Table 1.
Questions for each of the 10 topics.
| Topic | Questions |
|---|---|
| Blood gas analysis | Please characterize the acid-base issue in this arterial blood gas: pH 7.21, Pco2 62 mm Hg, Po2 80 mm Hg, and HCO3 23 mEq/dL. |
| How do the values for Pco2 and pH differ on a venous compared with an arterial blood gas? | |
| A patient who is in severe septic shock requiring 2 vasoactive agents has a mixed venous saturation of 82% obtained from a central venous line. His arterial oxygen saturation is 92%. The lactate level is 4 mmol/dL (normal < 2 mmol/dL). How does this information help in managing the patient? | |
| Please list 2 sampling errors that result in an inaccurate arterial blood gas (ABG). | |
| Dr Cook climbs Mt. Everest without supplemental oxygen and then checks his ABG. What do you predict his arterial Po2 will be at the pinnacle of the mountain where the atmospheric pressure is 253 mm Hg? | |
| Asthma | List 3 pathophysiologic abnormalities associated with airway obstruction in an asthma exacerbation. |
| A 5-year-old boy reports that he feels easier to breathe while receiving continuous nebulized albuterol. His pulse oximeter reading has dropped from 94% to 90%, but on auscultation, he has improved aeration. How do you explain his decreased oxygenation? | |
| After intubating a 4-year-old boy for status asthmatics (wt = 20 kg) and hypoxemia, the respiratory therapist asks what respiratory rate should he set on the mechanical ventilator. What rate would you choose and why? | |
| Please list 3 side effects of albuterol that a nurse might call you about. | |
| You are admitting a child who has a severe asthma exacerbation. While examining her, you notice that her systolic blood pressure decreases by 18 mm Hg on inspiration. What is this finding called and why does it occur? | |
| Diabetic ketoacidosis | Why are patients with diabetic ketoacidosis (DKA) dehydrated on presentation? What is the recommended strategy for rehydration? |
| What is the corrected serum sodium (mEq/dL) for a patient who has DKA, a blood glucose of 500 mg/dL, and a measured serum sodium of 125 mEq/dL? | |
| What is the goal rate to decrease the blood glucose level (mg/dL/h) when treating a patient with DKA? Why is this important? | |
| In patients with moderate or severe DKA, why should the insulin drip be continued even after the hyperglycemia has resolved? | |
| A nurse reports that your newly admitted DKA patient who previously had a normal mental status examination has now become extremely agitated and combative. Why do you think this is happening? What would be the most appropriate course of action? | |
| Electrolyte abnormalities | You receive a call from an Emergency Department (ED) physician who is taking care of a 9-month-old infant (wt = 5 kg) with ongoing seizure activity. Her serum sodium is 120 mEq/dL. What specific instructions would you give to the ED physician? |
What electrolyte derangement can result in this electrocardiogram finding?
|
|
| You are caring for a 5-year-old boy with hypernatremia from dehydration. His initial serum sodium was 162 mEq/L. After having been placed on ¼ normal saline at 1.5 times maintenance rate for 3 hours, you notice that he is having a seizure. What do you think is the cause of this seizure and what treatment would you order? | |
| List 3 treatment options for hyperkalemia. | |
| What laboratory test(s) would it be appropriate to order to support a diagnosis of Syndrome of Inappropriate Antidiuretic Hormone Secretion (SIADH)? | |
| Traumatic brain injury and intracranial pressure management | Cerebral perfusion pressure (CPP) is calculated as x − y. What are x and y? |
| What is Cushing triad and what does this sign suggest? | |
| Please list 4 treatments that you can use to manage a patient who has increased intracranial pressure (ICP). | |
| A 16-year-old boy has a ruptured cerebral arteriovenous malformation and is on a mechanical ventilator. He has an intracranial pressure monitor and you are managing his intracranial pressure while awaiting surgery planned for tomorrow. His current ICP is 15 mm Hg. You notice that his Pco2 on an ABG is 20 mm Hg. How does this Pco2 affect cerebral blood flow and is this level in the recommended range? | |
| Describe one mechanism of action of intravenous mannitol when administered to lower ICP. | |
| Mechanical ventilation | A respiratory therapist shows you that the peak inspiratory pressure (PIP) for a patient with pneumonia on volume control mode ventilation now measures 38 cmH2O with an exhaled tidal volume of 6 mL/kg. Yesterday, the PIP measured 25 cmH2O with the same tidal volume. List three possible reasons for this change. |
