Abstract
Objectives
Air pollution has been associated with increased mortality and morbidity in several studies with indications that its effect could be more severe in children. This study examined the relationship between short-term variations in criteria air pollutants and occurrence of sudden infant death syndrome (SIDS).
Design
We used a case-crossover study design which is widely applied in air pollution studies and particularly useful for estimating the risk of a rare acute outcome associated with short-term exposure.
Setting
The study used data from the West Midlands region in the UK.
Participants
We obtained daily time series data on SIDS mortality (ICD-9: 798.0 or ICD-10: R95) for the period 1996–2006 with a total of 211 SIDS events.
Primary outcome measures
Daily counts of SIDS events.
Results
For an IQR increase in previous day pollutant concentration, the percentage increases (95% CI) in SIDS were 16 (6 to 27) for PM10, 1 (−7 to 10) for SO2, 5 (−4 to 14) for CO, −17 (−27 to –6) for O3, 16 (2 to 31) for NO2 and 2 (−3 to 8) for NO after controlling for average temperature and national holidays. PM10 and NO2 showed relatively consistent association which persisted across different lag structures and after adjusting for copollutants.
Conclusions
The results indicated ambient air pollutants, particularly PM10 and NO2, may show an association with increased SIDS mortality. Thus, future studies are recommended to understand possible mechanistic explanations on the role of air pollution on SIDS incidence and the ways in which we might reduce pollution exposure among infants.
Keywords: epidemiology, community child health, cot death, paediatric thoracic medicine, public health
Strengths and limitations of this study.
Sudden infant death is the leading cause of death in healthy infants between 1 month and 1 year old, and our study is the first based on time series data from the UK to investigate the relationship between common air pollutants and sudden infant death syndrome (SIDS).
Using case-crossover methdology meant we were able to investigate various lags and multi-pollutant models and determine the persistent effects of single pollutants.
Though our study is limited in power due to the comparatively small number of daily SIDS events, our chosen design is widely applied in air pollution studies and particularly useful for estimating the risk of a rare acute outcome associated with short-term exposure.
Introduction
The quality of ambient air is an important factor in the health of adults and children. Ambient air quality is the second largest challenge facing public health in the UK.1 According to WHO, over 3.7 million premature deaths per annum may be attributed to the harmful effects of ambient air. Children, it would seem, are more vulnerable than any other group,2 and recent studies have indicated how even low levels of traffic-related air pollution can have a negative impact on birth outcomes and perinatal health.3 4 A number of studies have also suggested a link between ambient air quality and the incidence of sudden infant death syndrome (SIDS).5–12 Here, we examine the effects of the short-term variations in air pollution and the onset of SIDS.
Sudden infant death is the leading cause of death in healthy infants between 1 month and 1 year old,13 and the impact on the families is notably traumatic as the death is without warning or witness.14 The exact cause continues to tax researchers15 though is likely the result of a combination of factors including susceptibility and environmental stressors such as lower social status of parents,16 environmental tobacco smoke,16 17 the prone position18 and the winter season.5 18 The impact of tobacco smoke suggests a respiratory trigger may be involved, however, the evidence of an association between SIDS and air pollution warrant further research as findings from epidemiological studies have been inconsistent19 20 and few have satisfactorily explored the impact of short-term exposure on SIDS. Our study is the first based on time series data from the UK to investigate the relationship between common air pollutants and SIDS. We have collated data from a 10-year period on concentrations of air pollution and onset of SIDS within the West Midlands one of the largest and most polluted conurbations in the UK and have conducted a case-crossover study to determine any associations.
Methods
Settings
The West Midlands is a metropolitan county in the centre of the UK. It has a population of some 2.8 million.21 The West Midlands is one of the most heavily urbanised counties in the UK and forms the most populated conurbation in the UK outside London, it is at the heart of the UK motorway network and remains a significant centre of the UK’s manufacturing industry.
Data collection
We combined data on SIDS events with data on total births, air pollution, air temperature and a measure of deprivation.
Data on SIDS mortality and total births
We obtained daily time series data on SIDS mortality (International Classification of Diseases(ICD)-9: 798.0 or ICD-10: R95) for the period 1996–2006 from the Perinatal Institute. All cases were between 0 and 12 months old at onset. This data consisted of the date of death and the first three digits of the postal code to avoid the possibility of identifying individual cases due to the rare nature of SIDS. This allowed us to explore the effects of short-term exposure. We obtained daily births data with West Midlands’ postal codes from the Office of National Statistics for the period 1996–2006 and was used for descriptive analysis only.
Air pollution data
The daily time series data on air pollution were compiled from the UK air quality archive managed by Department for the Environment, Food and Rural Affairs. These include a total of 10 monitoring stations in the West Midlands measuring PM10, SO2, NO2, NO, NOx, CO and O3 including sites within Birmingham, Coventry, Walsall and Wolverhampton. Before 1996, the reliability of air quality data was inconsistent. Not all monitoring stations had measurements for the range of pollutants over the entire study period and the precise pollutants measured at each monitoring centre are described in table 1.
Table 1.
