Abstract
Background
This study assessed the perceptions of older adults regarding the plan of care (POC) contained in the clinical summary mandated by the Electronic Health Records (EHR) Incentive Program.
Methods
A qualitative descriptive design was selected for this study. Older adults (≥65) with chronic cardiac diagnoses were invited to participate. The investigator shadowed the physician during the patient encounter, interviewed the patients following their encounter, and asked patients to complete standard health literacy and cognitive screening tools and the Patient Activation Measure. Directed content analysis was used to analyze transcripts.
Results
Patients (n=40) found the clinical summary useful for sharing information with family members and other physicians, reminding and informing, and for engaging in behavior change. Seventy-six percent reported that they would not go online to access the clinical summary for multiple reasons, including not being “computer savvy” and privacy concerns. Participant recommendations for a re-designed, improved clinical summary are included. The clinical summary helps patients and families communicate among health care professionals in a complex, disjointed health care system that often burdens patients with that responsibility. The majority of participants were happy with the paper version and offered multiple reasons for not wanting online access that may help us to focus on more compelling reasons for patient portal use.
Conclusions
Qualitatively, it appears that the clinical summary is a useful tool for engaging people with chronic disease in self-management. The participants in this study told us what many of us already know to be true; that the documentation we provide patients and families is less than ideal.
Keywords: Meaningful use, after-visit summary, patient participation
Introduction
The Electronic Health Records (EHR) Incentive Program, commonly known as “Meaningful Use” was born of the Health Information Technology for Economic and Clinical Health (HITECH) Act (1) embedded in the American Recovery and Reinvestment Act (ARAA) of 2009 (2). It is widely regarded as being successful in its mission to encourage the adoption and meaningful use of EHR by American health care providers. Over the last decade, there has been a rapid increase in the use of EHRs in clinical practice from a low of 9% in 2008 to a high of 84% in 2015 (3). The EHR Incentive Program was designed to be implemented in three stages, each with objectives and measures that became more demanding over time. For example, in stage 1, computerized physician order entry (CPOE) was required for more than 30% of patients and by stage 2 the percentage rose to 60%. In stage 1, providing access to patient records through a patient portal was optional, in stage 2 it was required for 50% of patients, and by stage 3 it was required for 80% of patients (4).
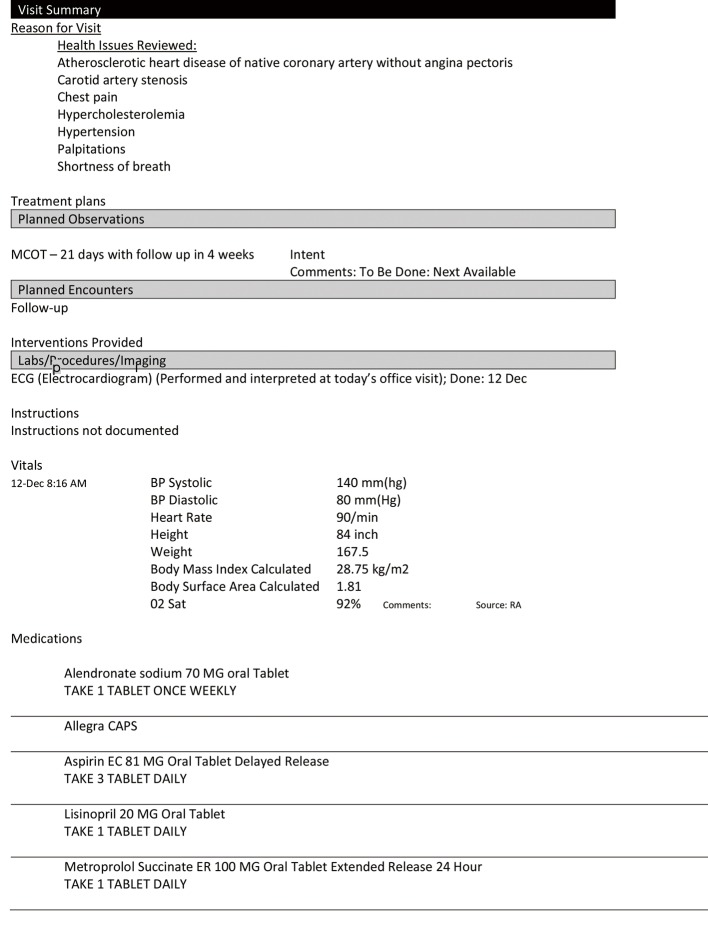
Among other things, Meaningful Use mandated the distribution of a clinical summary to patients at the conclusion of an encounter with their physician. The clinical summary, whether it was provided on paper (stage 1) or through a patient portal (stage 2 and beyond) contains the plan of care (POC) and may include medication, diet or exercise regimens, as well as instructions about monitoring, testing, and follow up visits. The EHR Incentive Program clearly outlines the elements that are required to be present in the clinical summary (Figure 1). All EHR products in use by physician offices and hospitals must be certified to meet Meaningful Use standards, and therefore must be able to reliably produce a summary that contains the required elements. However, different EHR vendors give practices the ability to modify or configure the clinical summary to their own liking, which creates some variation.
