Abstract
Purpose
The relationship between chronic smoking history and postoperative pain remains controversial. This study aimed to elucidate this relationship in non-small cell lung cancer (NSCLC) patients who underwent video-assisted thoracic surgery (VATS) lobectomy.
Patients and methods
This retrospective observational study included NSCLC patients treated with VATS lobectomy between January 2011 and July 2017. Demographic and clinical information, including preoperative smoking history, was collected. The primary goal was to investigate the relationship between smoking history and postoperative pain outcomes (oral morphine equivalent [OME] consumption and pain score). Multivariate linear regression analysis was performed, and P<0.05 was considered as statistically significant.
Results
A total of 1,785 patients were included in the final analysis. Multivariate linear regression analysis revealed that total smoking amount (in packs), status as current smoker, and cessation time did not have an association with OME consumption (mg) or pain scores on postoperative days 0–2 (P>0.05). However, patients who had never smoked consumed less morphine equivalent analgesics (mg) on postoperative days 0–2 (coefficient: −17.48, 95% CI [−33.83, −1.13], P=0.036) compared to patients who had a history of smoking.
Conclusion
Patients who had never smoked had lower opioid analgesics consumption on the days immediately following surgery, while being a current smoker or the total amount of smoking in packs did not affect postoperative pain outcomes after VATS lung lobectomy.
Keywords: anesthesia, analgesia, opioid, postoperative pain, smoking
Introduction
The causative role of smoking in lung cancer and poor outcomes in patients with lung cancer have been well documented.1 Thereby, the prevalence of smoking is high among patients diagnosed with lung cancer,2 and following cancer surgery, smokers have worse outcomes than nonsmokers because of greater postoperative complications.3,4 Moreover, since previous studies suggest that acute or chronic exposure to cigarette smoke affects acute and chronic painful conditions,5 further caution needs to be exercised when providing perioperative care to patients with a smoking history and efficient strategies are needed for postoperative pain control.6
Chronic exposure to nicotine is a known risk factor for chronic painful conditions,7 and it may modulate pain perception.8,9 This effect is explained by the desensitization of the nicotine acetylcholine receptor, which develops after continuous exposure to nicotine.10,11 A previous study conducted in 201012,13 described the development of pain intolerance in nicotine-tolerant rats, when compared with nicotine-naïve rats, as a model for the effects of chronic smoking, suggesting that chronic smokers might be less tolerant to pain than nonsmokers because of hyperalgesia. Indeed, recent studies have revealed that the intensity of back pain14 or pain caused by temporomandibular joint disorders15 or major surgery16 is more severe in smokers than in nonsmokers.
However, additional data are required to validate these hypotheses. In particular, studies that analyzed the association between smoking history and pain outcome in patients after lung cancer surgery are lacking, despite the potential critical effect of smoking history on pain. Therefore, the objective of this study was to determine the effects of smoking history on postoperative pain in non-small cell lung cancer (NSCLC) patients who underwent video-assisted thoracic surgery (VATS) lobectomy. We hypothesized that postoperative pain outcomes would be worse in smokers than in nonsmokers.
Patients and methods
This study was conducted by reviewing the medical records of adult patients aged ≥19 years who were diagnosed with NSCLC and treated with VATS lobectomy between January 1, 2011 and July 31, 2017. Exclusion criteria were as follows: patients who underwent another surgery within 2 days after the VATS lobectomy; intraoperative conversion to open thoracotomy, bilobectomy, or pneumonectomy; inaccurate or missing records related to pain outcomes; administration of thoracic epidural analgesia; and the requirement of interdisciplinary cooperation for combined resection of the extrathoracic organs. In addition, while we included patients who had undergone a single lobectomy or sublobar resection of another lobe in the affected lung, we excluded those who had undergone sublobar resection in the contralateral lung in addition to lobectomy.
VATS lobectomy and anesthetic care
At the hospital, lobectomy is routinely performed by an experienced thoracic surgery team using VATS techniques.17 Anesthesiologists provide anesthetic management based on standardized anesthetic techniques. In general, remifentanil infusion was used intraoperatively, and fentanyl-based intravenous patient-controlled anesthesia was used after surgery. In addition to intravenous patient-controlled anesthesia, additional opioid medications were used for pain management upon patient’s request and according to physician’s judgment. Neither nonsteroidal anti-inflammatory drugs nor acetaminophen was used for pain relief.
