglia.
“Up is Down:” The Dorsolateral Prefrontal Loop and Dysexecutive Syndrome
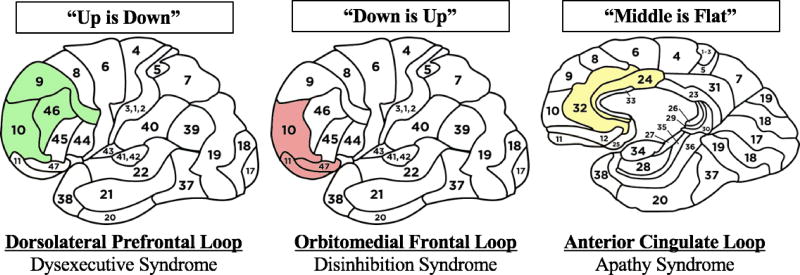
A circuit arising in the dorsal (upper) and lateral (outer) part of the frontal lobes, the dorsolateral prefrontal circuit (Figure 1), is associated with modulating cognitive processes including working memory (transient ability to hold, process, and manipulate information) and executive functions (planning, organizing, decision-making, and problem-solving) [16]. The associated regions correlate approximately with Brodmann’s areas 9, 10, and 46. This circuit’s loop runs as follows: dorsolateral prefrontal cortex → dorsolateral caudate nucleus → globus pallidus → ventral anterior and mediodorsal thalamus → dorsolateral prefrontal cortex [14]. Disruption of this circuit results in the dysexecutive syndrome, in which the brain’s ability to act as an executive is down, akin to what is observed in other disorders like depression, normal pressure hydrocephalus, and vascular dementia. These patients may have trouble with retrieving memories or other stored information, generating word lists, set-shifting, planning out a complex task, ignoring distracting stimuli, alternating between tasks, manipulating abstractions, and inhibiting reflexive responses [17]. “Up is Down” is our mnemonic for remembering that damage to this upper portion of the frontal lobes results in a decrease in the brain’s ability to act as an executive.
Figure 1.
The Neuroanatomic Correlates of Syndromal Presentations after Traumatic Brain Injury
“Down is Up:” The Orbitomedial Frontal Loop and Disinhibition Syndrome
A second circuit arising in the ventral (lower) and outer part of the frontal lobes, the orbitofrontal circuit (Figure 1), is described as the “neocortical representation of the limbic system” and is involved in determining the appropriate time, place, and strategy for environmentally-elicited behavioral responses [14]. The orbitofrontal cortex is divided into lateral orbitofrontal cortex, involved in evaluating and learning from negative experiences, and ventromedial prefrontal cortex, involved in evaluated and learning from rewarding experiences. Together, this is referred to as the orbitomedial prefrontal cortex. Overall, the orbitofrontal circuit plays a critical role in monitoring and integrating external sensory inputs and internal affective states, hence guiding intuitive social behaviors and the capacity to self-monitor and self-correct in real time within a social context [16]. The associated regions correlate approximately with Brodmann’s areas 10, 11, and 47. This circuit’s loop runs as follows: orbitofrontal cortex → ventral striatum (ventromedial caudate and putamen, medial nucleus accumbens) → ventral pallidum → mediodorsal thalamus → orbitofrontal cortex [14]. Disruption to this circuit results in the disinhibition syndrome, in which the number of inappropriate behaviors is up. Example symptoms include increased emotional lability, impulsivity, and lack of social tact. These patients may display behaviors similar to the mania of bipolar disorder, the inattention of ADHD, the sociopathy of antisocial personality, the irritability of borderline personality, and the compulsivity associated with substance abuse [17]. “Down is Up” is our mnemonic for remembering that damage to this lower portion of the frontal lobes results in an increase in inappropriate social behaviors.
“Middle is Flat:” The Anterior Cingulate Loop and Apathy Syndrome
A final circuit arising in the medial (middle) frontal lobes, dorsal and anterior to the corpus callosum, the anterior cingulate circuit (Figure 1), modulates motivated and reward-related behaviors [16]. The associated regions correlate approximately with Brodmann’s areas 24 and 32. This circuit’s loop runs as follows: anterior cingulate cortex → mid-caudate and putamen → medial globus pallidus → mediodorsal thalamus → anterior cingulate cortex [14]. Disruption to this circuit results in the apathy syndrome, which refers to global loss (flattening) of motivation and emotional responsivity, and hence reduced goal-directed behaviors [14]. These patients may present without emotion, and do not experience desire, passion, or motivation [17]. “Middle is Flat” is our mnemonic for remembering that damage to this medial portion of the frontal lobes results in flattening of emotions and behaviors.
Conclusion
Acquisition of clinical knowledge is an essential part of developing clinical reasoning. Having strong reasoning and critical thinking skills is simply not enough. Within the CLT framework, mnemonics work by optimizing germane load. As an example, here we presented a mnemonic for remembering the neuroanatomic location of the circuits damaged in the most common cognitive and other neuropsychiatric syndromes after TBI. We recommend the “Wizard of Oz” approach articulated by Quinn and Katzman [17] for remembering descriptions of these syndromes. Knowledge of these syndromes and the associated circuits is important to any physician treating patients with TBI. Overlapping syndromes may present due to damage to more than one frontal-subcortical circuit (e.g., disinhibition and apathy) and comprehensive neuropsychiatric evaluation can help in identifying the predominant syndrome. In the future, neuromodulation strategies (e.g., transcranial magnetic stimulation, deep brain stimulation) may be able to target and recalibrate specific neuronal circuits.