Pollutants measured and corresponding time period by monitoring stations
| Name (postal code area) | Pollutants | Time period* |
| Birmingham Centre (B) | PM10, SO2, NO2, NO, NOx, CO, O3 | 01/01/1996 to 31/12/2006 |
| Birmingham East (B) | PM10, SO2, NO2, NO, CO, O3 | 01/01/1996 to 03/08/2004 |
| Birmingham Tyburn (B) | PM10, SO2, NO2, NO, CO, O3 | 16/08/2004 to 31/12/2006 |
| Oldbury (B) | PM10, SO2, NO2, NO, NOx, CO, O3 | 27/06/1997 to 20/09/1998 |
| West Bromwich (B) | PM10, SO2, NO2, NO, NOx, CO, O3 | 04/11/1998 to 31/12/2006 |
| Coventry Centre (CV) | PM10, SO2, NO2, NO, NOx, CO, O3 | 19/02/1997 to 31/12/2006 |
| Coventry Memorial (CV) | PM10, SO2, NO2, NO, NOx, CO, O3 | 26/02/2001 to 31/12/2006 |
| Walsall Alumwell (WS) | NO2, NOx | 01/01/1996 to 31/12/2006 |
| Walsall Willenhall (WS) | NO2 | 13/05/1997 to 31/12/2006 |
| Wolverhampton Centre (WV) | PM10, SO2, NO2, NO, NOx, CO, O3 | 19/12/1995 to 31/12/2006 |
*Period with at least one pollutant being measured and taking into account missing data between start and end dates.
We aimed to examine the association between day-to-day variability in air pollution exposure and SIDS counts over the entire region rather than contrasting exposure and outcome between areas within the West Midlands region. Therefore, the daily pollution data for West Midlands were calculated by averaging across all monitoring stations with available measurements as our models were based on the temporal relationship between air pollution and SIDS; we did not fit a spatial model.
Temperature data
Data on daily minimum and maximum temperature were compiled for weather monitoring stations in the West Midlands from the Meteorological Office British Atmospheric Data Centre.22 We used the average daily temperature which was calculated by taking the average of the minimum and maximum temperature at each monitoring station for each day to obtain the daily average temperature for the entire West Midlands.
Index of Multiple Deprivation score
The Index of Multiple Deprivation (IMD) score is a composite measure based on seven dimensions of deprivation, including income deprivation, employment deprivation, health deprivation and disability, education deprivation, crime deprivation, barriers to housing and services deprivation and living environment deprivation. The data for the 2010 IMD at postal code level were downloaded from EDINA Digimap ShareGeo facility, an online spatial data repository and was used for descriptive analysis only.23
Statistical analysis
The case-crossover design was used to investigate the association between short-term exposure to air pollution and the occurrence of SIDS events controlling for average daily temperature and national holidays. This design, introduced by Maclure,20 has been widely applied in air pollution studies and is particularly useful for estimating the risk of a rare acute outcome associated with short-term exposure.24–27 In case-crossover design, each case acts as their own control and like case–control studies,28 the distribution of exposure is compared between ‘cases’ and ‘controls’. That is, exposure at the time just prior to the event (‘case’ or ‘index’ time) is compared with a set of ‘control’ times that represent the expected distribution of exposure for non-event follow-up times. The design helps primarily to control for confounding by subject-specific factors which remain static over time such as ethnicity and gender.
We applied the time stratified case-crossover approach which has previously been used to minimise bias.29 That is, control days were selected from the same day of the week, within the same calendar month and year as the event day. We applied a conditional Poisson regression model which has been shown to give equivalent estimates as the conditional logistic model but with the advantage of readily allowing for overdispersion and autocorrelation.30 All our models assume a linear effect for air pollution as reported in previous studies31–33 while temperature effects are likely to be non-linear and were modelled using natural splines with 3 df.34–36
Sensitivity analyses
The primary aim was to investigate the risk of SIDS events in relation to air pollution on the previous day in single-pollutant models. To examine sensitivities to our a priori model specification, additional lag structures were explored including single lags of 0, 1, 2,…, 6 days and also the corresponding average of lags 0–1, 0–2, 0–3,…, 0–6. Moreover, the association between SIDS and air pollution was examined after adjusting for the effect of each of the pollutants PM10, SO2, NO2, NO, CO and O3 as a second pollutant in turn. The aim of this two-pollutant modelling approach was to account for potential confounding effect of copollutants. Further sensitivity analyses were performed by controlling for minimum temperature instead of the average temperature. We excluded NOx from the sensitivity analyses as it showed very strong correlation particularly with NO (r=0.96).
Results are presented as percentage increases in mortality with 95% CIs for an IQR increase in pollutant concentration. Hypothesis tests were two sided with a significance level of 0.05. All analyses were performed using the R statistical software; details of the packages used and sample line of code for fitting specific conditional Poisson regression model is given in the supplementary material (see online supplementary file S1).37
bmjopen-2017-018341supp001.pdf (10KB, pdf)
Results
Descriptive statistics
Over the study period (1996–2006), there were 211 SIDS events across the four postal code areas (B, CV, WS and WV) included in the analyses which accounted for about approximately 5% of the days within the study period (table 2). In the same period and location, a total of 943 937 live (single) births were registered.
Table 2.
