Abstract
Background
Postoperative/adjuvant radiotherapy of advanced gastric cancer involves a large planning target volume (PTV) with multi-concave shapes which presents a challenge for volumetric modulated arc therapy (VMAT) planning. This study investigates the advantages of automated VMAT planning for this site compared to manual VMAT planning by expert planners.
Methods
For 20 gastric cancer patients in the postoperative/adjuvant setting, dual-arc VMAT plans were generated using fully automated multi-criterial treatment planning (autoVMAT), and compared to manually generated VMAT plans (manVMAT). Both automated and manual plans were created to deliver a median dose of 45 Gy to the PTV using identical planning and segmentation parameters. Plans were evaluated by two expert radiation oncologists for clinical acceptability. AutoVMAT and manVMAT plans were also compared based on dose-volume histogram (DVH) and predicted normal tissue complication probability (NTCP) analysis.
Results
Both manVMAT and autoVMAT plans were considered clinically acceptable. Target coverage was similar (manVMAT: 96.6 ± 1.6%, autoVMAT: 97.4 ± 1.0%, p = 0.085). With autoVMAT, median kidney dose was reduced on average by > 25%; (for left kidney from 11.3 ± 2.1 Gy to 8.9 ± 3.5 Gy (p = 0.002); for right kidney from 9.2 ± 2.2 Gy to 6.1 ± 1.3 Gy (p < 0.001)). Median dose to the liver was lower as well (18.8 ± 2.3 Gy vs. 17.1 ± 3.6 Gy, p = 0.048). In addition, Dmax of the spinal cord was significantly reduced (38.3 ± 3.7 Gy vs. 31.6 ± 2.6 Gy, p < 0.001). Substantial improvements in dose conformity and integral dose were achieved with autoVMAT plans (4.2% and 9.1%, respectively; p < 0.001). Due to the better OAR sparing in the autoVMAT plans compared to manVMAT plans, the predicted NTCPs for the left and right kidney and the liver-PTV were significantly reduced by 11.3%, 12.8%, 7%, respectively (p ≤ 0.001). Delivery time and total number of monitor units were increased in autoVMAT plans (from 168 ± 19 s to 207 ± 26 s, p = 0.006) and (from 781 ± 168 MU to 1001 ± 134 MU, p = 0.003), respectively.
Conclusions
For postoperative/adjuvant radiotherapy of advanced gastric cancer, involving a complex target shape, automated VMAT planning is feasible and can substantially reduce the dose to the kidneys and the liver, without compromising the target dose delivery.
Electronic supplementary material
The online version of this article (10.1186/s13014-018-1032-z) contains supplementary material, which is available to authorized users.
Keywords: VMAT, Automated planning, NTCP, Gastric cancer
Background
In the Intergroup Study 0116 (INT-0116) study, adjuvant chemoradiotherapy (CRT) improved overall survival and progression-free survival in patients with gastric cancer compared to surgery alone [1, 2]. The benefit of combined modality treatment was later confirmed in Asian studies with D2-resected patients [3–5]. European trials in gastroesophageal junction cancers showed survival benefits compared to surgery with neoadjuvant CRT [6] or perioperative chemotherapy without radiotherapy [7, 8]. Randomized trials comparing adjuvant CRT to (perioperative) chemotherapy indicated clinical benefits for CRT in subgroups, but failed in showing a consistent benefit in European and Asian trials [3, 5, 9, 10]. Therefore, the role of adjuvant CRT in gastric carcinoma compared to other approaches, such as perioperative chemotherapy, is not yet clearly defined [9]. The use of modern radiotherapy approaches might improve the risk−/benefit ratio in favor of radiotherapy in gastric carcinoma. Recent data showed the feasibility of using intensity-modulated radiation therapy (IMRT) or volumetric modulated arc therapy (VMAT) for this purpose [3, 10–12]. Postoperative radiotherapy of advanced gastric cancer involves a large target volume with multi-concave shapes which presents a challenge for VMAT planning with a risk of protocol deviations. In a similar setting, radiotherapy for esophageal carcinoma indicated that the experience of the treatment planner may largely affect plan quality, as shown by large differences in plan quality among planners within one institute [13]. In such a setting, automated treatment planning might have several advantages, including facilitated central review in clinical trials as well as improvement of less experienced treatment planner’s performance.
Over the years, in-house developed as well as commercial algorithms have attempted to automate the trial-and-error process in order to create optimal plans, reduce user variability and improve the quality and efficiency of the resulting plans. Knowledge-based planning uses a model library of previously generated plans to predict new treatment plan parameters [14, 15], while multi-criterial optimization generates a set of Pareto-optimal plans [16, 17]. Erasmus-iCycle is an optimizer for fully automated multi-criterial beam profile optimization and beam angle selection for coplanar and non-coplanar IMRT, developed at the Erasmus MC Cancer Institute [18–22]. In combination with the Monaco treatment planning system (TPS), Erasmus-iCycle is currently used in clinical practice for IMRT and VMAT plan generation for prostate, head and neck, cervical and lung cancer patients [19–22]. Several studies on postoperative gastric cancer patients have dosimetrically evaluated different radiotherapy techniques [23–26]. To our knowledge, no study has been published considering the feasibility and advantages of automated treatment planning for this treatment site. In this study, we investigated to what extent automated treatment planning using Erasmus-iCycle results in improved VMAT plan quality for advanced gastric cancer patients compared to plan generation by an expert planner.
Methods
Patients
A total of 20 patients with advanced gastric cancer who received radiotherapy treatment were included in the study. Clinical details are shown in Additional file 1: Table S1. Written informed consent was obtained from all patients for anonymized usage of treatment planning data. Our study protocol for retrospective evaluation of automated planning using Erasmus-iCycle was approved by the ethics committee of Heidelberg University, Medical Faculty Mannheim (2016-806R-MA).