Figure 1.
Elements contained in the Meaningful Use clinical summary (5).
As many as 80% of the 38 million adults over the age of 65 in the United States manage at least one chronic disease (6,7). For these older adults, the POC they receive from the physician office serves as a checklist, providing a foundation for chronic disease self-management and engagement in health-promoting behaviors. The Agency for Healthcare Research and Quality (AHRQ) has been a leader in identifying the elements required in a shared POC, which include: patient education about conditions, treatments and self-management, medical treatments and medication lists, the role of other team members (such as psychotherapy or substance abuse therapy), counseling or coaching, and evidence that the plan has been tailored to meet patient/family preferences (8).
Although patient engagement has been written into national quality improvement strategies, there has been little research to date on the ways in which older adults are capable or willing to engage with a healthcare system that is rapidly modernizing with health information technology, and more specifically with a POC that is expected to guide their care across providers and settings.
The purpose of this paper is to report the findings from a qualitative study aimed at assessing the perceptions of older adults regarding the POC contained in the Meaningful Use clinical summary and their willingness to access it online.
Methods
Study design
A qualitative descriptive design (9-11) was utilized to describe the engagement behaviors of older adults with cardiovascular disease (CVD). Forty English-speaking older adults (≥65 years of age) with at least two chronic cardiovascular diagnosis who received care in an outpatient clinic participating in the EHR Incentive Program participated in this study. Older adults with a dementia-related diagnosis on their EHR problem list were excluded from this study. The study took place at two cardiac clinics in urban centers in the American Southwest.
Recruitment
Participants were recruited using purposive sampling in which heterogeneity in literacy, activation, chronic diagnoses, and HIT use could be explored in order to assess variations and identify patterns (12). During their regular clinic appointments, cardiologists asked patients that met inclusion criteria if they were willing to participate in a brief project to discuss patient and physician communication. We recruited from each site on subsequent clinic days until 20 patients were recruited from each site. Three eligible patients were omitted from participation in the study; one whose accompanying daughter was in a hurry to return to work, and two who were sent via ambulance to the hospital from the office.
Procedures
This study was reviewed and approved by the Arizona State University’s Institutional Review Board. The investigator obtained informed consent from patients and family members after describing the planned observation of their routine clinical encounter, an interview lasting no more than 20 minutes, and the completion of a demographic form and standardized instruments at the conclusion of the encounter. Family members were included in the observation and interview when they accompanied the patient to the physician’s office and participated in the clinical encounter. Data were collected with the following devices: an investigator-designed worksheet during the observation, an investigator-designed demographic form, standardized, reliable and valid instruments for measuring health literacy (13,14), patient activation (15,16), and cognition (17-20) in the population of older adults, and investigator-designed interview questions. Table 1 defines and summarizes the psychometric properties of the instruments used in this research.
Table 1. Psychometric properties of data collection instruments.
| Construct | Instrument | Psychometric properties |
|---|---|---|
| Factors that influence health literacy and/or patient activation | Investigator-created demographic form collecting: age, ethnicity, ace, income, education level, health status by the listing of current diagnoses | Content validity, reviewed by experts and compared to the literature |
| Health literacy | Single Item Health Literacy Screener (SILS) | AUROC of 0.74 (95% CI: 0.69–0.79) based on the S-TOFHLA and 0.84 (95% CI: 0.79–0.89) based on the REALM. Construct validity by comparative testing with the S-TOFHLA and REALM |
| Patient activation | Patient Activation Measure (PAM) | Rasch (real) person scores ranged from 0.69–0.84, Rasch (model) person scores ranged from 0.72–0.8. Construct validity with variables that have been conceptually and empirically linked with the PAM (i.e., general prevention behaviors, disease specific behaviors); comparison of means meet thresholds (F=3.1–74.4, P=0.001) |
| Cognition | Mini-Cog | Alpha coefficient =0.92 (P<0.001). Construct validity (factor analysis and convergent) by comparison with independent physician assessment; Pearson correlation =0.65 (P<0.001) |
Analysis
Data were simultaneously collected and analyzed in keeping with general principles of naturalistic research (10,21-25). In practice, this meant keeping detailed field notes, writing analytic memos, and analyzing transcripts for themes after two or three interviews were conducted, before proceeding with additional interviews. Data analysis techniques (12,21,26) consisted primarily of directed content analysis, a technique commonly used in qualitative research to analyze words or phrases in text documents. It was used to identify common patterns of patient engagement with the POC revealed through observation and interview in this study. A detailed account of the procedures used in data analysis (i.e., partitioning meaning units, assigning codes and themes, analytic memoing, constructing data matrices), to testing conclusions, and strategies for ensuring rigor have been described extensively elsewhere (27-29).