Average air pollution (µg/m3), temperature (°C) and IMD scores for selected West Midlands postal code areas with SIDS and birth counts, 1996–2006
| Post town (area) | PM10 | SO2 | CO | O3 | NO2 | NO | NOx | Temperature (minimum- maximum) |
IMD score | SIDS event (%) | Birth count (%) |
| Birmingham (B) | 23.8 | 6.8 | 0.4 | 38.5 | 33.9 | 17.5 | 60 | 7.2–12.8 | 36.6 | 118 (55.9) |
753 844 (79.9) |
| Coventry (CV) | 18.3 | 11.3 | 0.3 | 32.4 | 22.5 | 9.2 | 36.2 | 7.7–13.5 | 23.7 | 43 (20.4) |
91 393 (9.7) |
| Walsall (WS) | 41.5 | 89.4 | 6.4–14.0 | 25.2 | 24 (11.4) |
53 532 (5.7) |
|||||
| Wolverhampton (WV) |
23.8 | 9.3 | 0.5 | 38.9 | 29.5 | 18.9 | 59.5 | 8.4–12.3 | 33.4 | 26 (12.3) |
45 168 (4.8) |
| Total | 211 (100) |
943 937 (100) |
IMD, Index of Multiple Deprivation; SIDS, sudden infant death syndrome.
The daily average air pollution concentrations and their SDs are presented in table 3 and show that average concentrations tended to be below UK air quality limits as defined by the EU Ambient Air Quality Directive.38
Table 3.
Descriptive statistics for daily SIDS mortality counts, air pollution (µg/m3), temperature (°C) and birth counts for West Midlands, 1996–2006
| Variable | Mean | SD | Median | IQR | Minimum | Maximum |
| SIDS count | <1 | <1 | 0 | 0–0 | 0 | 2 |
| Average temperature | 10.2 | 5.4 | 10.2 | 6.2–14.5 | −4.2 | 25.0 |
| Maximum temperature | 13.1 | 6.0 | 12.9 | 8.5–17.6 | −2.1 | 29.6 |
| Minimum temperature | 7.4 | 5.1 | 7.5 | 3.6–11.4 | −7.5 | 20.7 |
| PM10 | 23.4 | 11.6 | 20.2 | 15.7–28.2 | 4.0 | 128.9 |
| SO2 | 8.5 | 6.9 | 7.2 | 4.4–10.2 | 0.0 | 70.8 |
| CO | 0.4 | 0.2 | 0.4 | 0.3–0.5 | 0.1 | 3.5 |
| O3 | 38.1 | 18.2 | 38.0 | 25.4–50.4 | 1.3 | 115.8 |
| NO2 | 33.2 | 14.3 | 31.2 | 22.3–41.8 | 5.9 | 113.0 |
| NO | 16.9 | 23.8 | 9.0 | 5.4–17.9 | 0.4 | 314.9 |
| NOx | 64.5 | 49.3 | 51.1 | 35.2–76.4 | 7.9 | 569.2 |
| Birth count* | 290 | 34 | 296 | 266–314 | 183 | 387 |
| IMD score | 32.3 | 12.6 | 31.7 | 21.3–40.5 | 7.2 | 54.9 |
*Counts are for single births only.
IMD, Index of Multiple Deprivation; SIDS, sudden infant death syndrome.
Table 4 shows that there was generally a strong correlation between the levels of pollutants investigated with the exception of the weaker correlation between O3 and PM10 (r=−0.26) and with SO2 (r=−0.34). What was also notable was the negative correlation between ozone and the other pollutants and how in contrast to the other pollutants its positive correlation with temperature.
Table 4.
Pairwise Pearson correlations coefficients (r) for pollutants and temperature
| PM10 | SO2 | CO | O3 | NO2 | NO | NOx | |
| SO2 | 0.53 | ||||||
| CO | 0.56 | 0.59 | |||||
| O3 | −0.26 | −0.34 | −0.56 | ||||
| NO2 | 0.66 | 0.56 | 0.76 | −0.62 | |||
| NO | 0.54 | 0.48 | 0.87 | −0.58 | 0.73 | ||
| NOx | 0.59 | 0.56 | 0.90 | −0.62 | 0.86 | 0.96 | |
| Temperature | −0.08 | −0.24 | −0.39 | 0.40 | −0.40 | −0.38 | −0.40 |
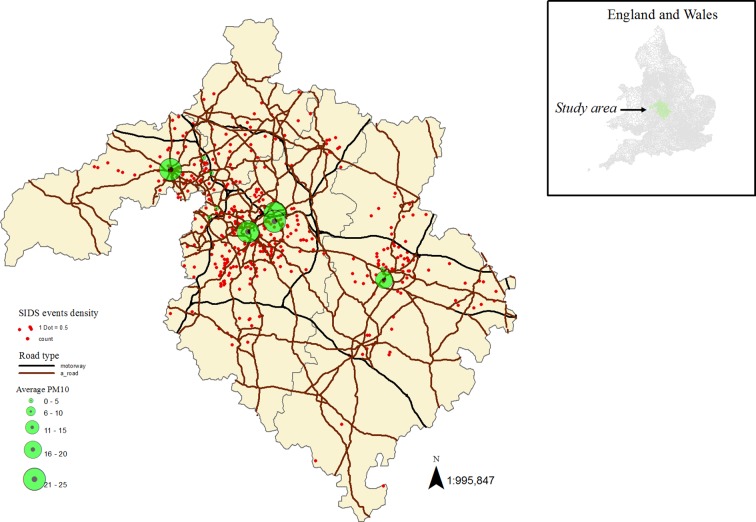
Comparing the four postal code areas, Birmingham had the highest SIDS mortality (about 56%) and births rates (about 80%). Air pollution concentrations were more or less similar for Birmingham and Wolverhampton except slightly lower levels of NO2 and higher levels of SO2 observed for the latter. Coventry had the lowest pollution level with respect to all pollutants except SO2. Walsall had measurements for NO2 and NOx only which were very large compared with the other postal code areas (table 2). Similarly, Birmingham and Wolverhampton had higher average deprivation scores compared with Coventry and Walsall (table 2). Also, SIDS counts and pollution levels tended to be larger in highly deprived areas and near motorways and A-road networks which may be a reflection of population density (figure 1; see online supplementary figure S2). There was also indication of seasonal pattern for SIDS occurrence; the highest proportions of SIDS were observed in January and February (about 10%) and among the relatively colder months and in July (about 14%) among the warmer months (data not shown).