Treatment plan generation
All manually and automatically generated dual-arc VMAT plans (manVMAT and autoVMAT, respectively) were prescribed to deliver a median dose of 45 Gy to the target in 25 fractions. The primary planning objective was achieving adequate PTV coverage while maximally sparing the organs at risk. All plans were generated for delivery at a VersaHD linear accelerator (Elekta AB, Stockholm, Sweden), equipped with an Agility multi-leaf collimator and a photon beam energy of 10 MV.
All manVMAT plans were generated by expert treatment planners with the Monaco TPS, version 5.11 (Elekta AB, Stockholm, Sweden) using template-based optimization cost-functions. The employed optimization template is set according to the current clinical guidelines used at the Medical University of Mannheim. For each patient, the optimization cost-functions’ parameters were iteratively tweaked to improve the dose distribution and achieve optimal target coverage while respecting OAR constraints. As explained below, also the final autoVMAT plans were generated with Monaco, for which we used the same software version. All Monte Carlo dose calculations in Monaco were performed using a 1% dose variance, and a dose grid resolution of 3 mm. A maximum of 140 control points per arc was allowed. Also the other segmentation settings were kept identical for manual and automated plan generation.
Automated multi-criterial VMAT plan generation with Erasmus-iCycle/Monaco
The in-house developed Erasmus-iCycle/Monaco platform for fully automated multi-criteria plan generation [18–22] was configured to generate clinically deliverable VMAT plans for gastric cancer. For each of the study patients, Erasmus-iCycle was used to first automatically generate a Pareto-optimal plan with clinically favorable trade-offs between treatment objectives using a “wish-list” developed for gastric cancer (as detailed below in Table 1). Based on this Erasmus-iCycle plan, a patient-specific Monaco template was then created fully automatically, to be used in the Monaco TPS for automated generation of a deliverable dual-arc VMAT plan that mimicked the initial Erasmus-iCycle plan. The applied wish-list contains constraints to be strictly fulfilled, and clinical plan objectives with ascribed priorities to be met as closely as possible or superseded (see Table 1 for details). Three constraints were used to control the maximum dose in the PTV and the patient (i.e., the outline of the patient’s external surface including the PTV, delineated OARs and the unspecified tissues), as well as the dose conformity outside the PTV. In order to achieve a homogeneous and adequate PTV dose coverage, the highest priority objective was given to the PTV using the Logarithmic Tumor Control Probability function (LTCP) [27], followed by a shell around the PTV to ensure a steep gradient outside the PTV (priority 2). In line with the clinical practice, minimizing the mean dose in the kidneys was the organ-at-risk (OAR) objective with highest priority (priority 3), followed by the mean dose in the liver (priority 4). Subsequently, equivalent uniform dose (EUD) objectives with volume effect parameters (k = 6 and 12) [28], focusing on reduction of the midrange and high dose in the heart and spinal cord were used (priorities 5 and 6), respectively. To control the dose conformity and entrance dose, a shell at 18 mm from the PTV, as well as a skin ring of 21 mm wide from the body contour towards the patient’s internal were defined (priority 7). Additionally, dose-volume objectives for the kidneys, liver, and the lungs were used with lower priorities.
Table 1.
Applied wish-list for automatic VMAT plan generation for gastric cancer patients
| Constraints | ||||
| Volume | Type | Limit | ||
| PTV | Maximum | 105% of Dp | ||
| PTV Shell 39 mm | Maximum | 50% of Dp | ||
| Patient | Maximum | 105% of Dp | ||
| Objectives | ||||
| Priority | Volume | Type | Goal | Parameters |
| 1 | PTV | ↓ LTCP | 0.4 | Dp=45 Gy,α = 4 |
| 2 | PTV Shell 3 mm | ↓ Maximum | 90% of Dp | |
| 3 | Left and Right Kidney | ↓ Mean | 8 Gy | |
| 4 | Liver | ↓ Mean | 15 Gy | |
| 5 | Heart | ↓ EUD | 15 Gy | k = 6 |
| 6 | Spinal Cord | ↓ EUD | 25 Gy | k = 12 |
| 7 | PTV Shell 18 mm | ↓ Maximum | 40% of Dp | |
| Skin Ring | ↓ Maximum | 25% of Dp | 21 mm | |
| 8 | Left and Right Kidney | ↓ Volume-Dose | 25% | 12 Gy |
| Liver | ↓ Volume-Dose | 30% | 24 Gy | |
| 9 | Left and Right Lung | ↓ Volume-Dose | 50% | 20 Gy |
Abbreviations: Dp prescribed dose, LTCP Logarithmic Tumor Control Probability, α cell sensitivity parameter to achieve adequate target coverage, EUD Equivalent Uniform Dose, k volume parameter
Plan evaluation and comparison
All plans were evaluated by expert radiation oncologists (FL, JBH, and DB) for clinical acceptability. For fair dosimetric plan comparisons, all manVMAT and autoVMAT plans were first normalized to obtain equal median PTV dose (i.e., D50% = 45 Gy). In accordance with the International Commission on Radiation Units and Measurements Report No. 83, near-minimum and near-maximum doses (D98% and D2%, respectively) in the PTV were evaluated, from which the homogeneity index (HI = (D2% - D98%)/D50%) was computed. Additionally, dose conformity was estimated by calculating the conformity index (CI = (TVRI)2/(TV*VRI)), i.e., ratio of the target volume covered by the reference isodose level (TVRI) to the target volume (TV) and volume of the reference isodose (VRI). Quantitative analyses of OAR doses included Dmean, D30%, D50%, D60% in the kidneys and the liver-PTV, mean and maximum doses (Dmean, and Dmax) in the spinal cord and the heart, volumes of the kidneys receiving more than 12 Gy (V12Gy) and 20 Gy (V20Gy) [29], volumes of the liver-PTV receiving more than 24 Gy (V24Gy) and 30 Gy (V30Gy), and Dmean in the lungs and volumes of the lungs receiving more than 5 Gy (V5Gy) and 20 Gy (V20Gy) [30]. In addition, integral patient doses were evaluated by assessing patient Dmean and volumes receiving V5Gy, V11.25Gy and V22.5Gy. Estimated treatment delivery time and total number of monitor units (MUs) for each plan were also quantified.