Measurement and outcome
Patient data collected included the following: patient sex, age, height, and weight; histologic type of NSCLC; American Society of Anesthesiologists classification; admission to postoperative intensive care; use of adjuvant chemotherapy or radiotherapy; history of hypertension, diabetes mellitus, neurologic disease, or ischemic heart disease; surgery duration; length of hospital stay; smoking history (average number of cigarettes smoked per day, duration of smoking); opioid consumption; and pain scores on postoperative days (PODs) 0–2.
Patients were divided into three groups on the basis of their smoking history: 1) current smoker: those who continued smoking within 1 month before surgery; 2) never smoker: those who had never smoked; and 3) ex-smoker: those who stopped smoking before surgery. Cessation time for ex-smokers was divided into three categories (<1 month, 1 month–1 year, and >1 year). Total lifetime smoking amount in packs was calculated for the current smoker and ex-smoker groups.
Total opioid consumption was calculated as the sum of opioid medications administered on PODs 0, 1, and 2, calculated using standard conversion ratios and expressed in milligrams of oral morphine equivalent (OME),18 as shown in Table S1. A Numeric Rating Scale (NRS) was used to quantify pain intensity. During the study period, postoperative pain intensity was measured more than five times per day by nurses using the NRS, and the average of all scores measured in 1 day was defined as the daily NRS score. All medical record data were collected by technicians in the Medical Informatics team who were blinded to the study purpose. Moreover, the primary researchers were blinded to the data before statistical outcomes became available.
The primary purpose of this study was to identify any differences in pain outcome (postoperative NRS score on PODs 0, 1, and 2 and OME for PODs 0–2) according to smoking history.
Statistical methods
Baseline characteristics are presented as number with percentage or mean with SD (Table 1). We performed a univariate linear regression analysis for OME consumption on PODs 0–2 after VATS lung lobectomy. The variables with P<0.2 were selected and included in the first multivariate linear regression model (Model 1). Next, backward variable selection method with an elimination criterion of P<0.1 was performed to fit the second multivariate linear regression model (Model 2). IBM SPSS software (version 23.0; IBM Corp., Armonk, NY, USA) was used for statistical analysis, and P<0.05 was considered statistically significant.
Table 1.
Distribution for patient characteristics
| Characteristics (total=1,785 patients) | Number (%)or mean (SD) |
|---|---|
| Total | 1,785 |
| Age (years) | 63.5 (11.8) |
| Body mass index (kg m−2) | 23.9 (11.8) |
| Length of hospital stay (days) | 9.0 (14.9) |
| ASA class | |
| 1 | 434 (24.3) |
| 2+3 | 1,351 (75.7) |
| Preoperative comorbidity | |
| Hypertension | 567 (31.8) |
| Diabetes mellitus | 246 (13.8) |
| Neurologic disease | 153 (8.6) |
| Ischemic heart disease | 145 (8.1) |
| Psychiatric disorder | 18 (1.0) |
| Preoperative smoking information | |
| Current smoker | 161 (9.0) |
| Never smoker | 882 (49.4) |
| Ex-smoker | 742 (41.6) |
| Cessation time | |
| <1 month | 121 (6.8) |
| 1 month–1 year | 115 (6.4) |
| >1 year | 506 (28.3) |
| Total smoking amount in life (packs) | 10,968 (7,827) |
| Morphine equivalent (mg) in POD 0–2 | 515.5 (523.5) |
| Postoperative NRS pain score | |
| POD 0 | 4.7 (1.2) |
| POD 1 | 3.0 (1.0) |
| POD 2 | 2.5 (0.9) |
Abbreviations: ASA, American Society of Anesthesiologists; NRS, Numeric Rating Scale; POD, postoperative day.
Ethical approval
This was a retrospective cohort study approved by the Institutional Review Board of the Seoul National University Bundang Hospital (B1708/412-110, approval date: August 29, 2017, Gumi-ro 173 Beon-gil, Bundang-gu, Seongnam-si, Gyeonggi-do, Korea 463-707). Written informed consent was waived as this was a retrospective review of patient medical records, and all patients’ data were anonymized for analysis.
