Abstract
We examined differences in complication rates between obese and non-obese patients undergoing revision total hip arthroplasty. Sixty-five patients with a BMI ≥30 kg/m2 and 54 patients with a BMI of <30 kg/m2 were identified. Obese patients were 2.5 times more likely to suffer a complication than non-obese (38.4% cf 14.8%, p = 0.02). Obese patients were more likely to experience dislocation, leg length discrepancy, fracture, implant loosening, infection and pulmonary embolus. The obese group had a significantly higher revision rate (12.3% cf 1.8%, p = 0.039). Obese patients should be counselled pre-operatively on their elevated risk.
Keywords: Revision hip arthroplasty, Obesity, Complications
1. Introduction
Obesity is becoming increasingly prevalent1 and is associated with multiple other conditions including coronary artery disease and hypertension.2 Furthermore, osteoarthritis of the hip is common in these patients, many of who will subsequently undergo total hip arthroplasty (THA). Despite improved functional status post-operatively, obese patients generally do not lose weight.3 Although obese patients have greater forces acting across their hips due to increased weight, previous revision rates have been reported to be comparable with non-obese patients.4 This may be due to the associated lower activity levels. As the number of primary THA being performed increases, revision rates will also rise, with many of these procedures being performed in obese patients. Revision THA involves greater operative time, higher blood loss and a greater number of complications.5 Obesity has been associated with higher complication rates including periprosthetic joint infection6 and respiratory compromise.7 The effects of obesity on outcomes of revision THA are uncertain given the paucity of evidence within the literature. The few studies existing have reported functional outcomes and satisfaction to improve significantly post-operatively, and often be either comparable or only slightly lower in obese patients compared to non-obese.4, 8 However, variability in complication rates are not well understood with wide disparities reported. This may be a result of these studies having small patient cohorts4, 5, 8 and variable body mass index (BMI) categorisations of obesity.5 This therefore limits our ability to adequately inform obese patients of appropriate complication rates. This study aimed to establish the complication rate in obese patients undergoing revision THA and determine if this differs from a non-obese group.
2. Methods
Two cohorts were identified with a mean BMI difference of 9 kg/m2 over a 10 year period. The records of our prospectively collected arthroplasty database were reviewed to identify patients undergoing revision THA between 2005 and 2015. All procedures were performed at a single tertiary referral unit with follow-up at regular intervals for life. Two hundred and eighteen patients were available for review. Patients undergoing revision for infection, periprosthetic fracture, recurrent dislocations and hip resurfacing failure were excluded to provide a more homogeneous group. Hip resurfacing failure was excluded given the potential for extensive soft tissue damage as a result of adverse reactions to metal debris. Infection cases were excluded based on pre-operative work-up and intra-operative tissue sampling. This left 119 patients for analysis. A power calculation was performed which determined 114 patients were required to produce a power of 0.8. Our sample size was therefore sufficient to adequately power the study. All cases were revisions of primary THA. BMI as calculated by weight (kg)/height (m)2 was documented for all patients. Obesity was defined by a BMI ≥30 kg/m2.9 An age, gender and American Society of Anesthesiologists (ASA) score matched comparator group was established consisting of patients with a BMI <30 kg/m2 performed during the same time period and with the same pre-operative diagnoses as the obese group. All complications were recorded in our arthroplasty database by independent practitioners. Documentation in the database was rigorous and we therefore only presented complications graded 2 and above based on the classification by Dindo et al10 which excludes any problems treated with antiemetics, antipyretics, analgesics, diuretics, electrolytes or physiotherapy. Radiographic analysis was performed on annual anteroposterior and lateral radiographs for implant loosening and failure.
2.1. Statistical analysis
Survival analysis was done to determine the predictors of complications with age, gender, ASA score and BMI as possible predictors. Fisher’s exact test was used to test for an association between obesity and the need for a further revision operation. All analyses were done using SPSS (version 22).
3. Results
Sixty five patients with a BMI ≥30 kg/m2 and 54 patients with a BMI of <30 kg/m2 were identified. Patient demographics of both groups are presented in Table 1. Reasons for revision are presented in Fig. 1. Mean follow-up period was 3.6 years (range 1–11.1) for the obese group and 2.8 (range 1–11.1) for the non-obese.
Table 1.
Patient demographics of obese and non-obese groups.
| Obese | Non-obese | |
|---|---|---|
| Mean BMI (kg/m2) | 34 (range 30–44) | 25 (range 16–29) |
| Mean age | 67 | 70 |
| Male:female | 1:1.2 | 1:1.1 |
| Median ASA | 2 | 2 |
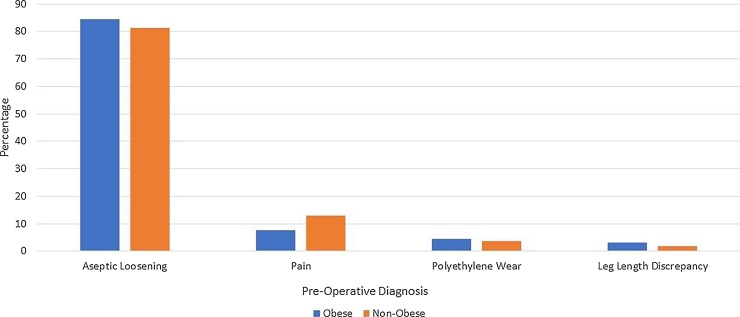
Fig. 1.