From the DVHs, normal tissue complication probabilities (NTCPs) for the kidneys and the liver were estimated using the Lyman-Burman-Kutcher NTCP model for late effects, considering tolerance dose TD50/5 = 12 Gy, n = 0.70, m = 0.26 for the kidneys [29], and TD50/5 = 30 Gy, n = 0.32, m = 0.15 for liver failure [31], where TD50/5 refers to the dose to the whole organ which lead to complication in 50% of the population at 5 years, m relates to the steepness of the dose-response curve, and n represents the volume effect in the LKB model. For this purpose, all plans were first normalized to 1.5 Gy per fraction using α/β = 2.5 Gy.
Differences in dosimetric parameters between manVMAT and autoVMAT plans were analyzed using SPSS software v.21 (SPSS, Inc., Chicago, USA) and presented as the mean ± 1 standard deviation. Paired two-sided Wilcoxon Signed-rank tests were performed to assess statistical significance of observed differences, considering p < 0.05 statistically significant.
Results
Target volume dosimetric evaluations
All automatically and manually generated VMAT plans were clinically acceptable and achieved adequate target coverage. Clinical acceptability of the plans was evaluated by radiation oncologists with experience in gastric cancer treatment (JBH, FL and DB). Differences between the autoVMAT and manVMAT plans in V95% or D98% were not statistically significant (Table 2). However, autoVMAT plans exhibited a significantly lower near-maximum dose in the PTV, resulting in a better target dose homogeneity (0.09 ± 0.01 vs. 0.10 ± 0.02 (p = 0.003)). For autoVMAT, the dose conformity was significantly improved as well (0.91 ± 0.02 vs. 0.88 ± 0.03 (p < 0.001)). As an example, Fig. 1a shows the resulting dose distributions from the autoVMAT and manVMAT plans for patient 8. As is evident from this figure and the corresponding dose-volume histograms in Fig. 1b, AutoVMAT resulted in favorable dose conformity and better OAR sparing.
Table 2.
Comparison of dosimetric parameters between autoVMAT and manVMAT plans. Population mean values for the 20 study patients and corresponding standard deviations are reported
| Structure | Parameter | autoVMAT | manVMAT – autoVMAT | |
|---|---|---|---|---|
| Mean ± SD | Mean diff. ± SD | p-value | ||
| PTV | V95% (%) | 97.4 ± 1.0 | - 0.8 ± 1.7 | 0.085 |
| D98% (Gy) | 42.5 ± 0.5 | - 0.2 ± 0.7 | 0.14 | |
| D2% (Gy) | 46.3 ± 0.1 | 0.5 ± 0.2 | < 0.001 | |
| HI | 0.09 ± 0.01 | 0.02 ± 0.02 | 0.003 | |
| CI | 0.91 ± 0.02 | - 0.04 ± 0.03 | < 0.001 | |
| Left Kidney | Dmean (Gy) | 12.7 ± 4.3 | 1.8 ± 1.6 | 0.001 |
| D30% (Gy) | 14.9 ± 8.1 | 2.1 ± 3.3 | 0.013 | |
| D50% (Gy) | 8.9 ± 3.5 | 2.4 ± 2.2 | 0.002 | |
| D60% (Gy) | 7.3 ± 1.9 | 2.4 ± 1.4 | < 0.001 | |
| V12Gy (%) | 32.2 ± 14.0 | 11.7 ± 7.7 | < 0.001 | |
| V20Gy (%) | 19.2 ± 13.2 | 1.0 ± 3.9 | 0.117 | |
| NTCP (%) | 45.1 ± 35.8 | 11.3 ± 10.9 | 0.001 | |
| Right Kidney | Dmean (Gy) | 7.5 ± 1.7 | 3.0 ± 1.2 | < 0.001 |
| D30% (Gy) | 7.8 ± 1.7 | 4.1 ± 1.6 | < 0.001 | |
| D50% (Gy) | 6.1 ± 1.3 | 3.1 ± 1.3 | < 0.001 | |
| D60% (Gy) | 5.5 ± 1.2 | 2.7 ± 1.1 | < 0.001 | |
| V12Gy (%) | 12.4 ± 4.8 | 18.9 ± 8.4 | < 0.001 | |
| V20Gy (%) | 3.8 ± 2.8 | 3.0 ± 2.8 | 0.001 | |
| NTCP (%) | 4.2 ± 3.8 | 12.8 ± 7.2 | < 0.001 | |
| Liver - PTV | Dmean (Gy) | 18.6 ± 3.3 | 1.8 ± 2.8 | 0.02 |
| D30% (Gy) | 21.9 ± 4.1 | 2.8 ± 3.2 | 0.003 | |