Figure 1.
Air pollution monitoring sites with road networks (motorways and A-roads) and sudden infant death syndrome (SIDS) events in the study area. We used ArcGIS Desktop V.10.2 (http://www.esri.com/software/arcgis) to create the map combining shapefiles for postal code areas and motorways and overlaying air pollution and SIDS data.
bmjopen-2017-018341supp002.jpg (543KB, jpg)
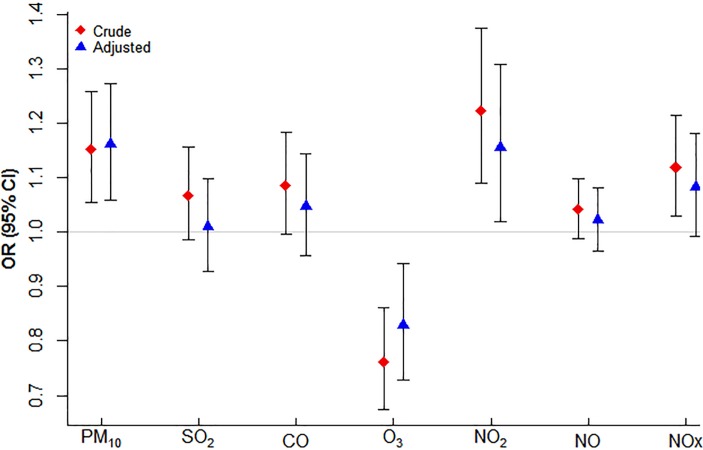
Case-crossover analysis
Figure 2 shows the estimated OR (95% CI) for the association of SIDS events with each of the pollutants considered based on the conditional Poisson model. For an IQR increase in previous day pollutant concentration, the percentage increases (95% CI) for the risk of SIDS death was 16 (6 to 27); p=0.002 for PM10, 1 (−7 to 10); p=0.83 for SO2, 5 (−4 to 14); p=0.33 for CO, −17 (−27 to –6); p=0.004 for O3, 16 (2 to 31); p=0.02 for NO2, 2 (−3 to 8); p=0.47 for NO and 8 (−1 to 18); p=0.07 for NOx after controlling for average temperature and national holidays. Therefore, considering pollutant levels at lag 1, significant association with increased risk of SIDS was indicated only for PM10 and NO2 while a protective effect was apparent for O3.
Figure 2.
Estimated risk of sudden infant death syndrome for an IQR increase in lag 1 pollutant concentration before and after controlling for confounding by average temperature and national holidays.
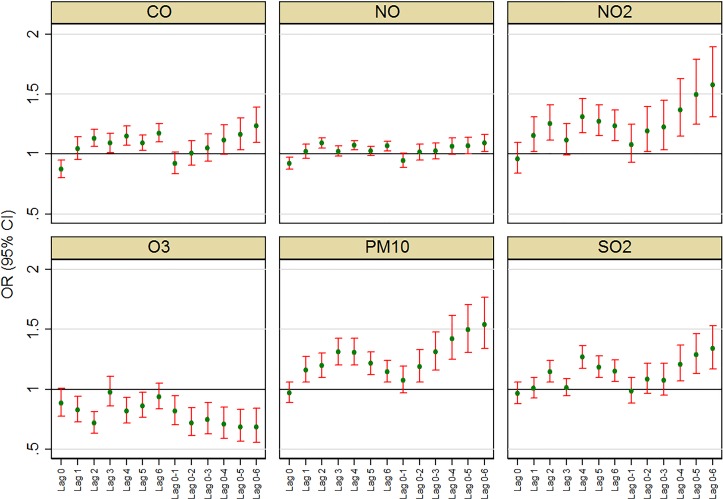
Sensitivity analyses
Lag structures: Analyses exploring relationships between SIDS and air pollution for other lag structures (lags 0, 2, 3,…, 6 and corresponding average of lags 0–1, 0–2, 0–3,…, 0–6) indicated associations were somewhat sensitive to the choice of lag (figure 3). In the single-lag models, there was an impression of stronger delayed effects for CO, NO2, O3, PM10 and SO2 compared with relatively recent lags (lag 0 and lag 1). The effect of NO appeared to remain comparatively flat across lags. Relatively more consistent association across lags was observed for NO2 and PM10 and to some extent for CO. Likewise, in average lag models, ORs tended to increase with averaging over more lags with exception of NO where such an effect was not observed. Results were also similar (at least qualitatively) after adjusting for minimum temperature instead of the average temperature (see online supplementary figure S3).
Figure 3.
