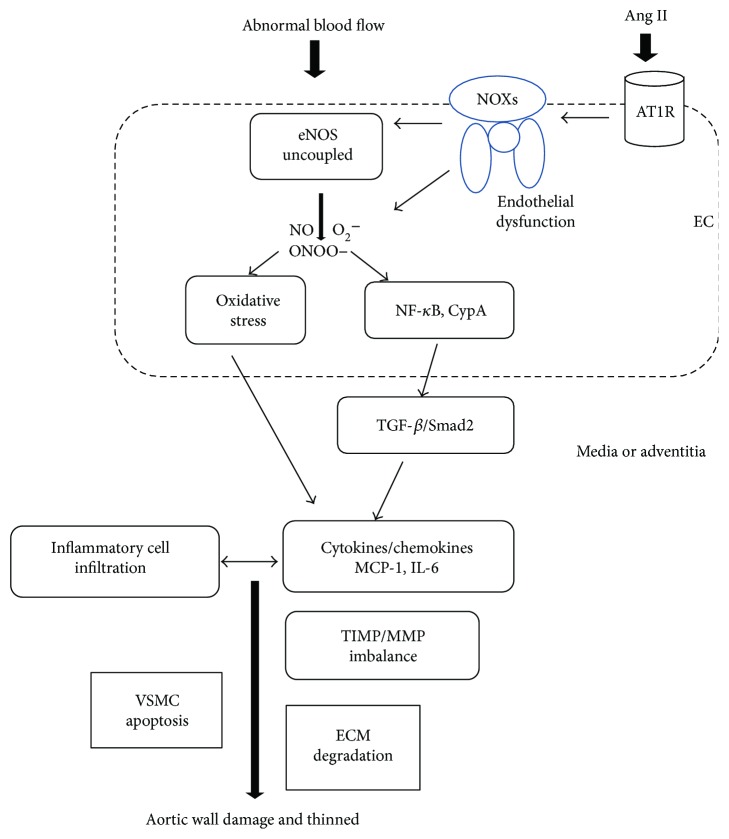
Figure 2.
The proposed role of the endothelium in AAA formation. Shear stress produced by blood flow together with Ang II influences the endothelium to cause endothelial dysfunction via uncoupling of eNOS and oxidative stress induction. Endothelial dysfunction activates NOXs, NF-κB, CypA, and TGF-β/Smad2 pathways to further initiate and amplify the inflammatory reaction via overproduction of cytokines and chemokines such as MCP-1 and IL-6. More inflammatory cells infiltrate and exacerbate oxidative stress to form a vicious cycle. The balance of TIMP/MMP is tipped, and proteolysis is promoted. Eventually, the aortic wall is damaged as a result of SMCs apoptosis and ECM degradation due to proteolytic degradation. EC: endothelial cell; Ang II: angiotensin II; AT1R: AT1 receptor; eNOS: endothelial nitric oxide synthase; NO: nitric oxide; O2−: superoxide anion; ONOO−: nitrous oxide ion; NF-κB: nuclear factor-kappa B; CypA: cyclophilin A; TGF-β: transforming growth factor-β; MCP-1: monocyte chemoattractant protein-1; IL-6: interleukin-6; TIMP: tissue inhibitors of metalloproteinases; MMP: matrix metalloproteinase; ECM: extracellular matrix; VSMCs: vascular smooth muscle cells.