Acknowledgments
n/a
Grant Support: During this project, Dr. Peters received the following NRSA training grant – T32AG027668
Footnotes
Compliance with Ethical Standards: no human subjects or animals were involved in this work, all ethical and academic standards were followed by all authors
Ethical Considerations: n/a
One behalf of all authors, the corresponding authors states there is no conflict of interest.
References
- 1.Gooding HC, Mann K, Armstrong E. Twelve tips for applying the science of learning to health professions education. Med Teach. 2016;29(1):26–31. doi: 10.1080/0142159X.2016.1231913. [DOI] [PubMed] [Google Scholar]
- 2.Gruppen LD. Clinical Reasoning: Defining it, teaching it, assessing it, studying it. West J Emerg Med. 2017;18(1):4–7. doi: 10.5811/westjem.2016.11.33191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sweller J, van Merrienboer JJ, Paas FGWC. Cognitive architecture and instructional design. Educ Psychol Rev. 1998;10:251–296. [Google Scholar]
- 4.van Merrienboer JJ, Sweller J. Cognitive load theory in health professional education: design principles and strategies. Med Educ. 2010;44(1):85–93. doi: 10.1111/j.1365-2923.2009.03498.x. [DOI] [PubMed] [Google Scholar]
- 5.Mostafa EA, El Midany AAH. Review of mnemonic devices and their applications in cardiothoracic surgery. Journal of the Egyptian Society of Cardio-Thoracic Surgery. 2017;25(79–90) [Google Scholar]
- 6.Wolfe JM. Asymmetries in visual search: An Introduction. Percept Psychophys. 2001;63(3):381–389. doi: 10.3758/bf03194406. [DOI] [PubMed] [Google Scholar]
- 7.Carlat DJ. The Psychiatric Review of Symptoms: A Screening Tool for Family Physicians. Am Fam Physician. 1998;58(7):1617–1624. [PubMed] [Google Scholar]
- 8.Keshavan MS. Mnemonics for DSM-IV. Part I. Diagnostic criteria and psychiatric assessments. Asian J Psychiatr. 2009;2(3):117–118. doi: 10.1016/j.ajp.2009.09.002. [DOI] [PubMed] [Google Scholar]
- 9.Keshavan MS. Mnemonics for DSM-IV. Part II. Asian J Psychiatr. 2010;3(1):41–42. doi: 10.1016/j.ajp.2010.01.001. [DOI] [PubMed] [Google Scholar]
- 10.Pinkofksy HB, Reeves RR. Mnemonics for DSM-IV substance-related disorders. Gen Hosp Psychiatry. 1998;20(6):368–370. doi: 10.1016/s0163-8343(98)00052-8. [DOI] [PubMed] [Google Scholar]
- 11.Menon DK, Schwab K, Wright DW, et al. Position statement: Definition of traumatic brain injury. Arch Phys Med Rehabil. 2010;91(11):1637–1640. doi: 10.1016/j.apmr.2010.05.017. [DOI] [PubMed] [Google Scholar]
- 12.Coronado VG, McGuire LC, Faul MF, Sugerman DE, Pearson WS. In: Traumatic brain injury epidemiology and public health issues. Zasler ND, Katz DI, Zafonte RD, editors. New York, NY: Demos Medical Publishing; 2012. pp. 84–100. [Google Scholar]
- 13.Kim E, Lauterbach EC, Reeve A, et al. Neuropsychiatric complications of traumatic brain injury: A critical review of the literature (a report by the ANPA committee on research) J Neuropsychiatry Clin Neurosci. 2007;19(2):106–127. doi: 10.1176/jnp.2007.19.2.106. [DOI] [PubMed] [Google Scholar]
- 14.Bonelli RM, Cummings JL. Frontal-subcortical circuitry and behavior. Dialogues Clin Neurosci. 2007;9(2):141–151. doi: 10.31887/DCNS.2007.9.2/rbonelli. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Alexander GE, Crutcher MD, DeLong MR. Basal ganglia-thalamocortical circuits: Parallel substrates for motor, oculomotor, "prefrontal" and "limbic" functions. Prog Brain Res. 1990;85:119–146. [PubMed] [Google Scholar]
- 16.McAllister TW. Neurobiological consequences of traumatic brain injury. Dialogues Clin Neurosci. 2011;13(3):287–300. doi: 10.31887/DCNS.2011.13.2/tmcallister. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Quinn D, Katzman J. "The wizard of oz:" A depiction of TBI-related neurobehavioral syndromes. Acad Psychiatry. 2012;36(4):340–344. doi: 10.1176/appi.ap.11010014. [DOI] [PubMed] [Google Scholar]