Risk of sudden infant death syndrome associated with an IQR increase in pollution for selected lags and average of lags; models adjusted for average temperature and national holidays.
bmjopen-2017-018341supp003.jpg (144.1KB, jpg)
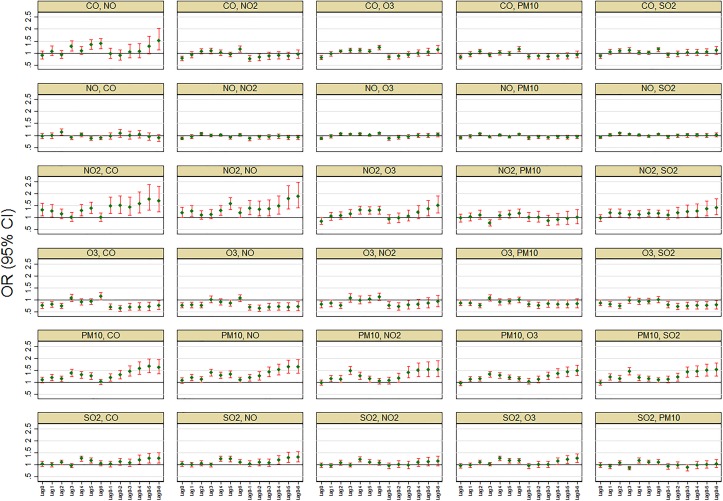
Multipollutant models: Further investigation using two-pollutant models also showed associations were sensitive to control of other pollutants. In general, adjusting for copollutants appeared to attenuate ORs towards the null except for NO2 and PM10 where effects remained to persist (figure 4). Interestingly, after controlling for PM10, the protective effect of O3 and the adverse effect of NO2 observed in the single-pollutant models were not apparent for most of the lag choices. Similarly, none of the other pollutants showed marked association with SIDS after controlling for PM10 effects. The estimates from the multipollutant model should, however, be interpreted with caution as most of the pollutants were correlated.
Figure 4.
Risk of sudden infant death syndrome associated with an IQR increase in air pollution after controlling for copollutants, average temperature and national holidays (panel titles indicate: main and copollutant, respectively).
Comments
Summary of findings
In this study, we hypothesised a delayed effect (lag 1) of air pollution on SIDS incidence and investigated additional lags in sensitivity analyses and in single-pollutant and multipollutant models. Though CIs were wide, we found evidence suggesting association of SIDS mortality with PM10 and NO2 exposure. Compared with other pollutants, their effects persisted after controlling for copollutants and across the various lag structures investigated. The exception was controlling for O3 did attenuate the risk estimates observed for both PM10 and NO2. There were no consistent associations observed with exposure to the remaining pollutants investigated (CO, SO2, NO, NOx). An exception was the protective effect observed in relation to O3 exposure.
Strengths and limitations
Previous studies have tended to focus on relatively longer-term exposure to air pollutants.37 39 40 Our study is one of the first to use case-crossover methodology to explore the impact of air pollution on SIDS based on data from UK. Using an approach that is suitable for estimating the risk of a rare acute outcome such as SIDS events, we were able to investigate various lags and multipollutant models indicating delayed effects of pollutants that persisted after controlling for copollutants. However, measurement error for air pollution exposure a potential limitation in this study as we did not use personal measurements. Other epidemiological studies using data from ambient monitoring stations have shown a good level of correlation between daily personal exposure and daily ambient air pollution measurements,36 37 though there is the potential for measurement error that can attenuate regression coefficient estimates. That is, such misclassification will likely lead to an underestimation of the effects. We were also unable to control for influenza and humidity as we did not have access to reliable data for these variables.
Detailed discussion
Certain groups of the population are more vulnerable to ambient air pollution than others and children figure predominantly among them due to the fragility of their immune system and the ratio of their lung capacity to their size.41 Particulate matter has been recognised as the most significant contributor to air quality-related morbidity and mortality42 and a number of studies have reported a link between infant mortality and PM10 at similar concentrations of pollutant below air quality guidelines as are described in this study.11 43 44 However, previous evidence of a direct association with SIDS is inconclusive and few studies describe a significant association of PM10 with increased risk.6 45
The potential association with NO2 we discovered reflected the findings of a multicity study from Canada that found an increased risk for SIDS with a lag of 2 days.8 More broadly, our findings are in line with previous studies that have found evidence of a lag between exposure to criteria pollutants and mortality. For PM10, a single-day exposure has been shown to have an effect for up to 5 days46 47 and numbers of respiratory deaths appear to be more affected by air pollution levels on previous days, than cardiovascular deaths that are impacted by same-day pollution.48 For example, myocardial infarction represents an acute response to a trigger.49
This is biologically plausible when considering how a wider and more lagged response can be expected for deaths from respiratory responses to pollution (eg, chronic obstructive pulmonary disease) via the proposed mechanisms, such as pulmonary or systemic inflammation and modulated immunity.50
With regard to the apparent protective properties of O3 that we describe here, its worth noting that these have been seen previously.39 One possible reason for the negative association of O3 and SIDS might be its negative correlation with other pollutants, in particular that with fine particulate matter pollution.51 O3 also showed a positive correlation with temperature while all other pollutants were negatively correlated.
