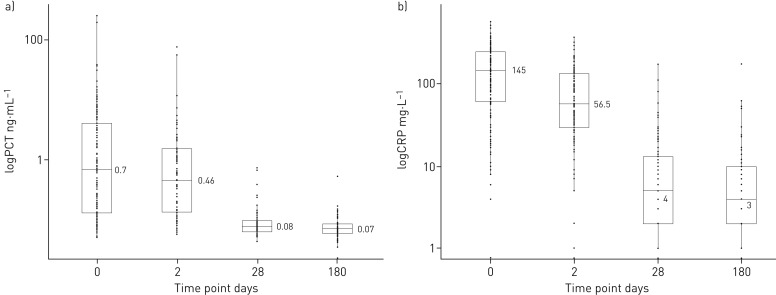
FIGURE 2.
a) Distribution of pro-calcitonin (PCT) levels on admission and during follow-up. At all time points, the distribution of PCT values was wide. Using accepted respiratory tract infection treatment thresholds, on admission 64.5% of values were >25 ng·mL1 and 54.6% of values were >0.5 ng·mL1. 48 h after in-hospital treatment, the median PCT level had fallen when compared with the median on admission, but many subjects had levels in the treatment range. By 1 month, the median PCT level had fallen below the lower treatment threshold of 0.25 ng·mL1; however, at 1 month and 6 months, some subjects had high PCT levels. b) Distribution of C-reactive protein (CRP) levels on admission and during follow-up. The pattern of CRP level was very similar to that of pro-calcitonin. Values were high at presentation, had begun to fall by 48 h, had fallen substantially by 1 month, and had changed very little between 1 month and 6 months. The 2014 NICE pneumonia guidelines suggest that antibiotic treatment should be offered to all patients diagnosed with pneumonia. If a diagnosis of pneumonia cannot be made, but a lower respiratory tract infection has been diagnosed, then the decision to treat with antibiotics can be assisted by the CRP level. If the CRP level is >100 mg·L1, antibiotics are recommended; antibiotics are considered if the level is between 20 and 100 mg·L1; antibiotics are withheld if the level is <20 mg·L1.