| D50% (Gy) | 17.1 ± 3.6 | 1.7 ± 3.3 | 0.048 | |
| D60% (Gy) | 15.1 ± 3.4 | 1.2 ± 3.3 | 0.14 | |
| V24Gy (%) | 25.4 ± 11.6 | 7.1 ± 8.8 | 0.004 | |
| V30Gy (%) | 12.9 ± 6.0 | 4.7 ± 4.6 | 0.001 | |
| NTCP (%) | 31.1 ± 23.2 | 7.0 ± 7.0 | 0.001 | |
| Heart | Dmean (Gy) | 12.7 ± 4.7 | 0.7 ± 1.8 | 0.117 |
| Dmax (Gy) | 46.8 ± 0.6 | 0.8 ± 1.2 | 0.009 | |
| Spinal cord | Dmean (Gy) | 13.9 ± 2.6 | 2.9 ± 1.5 | < 0.001 |
| Dmax (Gy) | 31.6 ± 2.6 | 6.7 ± 3.2 | < 0.001 | |
| Left Lung | Dmean (Gy) | 7.3 ± 3.2 | 0.6 ± 0.3 | < 0.001 |
| V5Gy (%) | 32.7 ± 15.6 | 1.4 ± 1.0 | < 0.001 | |
| V20Gy (%) | 14.0 ± 7.2 | 2.2 ± 1.8 | < 0.001 | |
| Right Lung | Dmean (Gy) | 5.4 ± 3.3 | 0.3 ± 0.5 | 0.013 |
| V5Gy (%) | 31.2 ± 16.8 | 1.1 ± 2.1 | 0.01 | |
| V20Gy (%) | 7.0 ± 7.6 | 0.8 ± 1.8 | 0.078 | |
| Patient | Dmean (Gy) | 9.4 ± 1.9 | 0.5 ± 0.3 | < 0.001 |
| V5Gy (%) | 40.2 ± 8.9 | 1.6 ± 0.8 | < 0.001 | |
| V11.25Gy (%) | 30.0 ± 6.6 | 1.8 ± 1.7 | 0.001 | |
| V22.5Gy (%) | 16.2 ± 3.3 | 1.5 ± 1.1 | < 0.001 | |
Abbreviations: HI homogeneity index, CI conformity index, NTCP normal tissue complication probability
Fig. 1.
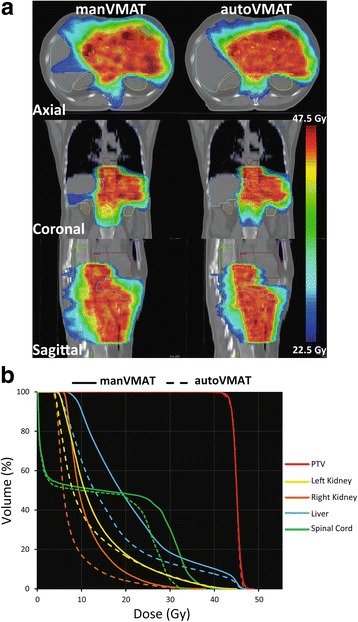
a Comparison of dose distributions for the manVMAT (left) and autoVMAT plans (right) for patient 8 on the axial, coronal and sagittal planes, (b) dose volume histograms for the manVMAT (solid lines) and the autoVMAT (dashed lines) plans of this patient
Organs at risk dosimetric evaluations
Figure 2 shows the observed absolute differences in dosimetric parameters for each of the study patients. Overall, autoVMAT plans had more favorable dose distributions, resulting in reduced dose delivery to the kidneys, liver, spinal cord, heart and lungs, without deteriorating the PTV dose coverage (Table 2 and Fig. 2). Median doses (D50%) to the left kidney, right kidney, and liver-PTV were significantly reduced by 28% (from 11.3 ± 2.1 Gy to 8.9 ± 3.5 Gy, p = 0.002), 39% (from 9.2 ± 2.2 Gy to 6.1 ± 1.3 Gy, p < 0.001), and 11% (from 18.8 ± 2.3 Gy to 17.1 ± 3.6 Gy, p = 0.048), respectively. The V20Gy for the left and right kidney with autoVMAT were lower than those for the manVMAT plans (Table 2). In addition, the V30Gy for the liver-PTV was significantly decreased with autoVMAT plans by 36% (from 17.7 ± 6.2% to 12.9 ± 6.0%, p = 0.001). The maximum dose in the spinal cord was on average reduced by 6.7 ± 3.2 Gy (p < 0.001) with autoVMAT. Furthermore, the integral dose in the patient and the dose conformity were also significantly better with autoVMAT (Table 2).
Fig. 2.
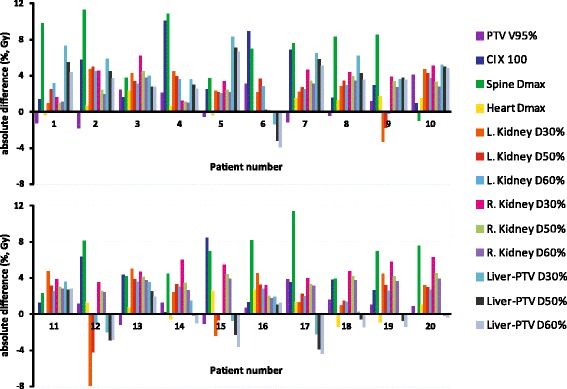
Differences in dosimetric plan parameters between autoVMAT and manVMAT plans for each of the 20 study patients. Positive values are in favor of the autoVMAT plans
NTCPs evaluations
The published sets of parameters used for calculations of NTCPs for the kidneys and liver-PTV resulted in overall lower probability of late complications with autoVMAT compared to manVMAT plans. In 16/20 patients, the predicted NTCPs were lowest with autoVMAT for the left kidney, whereas all 20 patients had lower predicted NTCPs with autoVMAT for the right kidney (Fig. 3). For 17/20 patients, the NTCP predictions for liver-PTV were lower for the autoVMAT plans. The average NTCP values resulting from autoVMAT, given in Table 2, were significantly reduced by 11.3%, 12.8% and 7% for the left and right kidney and the liver-PTV, respectively.
Fig. 3.