Concern around the effects of air pollution continues to mount particularly within developing economies52 where it contributes to 3.3 million premature deaths worldwide per year, a figure estimated to double by 2050 if the issue remains unattended.53 However, it appears that recently fossil fuel emissions have begun to increase again due to the developing world’s reliance on them to power their expanding economies.54 In the developed West, policy initiatives are beginning to recognise the mounting issue posed by the adverse effects on health posed by ambient air pollution. However, shifting political priorities in the USA has seen a commitment to revitalise the coal industry55 and an increase in the production of shale oil.56 However, mitigating these risks is not a straightforward proposition and government policies appear slow to react, for example, in the UK pledges to cease sales of diesel and petrol cars do not come into effect until 2040.57
In the absence of coherent policy to address the issue, a number of proposals have been put forward to mitigate the effects of high levels of ambient exposure. Knowing that children and young adults may be highly susceptible to some of the subclinical changes caused by air pollution58 59 and as indoor concentrations are lower than ambient levels, advice has been to remain indoors to reduce exposure and acute health risks on high air pollution days.60 There are also systems available for cleaning indoor air though these may be deemed expensive for the economically deprived.61 There has also been a case made for chemopreventive interventions, such as antioxidant or antithrombotic agents, but without data on health outcomes, no recommendations can be made in their use for primary prevention.62
Conclusions
Understanding the effects of air pollution on child heath is more relevant than ever. Our work here has highlighted a potential association of sudden infant death with PM10 and NO2 and the association with particulate matter and infant mortality in particular is widely recognised. However, until policy reflects the growing evidence and responds to mounting public concern, it would appear to be the responsibility of individuals to take independent action to mitigate the effects of air pollution and protect the health of their young ones.
Supplementary Material
Footnotes
Contributors: IJL contributed to the conceptualisation of the study, initial drafting of the manuscript and supervised the research project at all stages. NIM contributed to the research design, performed the data management, analysis and interpretation, and with IJL drafted the initial manuscript. JGA contributed to the conceptualisation of the study, data interpretation and critically reviewed the manuscript. JJKJ contributed to the conceptualisation of the study, data interpretation and critically reviewed the manuscript. All authors approved the final manuscript as submitted.
Funding: This work was supported by The Lullaby Trust, grant number 260.
Competing interests: None declared.
Patient consent: Not required.
Ethics approval: Ethical approval was given by the University of Birmingham, Life and Health Sciences Ethical Review Committee.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: No additional data are available.
References
- 1. Royal College of Physicians, Royal College of Paediatrics and Child Health. Every breath we take: The lifelong impact of air pollution. 2016. https://www.rcplondon.ac.uk/projects/outputs/every-breath-we-take-lifelong-impact-air-pollution (accessed Apr 2017).
- 2. World Health Organization. Burden of disease from ambient air pollution for 2012. 2014. http://www.who.int/phe/health_topics/outdoorair/databases/AAP_BoD_results_March2014.pdf?ua=1 (accessed Apr 2017).
- 3. Brauer M, Lencar C, Tamburic L, et al. . A cohort study of traffic-related air pollution impacts on birth outcomes. Environ Health Perspect 2008;116:680–6. 10.1289/ehp.10952 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Fleischer NL, Merialdi M, van Donkelaar A, et al. . Outdoor air pollution, preterm birth, and low birth weight: analysis of the world health organization global survey on maternal and perinatal health. Environ Health Perspect 2014;122:425–30. 10.1289/ehp.1306837 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Knöbel HH, Chen CJ, Liang KY. Sudden infant death syndrome in relation to weather and optimetrically measured air pollution in Taiwan. Pediatrics 1995;96:1106–10. [PubMed] [Google Scholar]
- 6. Lipfert FW, Zhang J, Wyzga RE. Infant mortality and air pollution: a comprehensive analysis of U.S. data for 1990. J Air Waste Manag Assoc 2000;50:1350–66. 10.1080/10473289.2000.10464168 [DOI] [PubMed] [Google Scholar]
- 7. Hunt CE. Sudden infant death syndrome and other causes of infant mortality: diagnosis, mechanisms, and risk for recurrence in siblings. Am J Respir Crit Care Med 2001;164:346–57. 10.1164/ajrccm.164.3.9910045 [DOI] [PubMed] [Google Scholar]
- 8. Dales R, Burnett RT, Smith-Doiron M, et al. . Air pollution and sudden infant death syndrome. Pediatrics 2004;113:e628–31. 10.1542/peds.113.6.e628 [DOI] [PubMed] [Google Scholar]
- 9. Kaiser R, Romieu I, Medina S, et al. . Air pollution attributable postneonatal infant mortality in U.S. metropolitan areas: a risk assessment study. Environ Health 2004;3:4 10.1186/1476-069X-3-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Heinrich J, Slama R. Fine particles, a major threat to children. Int J Hyg Environ Health 2007;210:617–22. 10.1016/j.ijheh.2007.07.012 [DOI] [PubMed] [Google Scholar]
- 11. Yorifuji T, Kashima S, Doi H. Acute exposure to fine and coarse particulate matter and infant mortality in Tokyo, Japan (2002-2013). Sci Total Environ 2016;551-552:66–72. 10.1016/j.scitotenv.2016.01.211 [DOI] [PubMed] [Google Scholar]
- 12. Luechinger S. Air pollution and infant mortality: a natural experiment from power plant desulfurization. J Health Econ 2014;37:219–31. 10.1016/j.jhealeco.2014.06.009 [DOI] [PubMed] [Google Scholar]
- 13. National Institute of Child Health and Human Development. How many infants die from SIDS or are at risk for SIDS? 2013. https://www.nichd.nih.gov/health/topics/sids/conditioninfo/pages/risk.aspx (accessed Apr 2017).