Results
A total of 40 patients participated in this study. The average age of participants was 72, ranging from 65 to 86. Sixteen participants (40%) were female. Nine participants, or 23% of the sample, were Hispanic/Latino (Table 2). Six participants (15%) scored positive for cognitive impairment on the Mini-Cog, approximating the national average (30-32). Fifteen participants (38%) brought a family member with them to the physician’s office. Four of the 6 (67%) participants who screened positive for cognitive impairment brought a caregiver and 2 (33%) did not. Approximately half of the sample scored positive on the health literacy screener, indicating possible difficulty with health-related material. Each participant responded to 13 questions on the Patient Activation Measure (PAM), a measure of patient activation (propensity to engage), as they were read out loud to minimize potential barriers due to vision loss or limited health literacy. Participants at the lowest level of activation (level 1) were more likely to have limited health literacy and participants at the highest level of activation (level 4) were more likely to have adequate health literacy. However, we found no relationship between participant responses or preferences based on health literacy, cognition, or patient activation when explored by multiple methods including correlation, data matrices, and other data visualization techniques (histograms, boxplots, bar charts, etc.). In other words, participants with high activation scores, adequate health literacy and no signs of cognitive impairment were no more likely to find the clinical summary valuable or to go online to access it than low activation, low health literacy, cognitively impaired participants. The qualitative findings are presented according to three primary inquiries: patient preference for the clinical summary, preference for online access, and preference for the content of the clinical summary.
Table 2. Description of sample (n=40).
| Variable | No. | % | Mean [range] |
|---|---|---|---|
| Age (year) | 72.8 [65–86] | ||
| 65–74 | 27 | 68 | |
| 76–86 | 13 | 33 | |
| Female gender | 16 | 40 | |
| Hispanic | 9 | 23 | |
| Black | 2 | 5 | |
| Income | |||
| ≥ enough money | 29 | 73 | |
| Not enough money | 11 | 28 | |
| Education | |||
| ≥ College | 23 | 58 | |
| ≥ High school | 17 | 43 | |
| Medicare only | 7 | 18 | |
| Medicare + supplement | 33 | 83 | |
| Visits to cardiologist, last year | 2 [1–6] | ||
| Visits to PCP, last year | 3 [1–10] | ||
| Positive Mini-Cog screen | 6 | 15 | |
| Positive health literacy screen | 21 | 53 | |
| Caregivers present | 15 | 38 | |
| Caregiver present with + Mini-Cog | 4 | 67 | |
| PAM | |||
| Level 1 | 13 | 33 | |
| Level 2 | 4 | 10 | |
| Level 3 | 12 | 30 | |
| Level 4 | 11 | 28 |
Patient Activation Measure (PAM); PCP, primary care physician.
Preference for the clinical summary
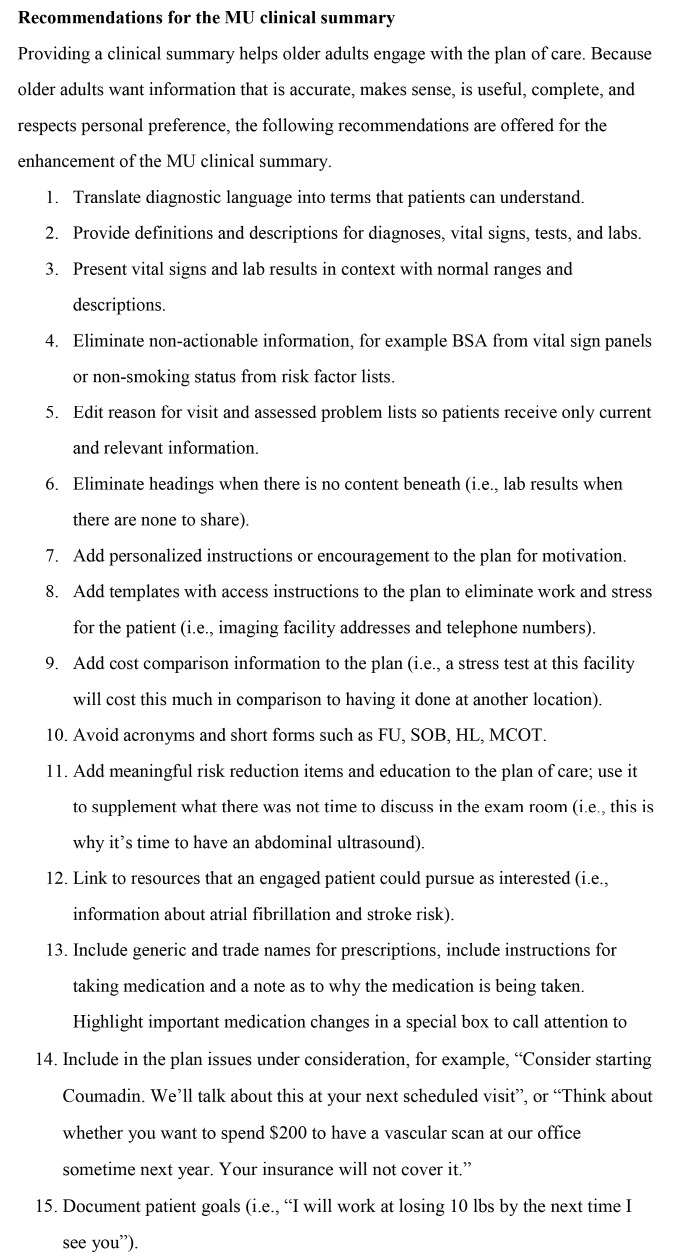
The clinical summaries evaluated from both clinics met the requirements of a Meaningful Use clinical summary, containing the requisite elements (Figure 2). They were shared with participants who were asked to describe aspects of the clinical summary that were helpful and not helpful for managing CVD.