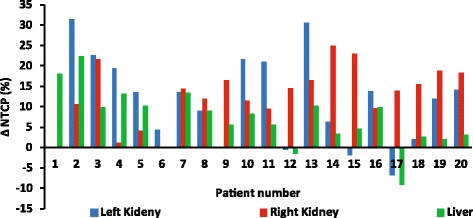
Differences in the predicted normal tissue complication probabilities (NTCP) between autoVMAT and manVMAT plans for the 20 study patients. Positive values are in favor of the autoVMAT plans
Planning and treatment delivery times
All manVMAT plans in this study were generated using template-based manual planning. Hands-on tweaking time of the optimization cost functions was on average 30 min (range 5-60 min). The optimization and dose calculation of autoVMAT plans in Erasmus-iCycle/Monaco was fully automated and therefore did not require any hands-on time.
Compared to manVMAT plans a significantly more MUs were required for delivery of the autoVMAT plans (1001 ± 134 MU vs. 781 ± 168 MU, p = 0.003), resulting in a prolonged (estimated) treatment delivery time (207 ± 26 s vs. 168 ± 19 s, p = 0.006).
Discussion
Gastric cancer is the third leading cause of cancer death in both sexes with yearly 723,000 deaths worldwide [32]. Protocol deviations can reduce clinical efficacy of radiotherapy in complex treatment geometries, like gastric carcinoma. In the centralized review of the INT-0116 study, minor or major protocol deviations were observed in 35% of patients [2]. Even after correction of errors, major protocol deviations were still found in 6.5% of the plans that were actually irradiated [1, 2]. The clinical impact of protocol deviations in INT-0116 has not been reported. However, in other complex geometries it was shown that protocol violations during radiation therapy were correlated with reduced overall survival [33]. Modern radiotherapy approaches such as IMRT and VMAT have several dosimetric advantages but they are associated with increased complexity [9, 34–36]. Very high protocol deviations are therefore possible; for example, RTOG 0529 showed 81% protocol deviations at first plan review [37]. Albeit in small numbers, RTOG 0022 showed local failure rates of 50% (2/4) vs. 6% (3/49) in oropharyngeal cancer patients treated with and without protocol deviations, respectively [38]. Protocol deviations may, amongst other things, be caused by inaccurate delineation or sub-optimal treatment planning. For gastric cancer, the percentage of these deviations is unknown. In a recent report on RTOG 0933 by Gondi et al. [39], unacceptable radiotherapy protocol deviations were observed in 25% of cases at a rapid review process: 11/21 cases had contouring deviations, 5/21 cases had unacceptable planning deviations and 5/21 had unacceptable deviations of contouring and planning. Also in a recent study of Habraken et al. [40] on hepatocellular carcinoma patients, it was demonstrated that pretreatment plan review was important to reduce unacceptable protocol deviations. Additionally, they demonstrated that automated treatment planning could be used to identify sub-optimal treatment plans. This might be especially relevant in trials in which low numbers of patients are eligible or small numbers of patients are treated in a participating hospital.
Over the past years, several studies have investigated the advantages of automated treatment planning compared to manual planning using in-house developed or commercial algorithms [18–22, 41–43]. Treatment planning with Erasmus-iCycle/Monaco is fully automated, and it has been successfully validated for clinical use in several treatment sites including prostate [19], head-and-neck [20], cervix [21], and lung [22]. Knowledge-based planning using a model library of previously generated plans to predict treatment plan parameters for a new patient was configured and tested in pelvic anatomy [41], lung [42], and esophageal cancer [43].
Numerous dosimetric studied have evaluated different radiotherapy techniques for gastric cancer by comparing IMRT, VMAT, helical tomotherapy, 3DCRT and proton therapy [23–26]. Until now, no study has been published showing the possibility/advantages of automated treatment planning for postoperative gastric cancer patients. In this study Erasmus-iCycle was used to automatically generate VMAT plans for gastric cancer patients. For this site, manual treatment optimization is a large challenge, even for an expert planner, due to the multi-concave shape, the extent of the target volume, and the close proximity to many radiosensitive organs (i.e., kidneys, liver, heart, and spinal cord). Another difficulty in postoperative radiotherapy in gastric cancer patients is that radiation tolerance doses of OARs are relatively low. Compared to the manVMAT plans, generated by an expert planner, plan quality was significantly better for the autoVMAT plans, only requiring slightly longer treatment delivery times. Specifically, dose conformity and sparing of organs at risk were improved, while the clinical importance of the observed longer treatment delivery time and the increased MUs is considered to be low. As a result of higher modulation, the number of MUs was significantly higher in the autoVMAT than in manVMAT plans, this could lead to challenges in radiation delivery. The integral dose was significantly reduced in autoVMAT plans, this may be beneficial specially for young patients to avoid secondary tumors, and most notably showed significantly reduced NTCP for liver and both kidneys, although it is not yet clear to what extent the observed dosimetric advantages of autoVMAT vs. an experienced planner will really translate into a clinical benefit. Automated treatment planning can improve the efficiency of the treatment planning process and reduce its user dependency, this in turns might lead to more consistent and uniform outcomes in treatment planning studies and clinical trials. Apart from the improved plan quality and reduced predicted complications, automated planning also eliminated the planning hands-on time required for planning.
Conclusion
Automated treatment planning is of great value for complex treatment sites like for gastric cancer. Compared to manual planning by an expert planner, plan quality could be largely improved, while drastically reducing treatment planning workload.
Additional file
Table S1. Clinical details of patients with gastric carcinoma. (DOCX 15 kb)
Acknowledgments
Funding
This work was in part funded by a research grant of Elekta AB, Stockholm, Sweden.