Results
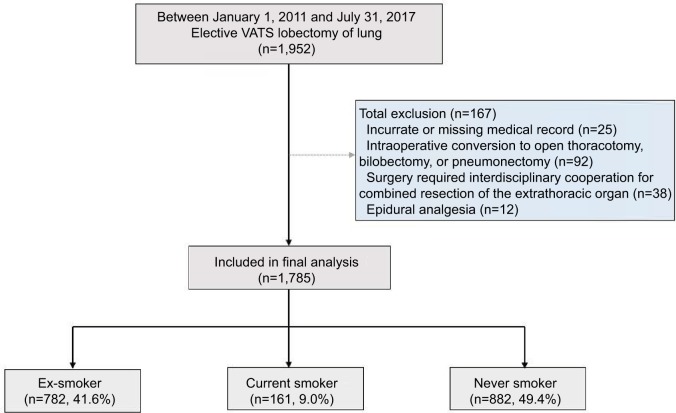
According to the retrospective review, 1,952 patients were diagnosed with NSCLC and treated with elective VATS lobectomy between January 1, 2011 and July 31, 2017. Patients were excluded in the following cases: 1) medical records were inaccurate or missing (n=25); 2) intraoperative conversion to open thoracotomy, bilobectomy, or pneumonectomy (n=92); 3) the surgery required interdisciplinary cooperation for combined resection of the extrathoracic organs (n=38); and 4) epidural analgesia was used (n=12). After applying the exclusion criteria, we included 1,785 patients in the final analysis (Figure 1). Table 1 shows the demographic and clinical characteristics of the 1,785 patients with preoperative smoking data. There were 161 (9.0%) current smokers, 882 (49.4%) never smokers, and 782 (41.6%) ex-smokers. The lifetime number of packs smoked was 10,968±7,827.
Figure 1.
Flow chart for patient selection.
Abbreviation: VATS, video-assisted thoracic surgery.
Postoperative opioid consumption on PODs 0–2 according to smoking history
Table 2 shows the results of a univariate linear regression analysis for OME consumption on PODs 0–2 after VATS lung lobectomy. From the univariate linear regression model, covariates with P<0.2 (sex, body mass index, American Society of Anesthesiologists class, preoperative diabetes mellitus and psychiatric disorder, postoperative intensive care unit admission, surgery time, never smoker, total smoking amount in packs) were included in the multivariate linear regression model (Model 1). After backward selection of variables, with an elimination criterion of P<0.1, never smoker was significantly associated with decreased OME consumption on PODs 0–2 after the lobectomy surgery (coefficient: −17.48, 95% CI [−33.83, −1.13], P=0.036; Table 3). Additionally, surgery time was positively associated with OME consumption on PODs 0–2 after the lobectomy surgery (coefficient: 0.53, 95% CI [0.39, 0.68], P<0.001; Table 3).
Table 2.
Univariate linear regression analysis for oral morphine equivalent (mg) consumption in POD 0–2 after VATS lung lobectomy
| Characteristics | Coefficient (95% CI) | P-value |
|---|---|---|
| Age (years) | −0.42 (−1.11, 0.27) | 0.228 |
| Sex | ||
| Female (vs male) | −23.30 (−39.63, −7.00) | 0.005 |
| Body mass index (kg m−2) | 1.87 (−0.71, 4.45) | 0.155 |
| ASA | ||
| 1 (vs 2–3) | 13.59 (−5.36, 32.54) | 0.160 |
| Preoperative comorbidity | ||
| Hypertension | 3.17 (−14.24, 20.58) | 0.721 |
| Diabetes mellitus | 15.88 (−7.62, 39.38) | 0.185 |
| Neurologic disease | −9.79 (−38.73, 19.16) | 0.507 |
| Ischemic heart disease | −9.10 (−38.77, 20.56) | 0.547 |
| Psychiatric disorder | −64.89 (−145.96, 16.17) | 0.117 |
| Surgery time (min) | 0.56 (0.42, 0.70) | <0.001 |
| Postoperative ICU admission | 44.90 (15.22, 74.59) | 0.003 |
| Preoperative smoking information | ||
| Current smoker (vs non-current smoker) | 14.81 (−13.47, 43.10) | 0.304 |
| Current smoker (vs never smoker) | 16.21 (−12.23, 44.66) | 0.264 |
| Never smoker (vs non-never smoker) | −24.72 (−40.89, −8.55) | 0.003 |
| Cessation time for ex-smoker (1) | ||
| Never smoker | 1 | |
| <1 month | 20.96 (−11.26, 53.19) | 0.202 |
| 1 month–1 year | 10.08 (−22.92, 43.09) | 0.549 |
| >1 year | −16.36 (−47.11, 14.38) | 0.297 |
| Cessation time for ex-smoker (2) | ||
| Current smoker | 1 | |
| 1 month–1 year | −10.11 (−56.13, 35.92) | 0.666 |
| >1 year | −9.80 (−46.03, 26.43) | 0.596 |
| Total smoking amount (packs) | 0.001 (0.000, 0.002) | 0.162 |
Notes: Variables with P<0.2 (bold) were included in the multivariate linear regression analysis in Table 3. Bold figures were variables in criteria with P<0.2, and they were included in multivariate analysis.