Figure 2.
Example of a Meaningful Use clinical summary.
Participants in the study were generally happy with the clinical summary because it helped them to engage with the POC. The clinical summary helped participants to communicate with other healthcare professionals, “This will be helpful. I can take it to other doctors,” as well as their own families—
Just having this, I mean, is this going to be mine? Just having this paper, at least I can pull it up and say look, you don’t believe what I’m saying, here it is, you know? You read it; maybe I’m reading it wrong.
Participants reported enhanced perceptions of control over their health when having the information from the clinical summary in hand, stating “the whole thing is helpful”.
And these down here, my vitals, that’s very important because I need to be able to know what they are and they are written down and I can always go back to them if I’m taking my blood pressure like tonight, tonight when I come in tonight from work I’m going to take my blood pressure and I probably will be under the same amount of stress tonight as I am now, maybe a little bit more tonight because right now I’m pretty calm, so I’ll be able to compare that.
The clinical summary reportedly helped remind and inform, which was particularly important to those who were “getting forgetful”. This was especially valuable with regard to medications,
That medication list would be good and very helpful because, you know, I can, you know, I can read it now and like aspirin, I know what aspirin is, but the other one, I can try to memorize it but a half an hour later I’ll forget what the name is. I have to—I have to have it marked so I can keep looking at it. My memory is not—it’s just—it only wants to be where I’m interested.
Finally, we suspect the clinical summary may help participants engage with difficult behavior change.
This is very, very good and I’m trying to remember fully—I’m trying to remember everything that was said because there’s so many valid points that what I’ll do is I’ll put this on my refrigerator and start taking a look at it and seeing if I could start the behavioral modification to reach the attainable objective and this may be, if I keep it on my refrigerator, this may be of benefit.
Preference for online access to the clinical summary
Patients were asked if they would use a computer to access their medical records online. The overwhelming majority of patients reported that they would not go online to view their clinical summary or other medical records. Their stated reasons can be explained by the following themes. First, older adults struggled with the technology, claiming they were “not computer savvy”. They were confused by multiple passwords and the extra steps required for a HIPAA-secured login. They were also agitated by navigating from one area to another once inside the patient portal. They were frustrated that the clinical summary was static, unlike other online documents that allowed you to hyperlink to other material for additional information. Second, they expressed concerns over privacy, not wanting to have medical information and social security numbers up on the web, or not wanting to be “nagged” with “one more set of you should do this and you should do that”. Third, some did not own a computer nor possess the interest in learning how to use one, stating “I don’t do computer things, I’m a dinosaur”. Finally, many of the non-computer users explained that they could not see any value in going online for their clinical summary, asking “what could possibly be of benefit there”? One participant commented, “My heart problem isn’t significant enough—I go onto other portals if I’m interested enough in the health problem, like my chronic back pain”. Another said, “There is nothing significant enough to make me interested. Maybe in 10 years down the road when I’ve had more heart stuff, but not now”. Other participants saw the act of going online to look at their medical records as an act of betrayal—
I know my health status because I come here once a year and he tells me everything I need to know—I have complete trust in the doctor and don’t need to double check him.
That’s not something I would look at on a regular basis because, quite frankly, I think I know more or less what the status of my health is right now based on previous doctor visits. That’s why I came here today—to find out. Why would I do that?
Three patients indicated a willingness to “give it a try”, stating, “I’m nervous about hackers, but I’d give it a try” because—
It might be helpful, but it depends on what kind of information was there. I already have a copy of my lab results, so I’d want to see some encouragement or a note about making positive changes, that I’m doing the right thing.
In contrast, four patients were very interested in going online to view records for multiple reasons. One participant stated, “we have a right to have our own records”. Another enjoyed having access to results, which avoided an unnecessary call to the clinic. One participant appreciated that using the online portal for entering and retrieving information made the entire visit more efficient, because you didn’t have to re-enter data into a paper questionnaire at the clinic.