- 14. Kinney HC, Thach BT. The sudden infant death syndrome. N Engl J Med 2009;361:795–805. 10.1056/NEJMra0803836 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Goldwater PN. Infection: the neglected paradigm in SIDS research. Arch Dis Child 2017;102:767–72. 10.1136/archdischild-2016-312327 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Leach CE, Blair PS, Fleming PJ, et al. . Epidemiology of SIDS and explained sudden infant deaths. CESDI SUDI Research Group. Pediatrics 1999;104:e43. [DOI] [PubMed] [Google Scholar]
- 17. Brooke H, Gibson A, Tappin D, et al. . Case-control study of sudden infant death syndrome in Scotland, 1992-5. BMJ 1997;314:1516–20. 10.1136/bmj.314.7093.1516 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Douglas AS, Allan TM, Helms PJ. Seasonality and the sudden infant death syndrome during 1987-9 and 1991-3 in Australia and Britain. BMJ 1996;312:1381–3. 10.1136/bmj.312.7043.1381a [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Glinianaia SV, Rankin J, Bell R, et al. . Does particulate air pollution contribute to infant death? A systematic review. Environ Health Perspect 2004;112:1365–70. 10.1289/ehp.6857 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Tong S, Colditz P. Air pollution and sudden infant death syndrome: a literature review. Paediatr Perinat Epidemiol 2004;18:327–35. 10.1111/j.1365-3016.2004.00565.x [DOI] [PubMed] [Google Scholar]
- 21. Office for National Statistics. UK population estimates", 2014. (Retrieved 27 July 2015). [Google Scholar]
- 22. National Centre for Atmospheric Science, Natural Environment Research Council. British Atmospheric Data Centre. http://badc.nerc.ac.uk/home/index_beacon.html (accessed Apr 2017).
- 23. Pope A. "Indices of Deprivation England and Wales 2010" [ESRI Shapefile geospatial data]. 2013. https://www.sharegeo.ac.uk/handle/10672/481 (accessed Dec 2016).
- 24. Maclure M. The case-crossover design: a method for studying transient effects on the risk of acute events. Am J Epidemiol 1991;133:144–53. 10.1093/oxfordjournals.aje.a115853 [DOI] [PubMed] [Google Scholar]
- 25. Lee JT, Schwartz J. Reanalysis of the effects of air pollution on daily mortality in Seoul, Korea: A case-crossover design. Environ Health Perspect 1999;107:633–6. 10.1289/ehp.99107633 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Jaakkola JJ. Case-crossover design in air pollution epidemiology. Eur Respir J Suppl 2003;40:81S–5. 10.1183/09031936.03.00402703 [DOI] [PubMed] [Google Scholar]
- 27. Pope CA, Muhlestein JB, May HT, et al. . Ischemic heart disease events triggered by short-term exposure to fine particulate air pollution. Circulation 2006;114:2443–8. 10.1161/CIRCULATIONAHA.106.636977 [DOI] [PubMed] [Google Scholar]
- 28. Bhaskaran K, Hajat S, Armstrong B, et al. . The effects of hourly differences in air pollution on the risk of myocardial infarction: case crossover analysis of the MINAP database. BMJ 2011;343:d5531 10.1136/bmj.d5531 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Janes H, Sheppard L, Lumley T. Case-crossover analyses of air pollution exposure data: referent selection strategies and their implications for bias. Epidemiology 2005;16:717–26. [DOI] [PubMed] [Google Scholar]
- 30. Breslow NE, Day NE. Statistical methods in cancer research. Volume I - The analysis of case-control studies. IARC Sci Publ 1980;32:5–338. [PubMed] [Google Scholar]
- 31. Armstrong BG, Gasparrini A, Tobias A. Conditional poisson models: a flexible alternative to conditional logistic case cross-over analysis. BMC Med Res Methodol 2014;14:122 10.1186/1471-2288-14-122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Le Tertre A, Medina S, Samoli E, et al. . Short-term effects of particulate air pollution on cardiovascular diseases in eight European cities. J Epidemiol Community Health 2002;56:773–9. 10.1136/jech.56.10.773 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Katsouyanni K, Samet JM, Anderson HR, et al. . Air pollution and health: a European and North American approach (APHENA). Res Rep Health Eff Inst 2009:5–90. [PubMed] [Google Scholar]
- 34. Scheers H, Mwalili SM, Faes C, et al. . Does air pollution trigger infant mortality in Western Europe? A case-crossover study. Environ Health Perspect 2011;119:1017–22. 10.1289/ehp.1002913 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Braga AL, Zanobetti A, Schwartz J. The effect of weather on respiratory and cardiovascular deaths in 12 U.S. cities. Environ Health Perspect 2002;110:859–63. 10.1289/ehp.02110859 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Armstrong B. Models for the relationship between ambient temperature and daily mortality. Epidemiology 2006;17:624–31. 10.1097/01.ede.0000239732.50999.8f [DOI] [PubMed] [Google Scholar]
- 37. R Core Team. R: A language and environment for statistical computing. 2013. http://www.R-project.org (accessed Apr 2017).
- 38. Department for Environment Food & Rural Affairs. UK and EU air quality limits. https://uk-air.defra.gov.uk/air-pollution/uk-eu-limits (accessed Dec 2017).