Reason for revision in both groups. There was a comparable spread of pre-operative diagnoses between the obese and non-obese group.
The obese group experienced 27 complications in 25 patients (38.4%). Eight patients (12.3%) underwent further revision surgery at a mean of 1.9 years post-operative. Reasons for further revision were recurrent dislocation (n = 4), periprosthetic fracture (n = 3) and infection (n = 1). One patient who underwent a second revision for periprosthetic infection developed a deep infection requiring a Girdlestone procedure. Two patients (3.1%) died at 1.5 and 6.9 years post-operative for causes unrelated to their surgery.
The non-obese group had eight complications in eight patients (14.8%). One patient (1.8%) underwent a further revision following a periprosthetic fracture. There were four deaths (7.4%) between 1.3 and 3.5 years post-operative for causes unrelated to surgery.
Complications are listed in Table 2. The obese group suffered higher rates of dislocation, leg length discrepancy, fracture, implant loosening, periprosthetic joint infection and pulmonary embolus. The difference in complication rate (p = 0.02) and revision rate (p = 0.039) was statistically significant. No difference in individual complication, e.g. dislocation, reached statistical significance due to small numbers. There was no association between obesity and death (p = 0.208). There was evidence of an association between higher ASA scores and complication rate (p = 0.009). Age (p = 0.454), gender (p = 0.651) and pre-operative diagnosis (p = 0.588) were not predictive of a complication.
Table 2.
Complication rates by group.
| Complication | Obese (%) | Non-obese (%) |
|---|---|---|
| Dislocation | 11 (16.9) | 3 (5.5) |
| Leg length discrepancy | 2 (3.0) | 0.0 |
| Implant loosening | 3 (4.6) | 2 (3.7) |
| Periprosthetic fracture | 4 (6.1) | 1 (1.8) |
| Intra-operative fracture | 4 (6.1) | 0.0 |
| Pulmonary embolus | 2 (3.0) | 0.0 |
| Periprosthetic joint infection | 1 (1.5) | 0.0 |
| Nerve injury | 0.0 | 2 (3.7) |
4. Discussion
Obesity represents a growing healthcare problem globally. Equally, the number of primary and revision hip arthroplasties being performed has been increasing over time.11 It is therefore crucial that we have a clear understanding of the impact of increased BMI on morbidity following joint replacement. This is particularly relevant in the National Health Service where recent discussions have suggested health boards may delay offering hip and knee arthroplasty to patients with an increased BMI. Previous studies have reviewed the effect of increased BMI in primary THA12 demonstrating a higher risk of early complications in the obese. At present, there is only limited and contradictory evidence relating to the role of obesity in revision arthroplasty. To our knowledge, this study represents the largest cohort of obese revision THA patients and demonstrates that this group have a significantly higher complication rate and are more likely to require a further revision when compared to non-obese individuals.
Revision THA can successfully restore function and reduce pain in cases of failed primary hip arthroplasty. However, it has been shown to have greater operative time, blood loss4 and key complications including dislocation13 and infection. We report a dislocation rate of 16.9% in obese patients, compared to 5.5% in the non-obese. This higher rate was also noted by Kim et al4 who proposed this was related to extraarticular soft tissue impingement during hip adduction and flexion. The authors recommended large diameter femoral heads to reduce the risk of dislocation. Given the larger soft tissue dissection generally required in obese patients, Lübbeke et al8 also proposed muscle weakness as a responsible factor for higher dislocation rates. In contrast to these studies, Perka et al5 found only an increase in operative time, with no difference in complication rates or mortality between obese and non-obese patients. This study included patients with a BMI of 25–29.9 kg/m2 in the obese category, however, in contrast to the World Health Organisations definition of ≥30 kg/m2 9 which may have influenced their results.
Performing revision THA is more technically challenging than primary hip arthroplasty. Obesity can further increase the complexity of the procedure owing to difficulties with exposure, implant position and closure. Such difficulties may in turn be responsible for higher complications. In our study, we found higher rates of intra-operative fracture, leg length discrepancy and periprosthetic joint infection, all of which may be related to technical challenges. Higher post-operative infection rates were also demonstrated by Houdek et al14. This may result from associated comorbidities, prolonged operative time, greater trauma from exposure and relative immune deficiency. Weight loss has the potential to correct some of these factors15 and so represents an important factor in risk stratification.
In the context of recurrent dislocation, infection and periprosthetic fracture, there is a clear case for early revision regardless of BMI. However, in the population we studied, consisting mainly of aseptic loosening, the timing of surgery may be less urgent. Given that this study has demonstrated a higher complication rate in obese patients, postponing surgery to facilitate weight loss may be justified. At the least, obese patients should be counselled that they are 2.5 times more likely to experience a complication than non-obese individuals.