Availability of data and materials
The dataset generated and analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- autoVMAT
Fully automated volumetric modulated arc therapy (plans)
- CI
Conformity index
- CRT
Chemoradiotherapy
- DVH
Dose-volume histogram
- EUD
Equivalent uniform dose
- HI
Homogeneity index
- IMRT
Intensity-modulated radiation therapy
- INT-0116
Intergroup Study 0116
- LTCP
Logarithmic tumor control probability
- manVMAT
Manually generated volumetric modulated arc therapy (plans)
- MU
Monitor units
- NTCP
Normal tissue complication probability
- OAR
Organ at risk
- PTV
Planning target volume
- RTOG
Radiation Therapy Oncology Group
- TPS
Treatment planning system
- TV
Target volume
- VMAT
Volumetric modulated arc therapy
Authors’ contributions
JBH, DB, and AWMS conceived the study; BJMH, MLPD, and SB provided supervision and assistance with iCycle procedures; OK, JBH, and DB re-contoured OAR and target volumes, if appropriate; FS re-planned clinically irradiated plans with modern planning systems; FW and FL provided assistance with study design and revisions of the manuscript; All authors read and approved the final manuscript.
Ethics approval and consent to participate
The study was approved by the ethics committee of Heidelberg University, Medical Faculty Mannheim (2016-806R-MA). Written informed consent for scientific usage of clinical data was obtained from all patients.
Consent for publication
Consent for scientific usage of clinical data was obtained from all patients included in the study.
Competing interests
Erasmus MC Cancer Institute has research collaborations with Accuray Inc., Sunnyvale, USA.
AWMS reports grants from Elekta AB, Stockholm, Sweden, during the conduct of the study; FS reports personal fees from Elekta AB, Sweden, outside the submitted work; OK has nothing to disclose; BJMH reports grants from Elekta AB, Stockholm, Sweden, during the conduct of the study; grants from Accuray Inc., Sunnyvale, USA, outside the submitted work; MLPD reports grants from Elekta AB, Stockholm, Sweden, during the conduct of the study; SB reports grants from Elekta AB, Stockholm, Sweden, during the conduct of the study; grants from Accuray Inc., Sunnyvale, USA, outside the submitted work; FW reports research grants and travel support from Elekta, during the conduct of the study; FL has nothing to disclose; JBH reports teaching honoraria from Elekta AB, Stockholm, Sweden, during the conduct of the study; DB reports personal fees from Siemens AG, personal fees from NB Capital ApS, outside the submitted work.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Footnotes
Electronic supplementary material
The online version of this article (10.1186/s13014-018-1032-z) contains supplementary material, which is available to authorized users.
Contributor Information
Abdul Wahab M. Sharfo, Phone: +31107041064, Email: a.sharfo@erasmusmc.nl
Florian Stieler, Email: florian.stieler@umm.de.
Oskar Kupfer, Email: oskar.kupfer@freenet.de.
Ben J. M. Heijmen, Email: b.heijmen@erasmusmc.nl
Maarten L. P. Dirkx, Email: m.dirkx@erasmusmc.nl
Sebastiaan Breedveld, Email: s.breedveld@erasmusmc.nl.
Frederik Wenz, Email: frederik.wenz@umm.de.
Frank Lohr, Email: lohr.frank@policlinico.mo.it.
Judit Boda-Heggemann, Email: judit.boda-heggemann@umm.de.
Daniel Buergy, Email: daniel.buergy@umm.de.
References
- 1.Macdonald JS, Smalley SR, Benedetti J, et al. Chemoradiotherapy after surgery compared with surgery alone for adenocarcinoma of the stomach or gastroesophageal junction. N Engl J Med. 2001;345:725–730. doi: 10.1056/NEJMoa010187. [DOI] [PubMed] [Google Scholar]
- 2.Smalley SR, Benedetti JK, Haller DG, et al. Updated analysis of SWOG-directed intergroup study 0116: a phase III trial of adjuvant radiochemotherapy versus observation after curative gastric cancer resection. J Clin Oncol. 2012;30:2327–2333. doi: 10.1200/JCO.2011.36.7136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zhu WG, Xua DF, Pu J, et al. A randomized, controlled, multicenter study comparing intensity-modulated radiotherapy plus concurrent chemotherapy with chemotherapy alone in gastric cancer patients with D2 resection. Radiother Oncol. 2012;104:361–366. doi: 10.1016/j.radonc.2012.08.024. [DOI] [PubMed] [Google Scholar]
- 4.Lee J, Lim DH, Kim S, et al. Phase III trial comparing capecitabine plus cisplatin versus capecitabine plus cisplatin with concurrent capecitabine radiotherapy in completely resected gastric cancer with D2 lymph node dissection: the ARTIST trial. J Clin Oncol. 2012;30:268–273. doi: 10.1200/JCO.2011.39.1953. [DOI] [PubMed] [Google Scholar]
- 5.Park SH, Sohn TS, Lee J, et al. Phase III trial to compare adjuvant chemotherapy with Capecitabine and cisplatin versus concurrent chemoradiotherapy in gastric Cancer: final report of the adjuvant chemoradiotherapy in stomach tumors trial, including survival and subset analyses. J Clin Oncol. 2015;33:3130–3136. doi: 10.1200/JCO.2014.58.3930. [DOI] [PubMed] [Google Scholar]
- 6.van Hagen P, Hulshof MC, van Lanschot JJ, et al. Preoperative chemoradiotherapy for esophageal or junctional cancer. N Engl J Med. 2012;366:2074–2084. doi: 10.1056/NEJMoa1112088. [DOI] [PubMed] [Google Scholar]