Preference for content in the clinical summary
Clinical summaries were placed in the hands of patients during the research interview. Patients were asked to talk through the document, pointing out what was helpful or not helpful. Participants identified multiple issues with the clinical summaries and their concerns can be expressed by the following categories.
I want information that is accurate
When reading through the clinical summary, participants were quick to point out information that was inaccurate, saying “Well, information is knowledge. You can correct it if something is in there incorrectly, which I have been through with my mother, I can’t tell you how many times”. Other examples include, “Reason for Visit” lists that were identical to the complete “Problem” list and contained entries that were no longer relevant. For example, one woman pointed out that she used to have edema, but she didn’t any more, and that “I didn’t come for this”. Under the heading “Smoking Status”, one patient noted an entry for “current smoker” but the patient hadn’t smoked in 40 years. Multiple participants commented on problem lists that were not kept current, and some patients questioned the content of the plan, saying “He never told me this, to follow a low carbohydrate diet. He never told me that. You were there. He didn’t talk to me about this”. Participants carefully examined the medication lists, and one participant commented that it was not complete because no one had asked her about the supplements she took.
I want information that makes sense
Participants expressed frustration with medical jargon in the clinical summary that was not defined. Both “Reason for Visit” and “Assessed Problem” lists contained SNOMED or ICD-coded diagnostic language that was hard for participants to understand. Participants asked for “regular people descriptions” and said that “I don’t understand this and it’s embarrassing to say you don’t. You don’t want to feel stupid”. Participants were confused about the name of tests particularly when acronyms were used in place of a proper description. They were equally frustrated with laboratory results that were presented without context or explanation. One woman commented that she didn’t “know what a serum calcium level was or why I need to be concerned about it”. Similarly, when values were presented without context, participants were irritated, saying “Right here, heart rate, what does that mean? What is the normal rate?” and “What is BMI? BSA? Why should I worry about that?”
I want information that is useful
Infrequently, participants noted that the information contained in the clinical summary was not useful because they had it already, stating they brought this information with them to the clinic visit (for example, a medication list), and there had been no changes. Another stated that she kept track of these things herself on a home computer, so the clinical summary did not add to her knowledge of her illness.
I want information that is complete
Several participants expressed a desire for more information, above what was provided in the clinical summary. Regarding the medication list, participants wanted not only the name of the medication, but to know why they were taking it and what it was doing for them. Regarding the problem list, patients wanted to be able to learn more about a diagnosis and its routine treatment plan. Others were confused by headings that appeared on the clinical summary without content underneath, asking, “Am I supposed to do something about this?” Still others spoke about the clinical summary being “sparse” and not as “animated” as the conversation with the physician, highlighting the voice of the clinical summary; the POC is clearly a medical narrative, not an illness narrative.
I want information that respects my preference
Although the vast majority of participants included in this sample appreciated the clinical summary and used it in many ways to enhance their care experience, one participant viewed the clinical summary as proof that she should find a different healthcare provider. She reportedly asked not to be “told her weight” and yet it displayed on the clinical summary. She also replied, when asked at the front desk, that her language preference was Spanish, and shared that she would have preferred a clinical summary printed in Spanish—
I can understand English very well. The problem is not for me. It’s for other people who is afraid to tell you, do you know what I mean? For the Hispanic people, things important like this needs to be in Spanish. That is my opinion.
Discussion
The purpose of this paper was to describe results from a study that explored the preferences of older adults and their families for the POC contained in the Meaningful Use clinical summary and their interest in accessing the clinical summary online.
From the physician perspective, the POC for a person with CVD involves aggressive management of key disease indicators, extensive application of evidence-based guidelines, and the use of multiple medications. Evaluated with this lens, the clinical summary document is vitally important to the task of self-management.
We learned that patients and families are grateful for the clinical summary provided by the physician office. Participants treated the clinical summary as a gift, saying “this is mine? I can take it with me?” and that “the whole thing is helpful”. This is not surprising given that the care of the aging chronically ill is complex; patients see multiple providers and receive multiple, sometimes conflicting instructions that must be reconciled by lay and professional members of the patient’s care team. It is encouraging that participants in this study told us that they took the clinical summary home to review with family members, post on the fridge, file in notebooks, and refer to often. Indeed, the clinical summary provides a reference, a good starting place, for conversations about the self-management of chronic disease and helps patients and families communicate among health care professionals in a complex, disjointed health care system that often unfortunately burdens patients with that responsibility.