- 39. Ritz B, Wilhelm M, Zhao Y. Air pollution and infant death in southern California, 1989-2000. Pediatrics 2006;118:493–502. 10.1542/peds.2006-0027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Woodruff TJ, Darrow LA, Parker JD. Air pollution and postneonatal infant mortality in the United States, 1999-2002. Environ Health Perspect 2008;116:110–5. 10.1289/ehp.10370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Pope CA, Dockery DW. Health effects of fine particulate air pollution: lines that connect. J Air Waste Manag Assoc 2006;56:709–42. 10.1080/10473289.2006.10464485 [DOI] [PubMed] [Google Scholar]
- 42. Landrigan PJ, Fuller R, Acosta NJR, et al. . The lancet commission on pollution and health. Lancet 2018;391:462–512. 10.1016/S0140-6736(17)32345-0 [DOI] [PubMed] [Google Scholar]
- 43. Rice MB, Ljungman PL, Wilker EH, et al. . Short-term exposure to air pollution and lung function in the Framingham Heart Study. Am J Respir Crit Care Med 2013;188:1351–7. 10.1164/rccm.201308-1414OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Samoli E, Stafoggia M, Rodopoulou S, et al. . Associations between fine and coarse particles and mortality in Mediterranean cities: results from the MED-PARTICLES project. Environ Health Perspect 2013;121:932–8. 10.1289/ehp.1206124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Woodruff TJ, Parker JD, Schoendorf KC. Fine particulate matter (PM2.5) air pollution and selected causes of postneonatal infant mortality in California. Environ Health Perspect 2006;114:786–90. 10.1289/ehp.8484 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Schwartz J. The distributed lag between air pollution and daily deaths. Epidemiology 2000;11:320–6. 10.1097/00001648-200005000-00016 [DOI] [PubMed] [Google Scholar]
- 47. Alessandrini ER, Stafoggia M, Faustini A, et al. . Association between short-term exposure to PM 2.5 and PM 10 and mortality in susceptible subgroups: a multisite case-crossover analysis of individual effect modifiers. Am J Epidemiol 2016;184:744–54. 10.1093/aje/kww078 [DOI] [PubMed] [Google Scholar]
- 48. Braga AL, Zanobetti A, Schwartz J. The lag structure between particulate air pollution and respiratory and cardiovascular deaths in 10 US cities. J Occup Environ Med 2001;43:927–33. 10.1097/00043764-200111000-00001 [DOI] [PubMed] [Google Scholar]
- 49. Gold DR, Litonjua A, Schwartz J, et al. . Ambient pollution and heart rate variability. Circulation 2000;101:1267–73. 10.1161/01.CIR.101.11.1267 [DOI] [PubMed] [Google Scholar]
- 50. Blackwell C, Moscovis S, Hall S, et al. . Exploring the risk factors for sudden infant deaths and their role in inflammatory responses to infection. Front Immunol 2015;6:44 10.3389/fimmu.2015.00044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Sarnat JA, Schwartz J, Suh HH. Fine particulate air pollution and mortality in 20 U.S. cities. N Engl J Med 2001;344:1253–4. 10.1056/NEJM200104193441614 [DOI] [PubMed] [Google Scholar]
- 52. WHO. WHO (2014) “Burden of Disease from Ambient Air Pollution for 2012.” n.d. http://www.who.int/phe/health_topics/outd oorair/databases/AAP_BoD_results_March20 14.pdf
- 53. Lelieveld J, Evans JS, Fnais M, et al. . The contribution of outdoor air pollution sources to premature mortality on a global scale. Nature 2015;525:367–71. 10.1038/nature15371 [DOI] [PubMed] [Google Scholar]
- 54. Jackson RB, Le Quéré C, Andrew RM, et al. . Warning signs for stabilizing global CO 2 emissions. Environmental Research Letters 2017;12:110202 10.1088/1748-9326/aa9662 [DOI] [Google Scholar]
- 55. Independent. Donald Trump promises to bring back coal jobs but experts disagree. http://www.independent.co.uk/news/world/americas/donald-trump-coal-mining-jobs-promise-experts-disagree-executive-order-a7656486.html (accessed Nov 2017).
- 56. U.S. Energy Information Administration. How much shale (tight) oil is produced in the United States? https://www.eia.gov/tools/faqs/faq.php?id=847&t=6 (accessed Nov 2017).
- 57. The Guardian. Britain to ban sale of all diesel and petrol cars and vans from 2040. https://www.theguardian.com/politics/2017/jul/25/britain-to-ban-sale-of-all-diesel-and-petrol-cars-and-vans-from-2040 (accessed Nov 2017).
- 58. Rich DQ, Kipen HM, Huang W, et al. . Association between changes in air pollution levels during the Beijing Olympics and biomarkers of inflammation and thrombosis in healthy young adults. JAMA 2012;307:2068–78. 10.1001/jama.2012.3488 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Wright RJ, Brunst KJ. Programming of respiratory health in childhood: influence of outdoor air pollution. Curr Opin Pediatr 2013;25:232–9. 10.1097/MOP.0b013e32835e78cc [DOI] [PubMed] [Google Scholar]
- 60. Plaia A, Ruggieri M. Air quality indices: a review. Rev Environ Sci Bio 2011;10:165–79. 10.1007/s11157-010-9227-2 [DOI] [Google Scholar]
- 61. Macintosh DL, Myatt TA, Ludwig JF, et al. . Whole house particle removal and clean air delivery rates for in-duct and portable ventilation systems. J Air Waste Manag Assoc 2008;58:1474–82. 10.3155/1047-3289.58.11.1474 [DOI] [PubMed] [Google Scholar]
- 62. Laumbach R, Meng Q, Kipen H. What can individuals do to reduce personal health risks from air pollution? J Thorac Dis 2015;7:96–107. 10.3978/j.issn.2072-1439.2014.12.21 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2017-018341supp001.pdf (10KB, pdf)
bmjopen-2017-018341supp002.jpg (543KB, jpg)
bmjopen-2017-018341supp003.jpg (144.1KB, jpg)