- 7.Ychou M, Boige V, Pignon JP, et al. Perioperative chemotherapy compared with surgery alone for resectable gastroesophageal adenocarcinoma: an FNCLCC and FFCD multicenter phase III trial. J Clin Oncol. 2011;29:1715–1721. doi: 10.1200/JCO.2010.33.0597. [DOI] [PubMed] [Google Scholar]
- 8.Cunningham D, Allum WH, Stenning SP, et al. Perioperative chemotherapy versus surgery alone for resectable gastroesophageal cancer. N Engl J Med. 2006;355:11–20. doi: 10.1056/NEJMoa055531. [DOI] [PubMed] [Google Scholar]
- 9.Buergy D, Lohr F, Baack T, et al. Radiotherapy for tumors of the stomach and gastroesophageal junction--a review of its role in multimodal therapy. Radiat Oncol. 2012;7:192. doi: 10.1186/1748-717X-7-192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Verheij M, Jansen E, Cats A, et al. A multicenter randomized phase III trial of neo-adjuvant chemotherapy followed by surgery and chemotherapy or by surgery and chemoradiotherapy in resectable gastric cancer: first results from the CRITICS study. J Clin Oncol. 2016;34(15_suppl):4000. [Google Scholar]
- 11.Boda-Heggemann J, Weiss C, Schneider V, et al. Adjuvant IMRT/XELOX radiochemotherapy improves long-term overall- and disease-free survival in advanced gastric cancer. Strahlenther Onkol. 2013;189:417–423. doi: 10.1007/s00066-013-0309-2. [DOI] [PubMed] [Google Scholar]
- 12.Dikken JL, van Sandick JW, Maurits Swellengrebel HA, et al. Neo-adjuvant chemotherapy followed by surgery and chemotherapy or by surgery and chemoradiotherapy for patients with resectable gastric cancer (CRITICS) BMC Cancer. 2011;11:329. doi: 10.1186/1471-2407-11-329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Berry SL, Boczkowski A, Ma R, Mechalakos J, Hunt M. Interobserver variability in radiation therapy plan output: results of a single-institution study. Pract Radiat Oncol. 2016;6:442–449. doi: 10.1016/j.prro.2016.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Appenzoller LM, Michalski JM, Thorstad WL, Mutic S, Moore KL. Predicting dose-volume histograms for organs-at-risk in IMRT planning. Med Phys. 2012;39:7446–7461. doi: 10.1118/1.4761864. [DOI] [PubMed] [Google Scholar]
- 15.Yuan L, Ge Y, Lee WR, Yin FF, Kirkpatrick JP, Wu QJ. Quantitative analysis of the factors which affect the interpatient organ-at-risk dose sparing variation in IMRT plans. Med Phys. 2012;39:6868–6878. doi: 10.1118/1.4757927. [DOI] [PubMed] [Google Scholar]
- 16.Monz M, Kufer KH, Bortfeld TR, Thieke C. Pareto navigation: algorithmic foundation of interactive multi-criteria IMRT planning. Phys Med Biol. 2008;53:985–998. doi: 10.1088/0031-9155/53/4/011. [DOI] [PubMed] [Google Scholar]
- 17.Breedveld S, Storchi PR, Keijzer M, Heemink AW, Heijmen BJM. A novel approach to multi-criteria inverse planning for IMRT. Phys Med Biol. 2007;52:6339–6353. doi: 10.1088/0031-9155/52/20/016. [DOI] [PubMed] [Google Scholar]
- 18.Breedveld S, Storchi PRM, Voet PWJ, Heijmen BJM. Icycle: integrated, multicriterial beam angle, and profile optimization for generation of coplanar and noncoplanar IMRT plans. Med Phys. 2012;39:951–963. doi: 10.1118/1.3676689. [DOI] [PubMed] [Google Scholar]
- 19.PWJ V, MLP D, Breedveld S, Al-Mamgani A, Incrocci L, BJM H. Fully automated volumetric modulated arc therapy plan generation for prostate cancer patients. Int J Radiat Oncol Biol Phys. 2014;88:1175–1179. doi: 10.1016/j.ijrobp.2013.12.046. [DOI] [PubMed] [Google Scholar]
- 20.Voet PWJ, Dirkx MLP, Breedveld S, Fransen D, Levendag PC, Heijmen BJM. Toward fully automated multicriterial plan generation: a prospective clinical study. Int J Radiat Oncol Biol Phys. 2013;85:866–872. doi: 10.1016/j.ijrobp.2012.04.015. [DOI] [PubMed] [Google Scholar]
- 21.Sharfo AWM, Breedveld S, Voet PWJ, et al. Validation of fully automated VMAT plan generation for library-based plan-of-the-day cervical cancer radiotherapy. PLoS One. 2016;11:e0169202. doi: 10.1371/journal.pone.0169202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Della Gala G, Dirkx ML, Hoekstra N, et al. Fully automated VMAT treatment planning for advanced-stage NSCLC patients. Strahlenther Onkol. 2017;193:402–409. doi: 10.1007/s00066-017-1121-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Li Z, Zeng J, Wang Z, Zhu H, Wei Y. Dosimetric comparison of intensity modulated and volumetric arc radiation therapy for gastric cancer. Oncol Lett. 2014;8:1427–1434. doi: 10.3892/ol.2014.2363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zhang T, Liang ZW, Han J, Bi JP, Yang ZY, Ma H. Double-arc volumetric modulated therapy improves dose distribution compared to static gantry IMRT and 3D conformal radiotherapy for adjuvant therapy of gastric cancer. Radiat Oncol. 2015;19:114. doi: 10.1186/s13014-015-0420-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Onal C, Dolek Y, Akkus YB. Dosimetric comparison of 3-dimensional conformal radiotherapy, volumetric modulated arc therapy, and helical tomotherapy for postoperative gastric cancer patients. Jpn J Radiol. 2018;36:30–39. doi: 10.1007/s11604-017-0696-x. [DOI] [PubMed] [Google Scholar]