| You just intubated a 13-year-old girl (wt = 50 kg) for hypoxemia due to pneumonia. She has no spontaneous breaths. The initial venous blood gas shows pH 7.20, Pco2 60 mm Hg, and Po2 55 on ventilator settings of tidal volume 400 ml, respiratory rate 10 per minute, positive end-expiratory pressure (PEEP) 7, pressure support 8, and FiO2 40% with oxygen saturation of 96%. What setting might you change to improve her blood gas? | |
| Describe the difference between synchronized intermittent mandatory ventilation (SIMV) volume control and SIMV pressure control modes on a mechanical ventilator. | |
| What endotracheal tube size would you choose to intubate a 5-year-old girl who weighs 10 kg? | |
| Please list 2 things that you can modify to improve oxygenation on a patient who is being mechanically ventilated. | |
| Respiratory failure | Define “respiratory failure.” |
| You are called to assess a 15-month-old girl on the wards who was admitted for pneumonia. In reviewing her chart, you note that she is more tachypneic and is currently hypoxemic on a 50% mask with grunting despite treatment with BiPAP. You order a STAT venous blood gas which shows pH 7.12, Pco2 80 mm Hg and HCO3 26 mEq/dL. Her CXR shows interval decrease in aeration with bilateral whiteout. What would you do next? | |
| A medical student asks you, “Why is it that we order to keep the patient’s pulse oximeter level above 90%? Is there a physiological reason for this?” How would you answer this question? | |
| List 3 things you can do to confirm tracheal placement of an endotracheal tube. | |
| You are called to a rapid response for an 8-month-old infant who was admitted to the ward for RSV bronchiolitis. She appears to be struggling to breathe despite aggressive suctioning. You try an albuterol treatment without improvement. She is breathing 80 times a minute and grunting with severe intercostal retractions. Her pulse oximetry is 92% while on 10 L/min of 100% oxygen provided via facemask. You obtain a CXR which shows peribronchial haziness and hyperexpansion. A capillary blood gas shows a pH 7.34, Pco2 44 mm Hg and HCO3 23 mEq/dL. What would you do next? | |
| Septic shock | Define shock. |
| List 2 signs of warm shock that differentiate it from cold shock. | |
| What is(are) the preferred vasoactive agent(s) to treat a patient in warm shock who is hypotensive? | |
| What is the difference between compensated vs uncompensated shock? | |
| How much fluid would you expect to give to a patient who is in septic shock during the initial resuscitation? | |
| Seizures | Please list 2 electrolyte derangements that can cause seizures. |
| A nurse calls to tell you that a 3-year-old boy (wt = 15 kg) just transferred from the ward due to a complex febrile seizure has been experiencing seizure for the last 5 minutes. What medication should you order? At what dosage and how fast would you want to give it? | |
| After receiving 3 rounds of a first line agent for status epilepticus, a patient is still experiencing seizure. Please list 2 second line agents you can use next. | |
| You are called to assess a 5-year-old boy (wt = 20 kg) with Lennox-Gastaut Syndrome who just received 1 dose of lorazepam intravenous for a prolonged seizure. The nurse is concerned that the patient is now snoring. The pulse oximeter is reading 93% and the patient is breathing 10 times/min. You immediately check a capillary blood gas which shows pH 7.25, Pco2 62 mm Hg, and HCO3 23 mEq/dL. What can you do to improve his respiratory status? | |
| A new nurse wants to know how fast she can give the Fosphenytoin intravenous you just ordered. How fast would you want to give the drug and why? | |
| Upper airway obstruction | Where is the narrowest anatomical portion of the airway of a 4-year-old boy? |
| Please list the 2 most common congenital causes of stridor in infants. | |
| A nurse calls to report that the patient who was recently extubated now has stridor. What does this finding suggest and what can you do to treat it? | |
| Stridor is a high-pitched sound heard most prominently during which phase of breathing? Why is it heard during this phase? | |
Please list 3 signs and symptoms that a child with this X-ray might have.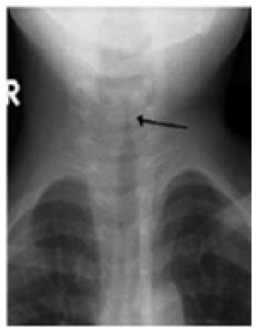
|
Abbreviations: CPP, cerebral perfusion pressure; EKG, electrocardiography; PIP, peak inspiratory pressure; CXR, chest X-ray