Abbreviations: ASA, American Society of Anesthesiologists; ICU, intensive care unit; POD, postoperative day; VATS, video-assisted thoracic surgery.
Table 3.
Multivariate linear regression analysis for morphine equivalent (mg) in POD 0–2 after VATS lung lobectomy
| Variables | Multivariate Model 1
|
Multivariate Model 2
|
||
|---|---|---|---|---|
| Coefficient (95% CI) | P-value | Coefficient (95% CI) | P-value | |
| Sex | ||||
| Female (vs male) | 4.07 (−48.93, 109.18) | 0.455 | ||
| ASA class | ||||
| 1 (vs 2–3) | 10.33 (−9.21, 29.87) | 0.751 | ||
| Preoperative diabetes mellitus | 20.76 (−3.42, 44.95) | 0.092 | 18.23 (−5.16, 41.62) | 0.127 |
| Preoperative psychiatric disorder | −37.83 (−122.63, 46.97) | 0.382 | ||
| Surgery time (min) | 0.55 (0.40, 0.69) | <0.001 | 0.53 (0.39, 0.68) | <0.001 |
| Postoperative ICU admission | 10.74 (−60.68, 42.16) | 0.503 | ||
| Never smoker (vs non-never smoker) | −25.19 (−52.17, 1.80) | 0.067 | −17.48 (−33.83, −1.13) | 0.036 |
| Total smoking amount (packs) | −0.001 (−0.002, 0.001) | 0.327 | ||
Notes: Multivariate Model 1: eight variables with P value <0.2 from the univariate model were included in the multivariable Model 1. Multivariate Model 2: backward variable selection method with an elimination criterion of 0.1 was performed to fit the multivariable model.
Abbreviations: ASA, American Society of Anesthesiologists; ICU, intensive care unit; POD, postoperative day; VATS, video-assisted thoracic surgery.
Postoperative NRS pain score on PODs 0, 1, and 2 according to smoking history
Table 4 shows the results of the multivariate linear regression analysis using backward selection of the variables for postoperative NRS on PODs 0, 1, and 2 after VATS lobectomy. The only significant factor was age for the NRS pain score on POD 0 (coefficient: −0.009, 95% CI [−0.011, −0.003], P=0.004).
Table 4.
Multivariate linear regression using backward variable selection method for postoperative NRS on POD 0, 1, and 2 after VATS lobectomy
| Variables | Coefficient (95% CI) | P-valuea |
|---|---|---|
| NRS pain score on POD 0 | ||
| Age | −0.009 (−0.011, −0.003) | 0.004 |
| Surgery time | 0.001 (0.001, 0.002) | 0.076 |
| Cessation time >1 year (vs never smoker) | −0.21 (−0.43, 0.02) | 0.068 |
| NRS pain score on POD 1 | ||
| Age | 0.001 (−0.001, 0.001) | 0.051 |
| Preoperative ischemic heart disease | 0.19 (0.01, 0.36) | 0.037 |
| Cessation time >1 year (vs never smoker) | −0.23 (−0.41, 0.05) | 0.072 |
| NRS pain score on POD 2 | ||
| Surgery time | 0.001 (0.000, 0.001) | 0.065 |
| Preoperative hypertension | 0.08 (−0.01, 0.17) | 0.074 |
Note:
Backward variable selection method with an elimination was performed to fit the final multivariable model for four dependent variables (NRS on POD 0, 1, and 2).