As health care professionals who accept the value of the clinical summary, we must be intentional about the ways in which we distribute it, knowing that the majority of older adults may not logon to a patient portal to retrieve it. A review of the Pew Research Center reports on internet and technology (33) reveals a trend for increasing adoption of internet-enabled devices among younger, educated, more affluent seniors (roughly four in ten seniors are now smartphone owners) but our research indicates that the same seniors are still skeptical of going online for health-related material at their doctor’s office. This revelation comes at a time when more EHR vendors are developing robust patient portals and even apps for accessing clinical information. Given the complexity of password management, it may be easier for older adults to access medical information through apps instead of traditional websites and we encourage innovation in this space.
Part of the hesitancy to access medical information through a website may be explained by the fact that patients did not see the value in engaging in such behavior. Many participants told us that attending routinely scheduled visits with their cardiologist was good enough and provided as much information as they required. They questioned the additive value of going online to retrieve the clinical summary. While we feel that a quick summary of the topics discussed, an updated medication list, and reminders about upcoming tests and appointments is of value, patients seemed to suggest that additional incentive was required to utilize the clinical summary online. Certainly with the power of technology, gaming, and clinical informatics, we have the ability to accomplish this request. We envision a clinical summary that is hyperlinked to patient resources such as recipes and videos for heart healthy cooking techniques, instructional videos with simple exercises, cardiac-related risk calculators, or additional educational material about diagnoses, medications, and tests. Especially given the pressure physicians face in the well documented shortening of the clinical encounter, an enhanced clinical summary could “virtually” extend the length of the office visit and feelings of being cared for by giving patients time, attention, and information that is it not possible while in the exam room.
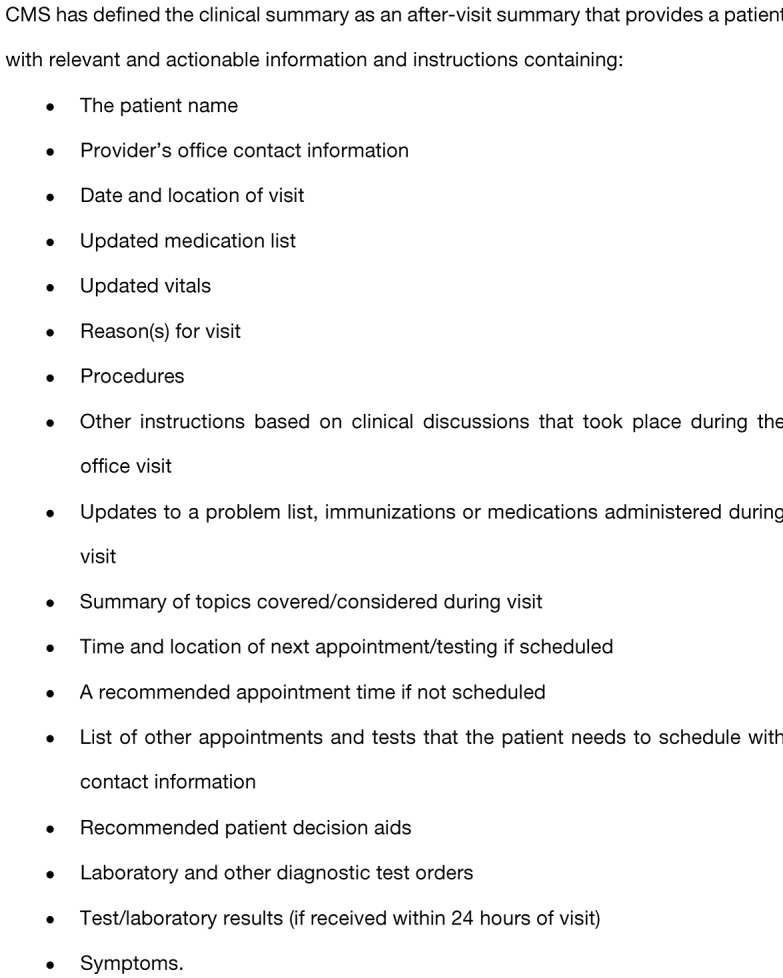
Finally, informaticians and EHR developers ought to be called upon to improve the content of the existing clinical summary, and our participants pointed out many opportunities for improvement. Patients require translations from coded medical diagnoses into language they can understand (i.e., citing history of “heart attack” instead of “myocardial infarction”). They also require a call to action. It is important to differentiate, especially for low literacy readers, what is important and requires action (i.e., “Your blood pressure is too high and we need to work together to bring it down to a normal range”) and what is superfluous (i.e., “Serum calcium: 9.2”). In this age of patient-centered care, technology should make it effortless for documenters to respect patient preference and tailor electronic information to patient values, needs, and predilections, including translating the clinical summary into the patient’s language of preference. We have supplied a list of best practices for the re-design of the Meaningful Use clinical summary from our research participants in Figure 3.
Figure 3.
Recommendations for the re-design of the clinical summary. MU, Meaningful Use.