- 26.Mondlane G, Gubanski M, Lind PA, Ureba A, Siegbahn A. Comparison of gastric-cancer radiotherapy performed with volumetric modulated arc therapy or single-field uniform-dose proton therapy. Acta Oncol. 2017;56:832–838. doi: 10.1080/0284186X.2017.1297536. [DOI] [PubMed] [Google Scholar]
- 27.Alber M, Reemtsen R. Intensity modulated radiotherapy treatment planning by use of a barrier-penalty multiplier method. Opt Methods Softw. 2007;22:391–411. doi: 10.1080/10556780600604940. [DOI] [Google Scholar]
- 28.Niemierko A. Reporting and analyzing dose distributions: a concept of equivalent uniform dose. Med Phys. 1997;24:103–110. doi: 10.1118/1.598063. [DOI] [PubMed] [Google Scholar]
- 29.Dawson LA, Kavanagh BD, Paulino AC, et al. Radiation-associated kidney injury. Int J Radiat Oncol Biol Phys. 2010;76:S108–S115. doi: 10.1016/j.ijrobp.2009.02.089. [DOI] [PubMed] [Google Scholar]
- 30.Marks LB, Bentzen SM, Deasy JO, et al. Radiation dose-volume effects in the lung. Int J Radiat Oncol Biol Phys. 2010;76:S70–S76. doi: 10.1016/j.ijrobp.2009.06.091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Dawson LA, Normolle D, Balter JM, McGinn CJ, Lawrence TS, Ten Haken RK. Analysis of radiation-induced liver disease using the Lyman NTCP model. Int J Radiat Oncol Biol Phys. 2002;53:810–821. doi: 10.1016/S0360-3016(02)02846-8. [DOI] [PubMed] [Google Scholar]
- 32.Ferlay J, Soerjomataram I, Dikshit R, et al. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer. 2015;136:E359–E386. doi: 10.1002/ijc.29210. [DOI] [PubMed] [Google Scholar]
- 33.Wong KK, All S, Waxer J, et al. Radiotherapy after high-dose chemotherapy with autologous hematopoietic cell rescue: quality assessment of head start III. Pediatr Blood Cancer. 2017;64:e26529. doi: 10.1002/pbc.26529. [DOI] [PubMed] [Google Scholar]
- 34.Wieland P, Dobler B, Mai S, et al. IMRT for postoperative treatment of gastric cancer: covering large target volumes in the upper abdomen: a comparison of a step-and-shoot and an arc therapy approach. Int J Radiat Oncol Biol Phys. 2004;59:1236–1244. doi: 10.1016/j.ijrobp.2004.02.051. [DOI] [PubMed] [Google Scholar]
- 35.Lohr F, Dobler B, Mai S, et al. Optimization of dose distributions for adjuvant locoregional radiotherapy of gastric cancer by IMRT. Strahlenther Onkol. 2003;179:557–563. doi: 10.1007/s00066-003-1087-z. [DOI] [PubMed] [Google Scholar]
- 36.Haneder S, Michaely HJ, Schoenberg SO, et al. Assessment of renal function after conformal radiotherapy and intensity-modulated radiotherapy by functional 1H-MRI and 23Na-MRI. Strahlenther Onkol. 2012;188:1146–1154. doi: 10.1007/s00066-012-0254-5. [DOI] [PubMed] [Google Scholar]
- 37.Kachnic LA, Winter K, Myerson RJ, et al. RTOG 0529: a phase 2 evaluation of dose-painted intensity modulated radiation therapy in combination with 5-fluorouracil and mitomycin-C for the reduction of acute morbidity in carcinoma of the anal canal. Int J Radiat Oncol Biol Phys. 2013;86:27–33. doi: 10.1016/j.ijrobp.2012.09.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Eisbruch A, Harris J, Garden AS, et al. Multi-institutional trial of accelerated hypofractionated intensity-modulated radiation therapy for early-stage oropharyngeal cancer (RTOG 00-22) Int J Radiat Oncol Biol Phys. 2010;76:1333–1338. doi: 10.1016/j.ijrobp.2009.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Gondi V, Cui Y, Mehta MP, et al. Real-time pretreatment review limits unacceptable deviations on a cooperative group radiation therapy technique trial: quality assurance results of RTOG 0933. Int J Radiat Oncol Biol Phys. 2015;91:564–570. doi: 10.1016/j.ijrobp.2014.10.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Habraken SM, Sharfo AW, Buijsen J, et al. The TRENDY multi-center randomized trial on hepatocellular carcinoma – trial QA including automated treatment planning and benchmark-case results. Radiother Oncol. 2017;125:507–513. doi: 10.1016/j.radonc.2017.09.007. [DOI] [PubMed] [Google Scholar]
- 41.Hussein M, South CP, Barry MA, et al. Clinical validation and benchmarking of knowledge-based IMRT and VMAT treatment planning in pelvic anatomy. Radiother Oncol. 2016;120:473–479. doi: 10.1016/j.radonc.2016.06.022. [DOI] [PubMed] [Google Scholar]
- 42.Fogliata A, Belosi F, Clivio A, et al. On the pre-clinical validation of a commercial model-based optimization engine: application to volumetric modulated arc therapy for patients with lung or prostate cancer. Radiother Oncol. 2014;113:385–391. doi: 10.1016/j.radonc.2014.11.009. [DOI] [PubMed] [Google Scholar]
- 43.Fogliata A, Nicolini G, Clivio A, et al. A broad scope knowledge based model for optimization of VMAT in esophageal cancer: validation and assessment of plan quality among different treatment centers. Radiat Oncol. 2015;10:220. doi: 10.1186/s13014-015-0530-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Clinical details of patients with gastric carcinoma. (DOCX 15 kb)
Data Availability Statement
The dataset generated and analyzed during the current study are available from the corresponding author on reasonable request.