Abbreviations: NRS, Numeric Rating Scale; POD, postoperative day; VATS, video-assisted thoracic surgery.
Discussion
In this study, we found no significant differences in postoperative pain outcomes, assessed in terms of NRS scores and opioid consumption following VATS lobectomy, according to current smoker, total smoking amount in packs, and smoking cessation time of ex-smokers. However, never smokers showed a 17.48% significant decrease in opioid consumption on PODs 0–2. These findings are meaningful given that this study focused on patients who underwent VATS lobectomy at a single institution, and considering that these lung cancer patients, for whom smoking was the most critical factor, were expected to develop similar levels of pain.
Recent studies reported that current smokers showed an increased pain intensity compared to patients who had never smoked.15,16,19,20 The results of our study are different from these results with respect to current smokers, which showed no increase in postoperative OME consumption on PODs 0–2 or in NRS pain scores for these patients (Table 2). Nicotine withdrawal in current smokers is known to decrease the pain threshold and eventually increase pain intensity,21 which might explain the results of current smokers in this study. However, the effect might be weakened in our study for the following reason. Normally, patients with NSCLC are advised by doctors to stop smoking immediately at the time of cancer diagnosis. When patients require curative resection, they undergo elective surgery several weeks later. If they fail to quit smoking until the day before surgery, the surgery is postponed by several weeks. Rescheduling of the surgery is necessary to ensure safe postoperative management because lung cancer surgery itself is a risk factor for developing postoperative lung injury.4 This rescheduling policy was also implemented in our study. Therefore, the withdrawal effect of nicotine for current smokers could have been weakened, so that no difference in postoperative pain outcomes was observed in our study.
However, never smokers in our study showed better postoperative pain outcomes compared to current and ex-smokers, and to our knowledge, this is the first study reporting these findings. In addition, we showed that the duration from smoking cessation did not affect postoperative pain outcomes after VATS lobectomy, which may also be a novel finding. Never smokers showed less opioid analgesic consumption than non-never smokers and this could be explained by the role of chronic nicotine exposure on intolerance for pain. An animal study revealed pain intolerance and mechanical hyperalgesia in nicotine-tolerant rats, which was explained primarily by elevated levels of spinal dynorphin and cytokines, centrally and peripherally.5 Although our study failed to show a relationship between total smoking amount in packs and postoperative opioid consumption or the NRS pain score on PODs 0–2, there might be an effect of chronic nicotine exposure on intolerance for pain regarding decreased OME consumption of the never smoker group.
Another important issue is that there was no significant effect of cessation time from smoking for ex-smokers on postoperative pain outcomes after VATS lobectomy. There have been no reports that the effect of chronic exposure of nicotine on pain can be eliminated after quitting smoking. On the other hand, there have been reports that cessation of smoking improved postoperative pain scores in patients with spinal disorders.22,23 However, these studies did not consider the relationship to the duration from smoking cessation. Therefore, more studies exploring the relationship between duration from smoking cessation and postoperative pain are needed.
This study has a few limitations. First, the retrospective design may have introduced selection bias. Second, this study was performed in single tertiary care hospital, so generalizability could be insufficient. Third, total OME for PODs 0–2 was calculated by using an opioid conversion factor. Although it is a standard conversion ratio, its accuracy is controversial.24,25
Conclusion
Patients who had never smoked consumed significantly less opioid analgesics on PODs 0–2, while being a current smoker or the total amount of smoking in terms of packs did not affect postoperative pain outcomes after VATS lung lobectomy.
Availability of data and materials
The datasets generated and analyzed during the current study are available from the corresponding author on reasonable request.
Supplementary material
Table S1.