Limitations
We chose a qualitative methodology for this study because little was known about the subject, accepting that readers of medical literature may be unfamiliar with the design. Clinical summaries from two clinics were used in this research, each clinic using a different, commercially available EHR. Therefore, formats of the clinical summaries varied somewhat, although both products (Allscripts Enterprise and GE Centricity) were certified for use in the EHR Incentive Program and should have contained similar elements. In an attempt to be inclusive, we accepted participants with minimal inclusion criteria. We did not record or specify the length of time a participant had been seen in the clinic nor we did we record the reason for visit. Therefore, it is possible that some participants had more familiarity with the clinical summary than others and this familiarity, or learning curve, may have influenced their responses. Similarly, both clinics were in various stages of Meaningful Use, so their patient populations had varying levels of exposure to the clinical summary document (distributed by their cardiologist or other doctors). One can imagine that over time, exposure to the clinical summary document at a variety of medical facilities might influence a patient’s assessment of the usefulness of the document in the management of chronic disease.
Conclusions
The EHR Incentive Program required a clinical summary in an attempt to enhance patient and family engagement. Several participants in this study identified ways in which it did engage them in their healthcare by informing, reminding, and even motivating. We must be mindful that older adults may not be comfortable with accessing the clinical summary online through patient portals. Innovation in technology may enable more older adults to make use of an electronic clinical summary. The participants in this study asked for a better designed clinical summary, one that would enhance understanding of their condition and allow them to make better use of the documented the POC. The ideas presented in this paper should be incorporated into the design of a more meaningful clinical summary document in order to better meet patient and family preferences and incentivize its use.
Acknowledgements
We appreciate the contributions of Drs. Gerri Lamb, Karen Marek, Bronwynne Evans, and Mel Peralta to this project.
Funding: Research assistance for data collection and analysis was supported by training funds from the National Institutes of Health National Institute on Nursing Research (NIH/NINR), award T32 1T32NR012718-01 Transdisciplinary Training in Health Disparities Science (C Keller, PI). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH or the NINR. This research was supported through the Hartford Center of Gerontological Nursing Excellence at Arizona State University College of Nursing & Health Innovation.
Ethical Statement: This study was reviewed and approved by the Arizona State University’s Institutional Review Board (No. STUDY00001433). Informed consent was obtained from patients and family members by the investigator.
Footnotes
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- 1.US Department of Health and Human Services. Health Information Technology for Economic and Clinical Health Act of 2009. HHS.gov [Internet]. [cited 2018 Jan 10]. Available online: https://www.hhs.gov/hipaa/for-professionals/special-topics/hitech-act-enforcement-interim-final-rule/index.html
- 2.US Congress. American Recovery and Reinvestment Act of 2009. Congress.gov [Internet]. [cited 2018 Jan 10]. Available online: https://www.congress.gov/bill/111th-congress/house-bill/1/text
- 3.Henry J, Pylypchuk Y, Searcy T, et al. Adoption of Electronic Health Record Systems among US Non-Federal Acute Care Hospitals: 2008-2015. The Office of National Coordinator for Health Information Technology 2016. [Internet]. [cited 2018 Jan 10]. Available online: https://dashboard.healthit.gov/evaluations/data-briefs/non-federal-acute-care-hospital-ehr-adoption-2008-2015.php
- 4.Centers for Medicare and Medicaid Services. Comparison of Eligible Professional Measures and Objectives. CMS 2016. [Internet]. [cited 2018 Jan 10]. Available online: https://www.cms.gov/Regulations-and-Guidance/Legislation/EHRIncentivePrograms/Basics.html
- 5.Hummel J, Evans P. Providing Clinical Summaries to Patients after Each Office Visit: A Technical Guide. HealthIT.gov 2012. [Internet]. [cited 2018 Jan 10]. Available online: https://www.healthit.gov/sites/default/files/measure-tools/avs-tech-guide.pdf
- 6.Centers for Disease Control and Prevention. The Power of Prevention. CDC 2009. [Internet]. [cited 2018 Jan 10]. Available online: https://www.cdc.gov/chronicdisease/pdf/2009-power-of-prevention.pdf
- 7.Centers for Disease Control and Prevention. The State of Aging and Health in America. CDC 2013. [Internet]. [cited 2018 Jan 10]. Available online: https://www.cdc.gov/aging/pdf/state-aging-health-in-america-2013.pdf