There are limitations to our study. Firstly, our sample size was not large. Our data was obtained from a tertiary referral centre over a 10 year period to maximise the number of available obese patients for inclusion however we were only able to obtain 65 patients. This may lead to other factors such as comorbidities influencing the results. However, this prospectively collected arthroplasty database provided gender, age, ASA score and pre-operative diagnosis matched cohorts. The follow-up period was also relatively short which may have resulted in late complications not being identified for all patients. However, this factor was adjusted for in the statistical analysis and the majority of complications following hip arthroplasty tend to occur early.12
5. Conclusion
Although revision THA can successfully manage a failed primary hip arthroplasty, obese patients who undergo this procedure can expect higher complication rates, particularly dislocation, and revision rates when compared to a non-obese cohort. Obese patients should be counselled on these risks pre-operatively and the potential benefits of weight loss.
Conflict of interest
None.
Acknowledgments
The authors would like to thank the orthopaedic outpatient department and audit team for their contribution.
References
- 1.Rennie K.L., Jebb S.A. Prevalence of obesity in Great Britain. Obes Rev. 2005;6:11–12. doi: 10.1111/j.1467-789X.2005.00164.x. [DOI] [PubMed] [Google Scholar]
- 2.National Institutes of Health consensus development conference statement Health implications of obesity. Ann Intern Med. 1985;103:977–1077. [PubMed] [Google Scholar]
- 3.Heisel C., Silva M., dela Rosa M.A., Schmalzried T.P. The effects of lower-extremity total joint replacement for arthritis on obesity. Orthopaedics. 2005;28:157–159. doi: 10.3928/0147-7447-20050201-18. [DOI] [PubMed] [Google Scholar]
- 4.Kim Y., Morshed S., Joseph T., Bozic K., Ries M.D. Clinical impact of obesity on stability following revision total hip arthroplasty. Clin Orthop Relat Res. 2006;453:142–146. doi: 10.1097/01.blo.0000238874.09390.a1. [DOI] [PubMed] [Google Scholar]
- 5.Perka C., Labs K., Muschik M., Buttgereit F. The influence of obesity on perioperative morbidity and mortality in revision total hip arthroplasty. Arch Orthop Trauma Surg. 2000;120 doi: 10.1007/s004020050462. [DOI] [PubMed] [Google Scholar]
- 6.Jämsen E., Nevalainen P., Eskelinen A., Huotari K., Kalliovalkama J., Moilanen T. Obesity, diabetes, and preoperative hyperglycemia as predictors of periprosthetic joint infection: a single-center analysis of 7181 primary hip and knee replacements for osteoarthritis. J Bone Joint Surg Am. 2012;18(94):e101. doi: 10.2106/JBJS.J.01935. [DOI] [PubMed] [Google Scholar]
- 7.Damia G., Mascheroni D., Croci M., Tarenzi L. Perioperative changes in functional residual capacity in morbidly obese patients. Br J Anaesth. 1988;60:574–578. doi: 10.1093/bja/60.5.574. [DOI] [PubMed] [Google Scholar]
- 8.Lübbeke A., Moons K.G., Garavaglia G., Hoffmeyer P. Outcomes of obese and nonobese patients undergoing revision total hip arthroplasty. Arthritis Rheum. 2008;59:738–745. doi: 10.1002/art.23562. [DOI] [PubMed] [Google Scholar]
- 9.World Health Organisation . Vol. 894. 2000. Obesity: preventing and managing the global epidemic : report of a WHO consultation. (WHO Technical Report Series). [PubMed] [Google Scholar]
- 10.Dindo D., Demartines N., Clavien P.A. Classification of surgical complications. A new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–213. doi: 10.1097/01.sla.0000133083.54934.ae. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kurtz S., Ong K., Lau E., Mowat F., Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89:780–785. doi: 10.2106/JBJS.F.00222. [DOI] [PubMed] [Google Scholar]
- 12.Lehman D.E., Capello W.N., Feinberg J.R. Total hip arthroplasty without cement in obese patients. A minimum two-year clinical and radiographic follow-up study. J Bone Joint Surg Am. 1994;76:854–862. doi: 10.2106/00004623-199406000-00009. [DOI] [PubMed] [Google Scholar]
- 13.Alberton G.M., High W.A., Morrey B.F. Dislocation after revision total hip arthroplasty: an analysis of risk factors and treatment options. J Bone Joint Surg Am. 2002;84-A:1788–1792. [PubMed] [Google Scholar]
- 14.Houdek M.T., Wagner E.R., Watts C.D. Morbid obesity: a significant risk factor for failure of two-stage revision total hip arthroplasty for infection. J Bone Joint Surg Am. 2015;97:326–332. doi: 10.2106/JBJS.N.00515. [DOI] [PubMed] [Google Scholar]
- 15.Fontana L., Eagon J.C., Colonna M., Klein S. Impaired mononuclear cell immune function in extreme obesity is corrected by weight loss. Rejuvenation Res. 2007;10:41–46. doi: 10.1089/rej.2006.0504. [DOI] [PubMed] [Google Scholar]