Equianalgesic opioid conversion table
| Opioid | Administration route | Dose equivalent to 10 mg of oral morphine (mg) |
|---|---|---|
| Morphine | Oral | 10 |
| Morphine | Intravenous | 3.3 |
| Hydromorphone | Oral | 2 |
| Fentanyl | Intravenous | 0.03 |
| Oxycodone | Oral | 7 |
| Codeine | Oral | 80 |
| Tramadol | Oral | 40 |
Footnotes
Author contributions
TKO contributed to the study design, analyzed the data, and drafted the first manuscript. KMK, SHJ, SHD, JWH, JHK, and YTJ contributed to the acquisition of data and provided critical revision of the manuscript. IAS contributed to the study design and provided critical revision of the manuscript. All authors contributed toward data analysis, drafting and revising the paper and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Peto R, Darby S, Deo H, Silcocks P, Whitley E, Doll R. Smoking, smoking cessation, and lung cancer in the UK since 1950: combination of national statistics with two case-control studies. BMJ. 2000;321(7257):323–329. doi: 10.1136/bmj.321.7257.323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kawai H, Tada A, Kawahara M, et al. Smoking history before surgery and prognosis in patients with stage IA non-small-cell lung cancer – a multicenter study. Lung Cancer. 2005;49(1):63–70. doi: 10.1016/j.lungcan.2004.12.006. [DOI] [PubMed] [Google Scholar]
- 3.Nakamura H, Haruki T, Adachi Y, Fujioka S, Miwa K, Taniguchi Y. Smoking affects prognosis after lung cancer surgery. Surg Today. 2008;38(3):227–231. doi: 10.1007/s00595-007-3599-0. [DOI] [PubMed] [Google Scholar]
- 4.Shiono S, Katahira M, Abiko M, Sato T. Smoking is a perioperative risk factor and prognostic factor for lung cancer surgery. Gen Thorac Cardiovasc Surg. 2015;63(2):93–98. doi: 10.1007/s11748-014-0461-3. [DOI] [PubMed] [Google Scholar]
- 5.Shi Y, Weingarten TN, Mantilla CB, Hooten WM, Warner DO. Smoking and pain: pathophysiology and clinical implications. Anesthesiology. 2010;113(4):977–992. doi: 10.1097/ALN.0b013e3181ebdaf9. [DOI] [PubMed] [Google Scholar]
- 6.Bendixen M, Jorgensen OD, Kronborg C, Andersen C, Licht PB. Postoperative pain and quality of life after lobectomy via video-assisted thoracoscopic surgery or anterolateral thoracotomy for early stage lung cancer: a randomised controlled trial. Lancet Oncol. 2016;17(6):836–844. doi: 10.1016/S1470-2045(16)00173-X. [DOI] [PubMed] [Google Scholar]
- 7.Leboeuf-Yde C. Smoking and low back pain. A systematic literature review of 41 journal articles reporting 47 epidemiologic studies. Spine (Phila Pa 1976) 1999;24(14):1463–1470. doi: 10.1097/00007632-199907150-00012. [DOI] [PubMed] [Google Scholar]
- 8.Nesbitt PD. Smoking, physiological arousal, and emotional response. J Pers Soc Psychol. 1973;25(1):137–144. doi: 10.1037/h0034256. [DOI] [PubMed] [Google Scholar]
- 9.Silverstein B. Cigarette smoking, nicotine addiction, and relaxation. J Pers Soc Psychol. 1982;42(5):946–950. doi: 10.1037//0022-3514.42.5.946. [DOI] [PubMed] [Google Scholar]
- 10.Anderson KL, Pinkerton KE, Uyeminami D, Simons CT, Carstens MI, Carstens E. Antinociception induced by chronic exposure of rats to cigarette smoke. Neurosci Lett. 2004;366(1):86–91. doi: 10.1016/j.neulet.2004.05.020. [DOI] [PubMed] [Google Scholar]
- 11.Carstens E, Anderson KA, Simons CT, Carstens MI, Jinks SL. Analgesia induced by chronic nicotine infusion in rats: differences by gender and pain test. Psychopharmacology (Berl) 2001;157(1):40–45. doi: 10.1007/s002130100770. [DOI] [PubMed] [Google Scholar]