- 8.Agency for Healthcare Research and Quality. Develop a shared care plan. AHRQ 2017. [Internet]. [cited 2018 Jan 10]. Available online: https://www.ahrq.gov/professionals/education/curriculum-tools/shareddecisionmaking/index.html
- 9.Neergaard MA, Olesen F, Andersen RS, et al. Qualitative description—The poor cousin of health research? BMC Med Res Methodol 2009;9:52-6. 10.1186/1471-2288-9-52 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sandelowski M. Qualitative analysis: What it is and how to begin. Res Nurs Health 1995;18:371-5. 10.1002/nur.4770180411 [DOI] [PubMed] [Google Scholar]
- 11.Sandelowski M. Whatever happened to qualitative description? Res Nurs Health 2000;23:334-40. [DOI] [PubMed] [Google Scholar]
- 12.Miles M, Huberman M, Saldana J. Qualitative data analysis. Thousand Oaks: Sage; 2014. [Google Scholar]
- 13.Chew LD, Bradley K, Boyko E. Brief questions to identify patients with inadequate health literacy. Fam Med 2004;36:588-94. [PubMed] [Google Scholar]
- 14.Chew LD, Griffin J, Partin M, et al. Validation of screening questions for limited health literacy in a large VA outpatient population. J Gen Intern Med 2008;23:561-6. 10.1007/s11606-008-0520-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hibbard JH, Stockard J, Mahoney ER, et al. Development of the Patient Activation Measure (PAM): Conceptualizing and measuring activation in patients and consumers. Health Services Research 2004;39:1005-26. 10.1111/j.1475-6773.2004.00269.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hibbard JH, Mahoney ER, Stockard J, et al. Development and testing of a short form of the patient activation measure. Health Serv Res 2005;40:1918-30. 10.1111/j.1475-6773.2005.00438.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Borson S, Frank L, Bayley P, et al. Improving dementia care: The role of screening and detection of cognitive impairment. Alzheimers Dement 2013;9:151-9. 10.1016/j.jalz.2012.08.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Borson S, Scanlan JM, Chen P, et al. The Mini-Cog as a screen for dementia: Validation in a population-based sample. J Am Geriatr Soc 2003;51:1451-4. 10.1046/j.1532-5415.2003.51465.x [DOI] [PubMed] [Google Scholar]
- 19.Borson S, Scanlan J, Brush M, et al. The Mini-Cog: A cognitive ‘vital signs’ measure for dementia screening in multi-lingual elderly. Int J Geriatr Psychiatry 2000;15:1021-7. [DOI] [PubMed] [Google Scholar]
- 20.Borson S, Scanlan J, Watanabe J, et al. Improving identification of cognitive impairment in primary care. Int J Geriatr Psychiatry 2006;21:349-55. 10.1002/gps.1470 [DOI] [PubMed] [Google Scholar]
- 21.Creswell JW. Qualitative inquiry and research design: Choosing among five approaches. 3rd ed. Los Angeles, CA: Sage, 2013. [Google Scholar]
- 22.Denzin NK. Sociological methods: A sourcebook. 5th ed. New Brunswick, NJ: Aldine Transaction, 2006. [Google Scholar]
- 23.Denzin NK, Lincoln YS. The handbook of qualitative research. New York, NY: Sage, 1994. [Google Scholar]
- 24.Glaser BG, Strauss AL. The discovery of grounded theory: Strategies for qualitative research. New Brunswick, USA: Aldine Transaction, 2012. [Google Scholar]
- 25.Lincoln YS, Guba EG. Naturalistic inquiry. New York, NY: Sage, 1985. [Google Scholar]
- 26.Sandelowski M, Leeman J. Writing usable qualitative health research findings. Qual Health Res 2012:22(10), 1404-13. 10.1177/1049732312450368 [DOI] [PubMed] [Google Scholar]
- 27.Colorafi K, Evans, B. Conducting patient-centered research using qualitative descriptive design. Sage Research Methods Cases, 2017. [Google Scholar]
- 28.Colorafi KJ, Evans B. Qualitative Descriptive Methods in Health Science Research. HERD 2016;9:16-25. 10.1177/1937586715614171 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Colorafi KJ. Patient Centered Health Information Technology: Engagement with the Plan of Care Among Older Adults With Multi-Morbidities [PhD Dissertation]. Arizona State University, 2015. [Google Scholar]
- 30.Zulman DM, Sussman J, Chen X, et al. Examining the evidence: A systematic review of the inclusion and analysis of older adults in randomized controlled trials. J Gen Intern Med 2011;26:783-90. 10.1007/s11606-010-1629-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Centers for Disease Control and Prevention. Healthy aging: Helping people to live long and productive lives and enjoy a good quality of life. CDC 2011. [Internet]. [cited 2018 Jan 10]. Available online: http://www.cdc.gov/chronicdisease/resources/publications/AAG/aging.htm
- 32.West LA, Cole S, Goodkind D, He, W. 65+ in the United States: Special Studies Current Population Reports. United States Census Bureau 2014. [Internet]. [cited 2018 Jan 10]. Available online: https://www.census.gov/content/dam/Census/library/publications/2014/demo/p23-212.pdf
- 33.Anderson M, Perrin A. Tech Adoption Climbs Among Older Adults. Pew Research Center 2017. [Internet]. [cited 2018 Jan 10]. Available online: http://www.pewinternet.org/2017/05/17/tech-adoption-climbs-among-older-adults/