- 12.Brett K, Parker R, Wittenauer S, Hayashida K, Young T, Vincler M. Impact of chronic nicotine on sciatic nerve injury in the rat. J Neuroimmunol. 2007;186(1–2):37–44. doi: 10.1016/j.jneuroim.2007.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Josiah DT, Vincler MA. Impact of chronic nicotine on the development and maintenance of neuropathic hypersensitivity in the rat. Psychopharmacology (Berl) 2006;188(2):152–161. doi: 10.1007/s00213-006-0481-5. [DOI] [PubMed] [Google Scholar]
- 14.Green BN, Johnson CD, Snodgrass J, Smith M, Dunn AS. Association between smoking and back pain in a cross-section of adult Americans. Cureus. 2016;8(9):e806. doi: 10.7759/cureus.806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Katyayan PA, Katyayan MK. Effect of smoking status and nicotine dependence on pain intensity and outcome of treatment in Indian patients with temporomandibular disorders: a longitudinal cohort study. J Indian Prosthodont Soc. 2017;17(2):156–166. doi: 10.4103/jips.jips_277_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Montbriand JJ, Weinrib AZ, Azam MA, et al. Smoking, pain intensity, and opioid consumption one to three months after major surgery: a retrospective study in a hospital-based transitional pain service. Nicotine Tob Res. 2017 May 3; doi: 10.1093/ntr/ntx094. Epub. [DOI] [PubMed] [Google Scholar]
- 17.Kim K, Kim HK, Park JS, et al. Video-assisted thoracic surgery lobectomy: single institutional experience with 704 cases. Ann Thorac Surg. 2010;89(6):S2118–S2122. doi: 10.1016/j.athoracsur.2010.03.017. [DOI] [PubMed] [Google Scholar]
- 18.Derby SA. Opioid conversion guidelines for managing adult cancer pain. Am J Nurs. 1999;99(10):62–65. [PubMed] [Google Scholar]
- 19.Plesner K, Jensen HI, Hojsted J. Smoking history, nicotine dependence and opioid use in patients with chronic non-malignant pain. Acta Anaesthesiol Scand. 2016;60(7):988–994. doi: 10.1111/aas.12741. [DOI] [PubMed] [Google Scholar]
- 20.Volkman JE, DeRycke EC, Driscoll MA, et al. Smoking status and pain intensity among OEF/OIF/OND veterans. Pain Med. 2015;16(9):1690–1696. doi: 10.1111/pme.12753. [DOI] [PubMed] [Google Scholar]
- 21.Warner DO, Patten CA, Ames SC, Offord KP, Schroeder DR. Effect of nicotine replacement therapy on stress and smoking behavior in surgical patients. Anesthesiology. 2005;102(6):1138–1146. doi: 10.1097/00000542-200506000-00013. [DOI] [PubMed] [Google Scholar]
- 22.Behrend C, Prasarn M, Coyne E, Horodyski M, Wright J, Rechtine GR. Smoking cessation related to improved patient-reported pain scores following spinal care. J Bone Joint Surg Am. 2012;94(23):2161–2166. doi: 10.2106/JBJS.K.01598. [DOI] [PubMed] [Google Scholar]
- 23.Behrend C, Schonbach E, Coombs A, Coyne E, Prasarn M, Rechtine G. Smoking cessation related to improved patient-reported pain scores following spinal care in geriatric patients. Geriatr Orthop Surg Rehabil. 2014;5(4):191–194. doi: 10.1177/2151458514550479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.O’Bryant CL, Linnebur SA, Yamashita TE, Kutner JS. Inconsistencies in opioid equianalgesic ratios: clinical and research implications. J Pain Palliat Care Pharmacother. 2008;22(4):282–290. doi: 10.1080/15360280802537241. [DOI] [PubMed] [Google Scholar]
- 25.Patanwala AE, Duby J, Waters D, Erstad BL. Opioid conversions in acute care. Ann Pharmacother. 2007;41(2):255–266. doi: 10.1345/aph.1H421. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1.
Equianalgesic opioid conversion table
| Opioid | Administration route | Dose equivalent to 10 mg of oral morphine (mg) |
|---|---|---|
| Morphine | Oral | 10 |
| Morphine | Intravenous | 3.3 |
| Hydromorphone | Oral | 2 |
| Fentanyl | Intravenous | 0.03 |
| Oxycodone | Oral | 7 |
| Codeine | Oral | 80 |
| Tramadol | Oral | 40 |
Data Availability Statement
The datasets generated and analyzed during the current study are available from the corresponding author on reasonable request.