Abstract
Background
Only a small percentage of dialysis patients receive a transplant and this is particularly the case for racial/ethnic minorities. Our objective was to identify barriers to initial transplant evaluation in our dialysis centers.
Methods
We conducted a survey of adult hemodialysis patients from 4 dialysis units in the Denver Metro area in 2016. Participants completed an 11-item survey with demographic information and questions regarding time on dialysis, if a provider ever spoke to them about transplant and whether they had been evaluated for a transplant. Reasons for not having an evaluation were explored. Descriptive statistics, chi-square analyses and multivariate analyses were used to examine the responses.
Results
167 patients completed the survey (response rate 63.9%). The majority of participants were male and were Hispanic (49%) or Non-Hispanic Black (31.7%). 140 patients (84.0%) reported discussing kidney transplantation with their doctor but only 53% reported having a transplant evaluation. After adjustment for age, gender and time on dialysis, significantly fewer Blacks reported having an evaluation than Non-Hispanic whites or Hispanics (43.4% vs. 57.7% (Whites) and 59.7% (Hispanics)) p=0.03. The most frequent responses of the patients who had not been evaluated were: not referred by their provider (46%), did not know how to proceed (43.4%) or did not understand the benefits (39.5%) or transplant process (38.2%). Compared to Non-Hispanic whites, Blacks and Hispanics reported less understanding of the benefits and process of transplant.
Conclusion
Timely referral by providers and improved kidney transplantation education may reduce disparities in access to kidney transplantation.
Keywords: racial disparities, kidney transplant, hemodialysis
Introduction
Patients with end stage renal disease (ESRD) on dialysis have high morbidity and mortality. In the United States, patients on dialysis have a mortality rate that exceeds 20% during the first year on dialysis and 50% after 5 years [1]. Kidney transplantation offers a survival advantage compared to chronic dialysis [2–4]. Following kidney transplantation, most patients receive a doubling of their life expectancy. Kidney transplantation is also associated with an improvement in quality of life, physical functioning and psychosocial functioning [2]. However, only a minority of patients with ESRD receive a kidney transplant. In 2012, only 13% of incident ESRD patients were added to the waiting list or received a transplant within one year of ESRD initiation.1 African American patients are less than half as likely to undergo transplantation compared to whites despite having four times the prevalence of ESRD [5]. Hispanics also have a disproportionally higher prevalence of ESRD compared to non-Hispanic whites but are less likely to receive a transplant [1]. To receive a transplant, patients must first be referred and then complete the evaluation process. Increased time on dialysis has been shown to have a negative effect on transplant allograft survival [6], so prompt referral and placement on the waitlist is essential. Racial/ethnic minorities are not referred to transplant at the same rate as white patients and take significantly longer to complete this process [5,7,8]. The reasons for these disparities are unclear but exist even after controlling for clinical factors such as comorbidities. While there has been more research done in the African American population, there is a paucity of data regarding the reasons for inequities in transplant referrals in the Hispanic population. The purpose of this study was to identify barriers to kidney transplant evaluation in dialysis patients in the Denver metro area in order to design appropriate interventions to overcome these barriers. We conducted a survey of patients with ESRD on hemodialysis to gather data regarding their knowledge, attitudes, beliefs and barriers to kidney transplantation. We hypothesized that patients from different racial/ethnic groups would have different barriers to kidney transplantation.
Methods
Adult patients on hemodialysis from four dialysis units in the Denver Metro Area staffed by providers from the University of Colorado were invited to complete an 11-item survey. We included both incident and prevalent hemodialysis patients. Incident patients were defined as being on hemodialysis ≤ 1 year. Participants were recruited by a medical student and study coordinator and completed the survey while they were on dialysis. If participants were unable to read the survey, the student or coordinator read the survey to the patient. The survey took approximately 10-15 minutes to complete. The survey was approved by the Colorado Institutional Review Board and the patients provided implied consent through their voluntary return of the survey. Responses to the survey were anonymous. Data collection occurred from June through September 2016. The survey was conducted in both English and Spanish.
The survey was modeled after an instrument previously developed by investigators to explore issues of barriers to initial kidney transplantation evaluation in South Carolina [9]. The original survey was developed by an expert panel of six clinicians and researchers and was pilot-tested using key-informant interviews to ensure the questions were appropriately understood and the categorical responses were inclusive of all possibilities. We modified the survey instrument slightly for our study in order to assess whether healthcare providers were discussing transplantation with patients, whether patients had undergone an initial evaluation for a kidney transplant and whether patients were on the transplant waiting list. The additional categorical responses we added were based on interviews of the dialysis providers at the 4 dialysis units. If patients had not been evaluated for a transplant by the transplant team they were asked why and were provided a list of choices including the following: ‘Not referred by my doctor;’ Didn’t think I would pass all medical tests;’ ‘Didn’t fit my schedule;’ ‘Difficulty making an appointment at the transplant center;’ ‘Did not have transportation or money to get to the transplant center for the evaluation;’ ‘Dialysis isn’t that bad;’ ‘Scared of getting a transplant;’ ‘Cannot afford the transplant and/or meds;’ ‘Don’t understand the transplant process;’ ‘Don’t understand the benefits of transplant;’ ‘Wasn’t sure how to proceed;’ ‘Didn’t believe anyone would serve as a living donor for me;’ Worried about how long the wait for a kidney would be;’ and an open ‘Other’ category. Participants were encouraged to circle all reasons that applied to them. If patients had been evaluated for transplant but were not on the transplant waitlist they were asked why and were provided a list of choices including the following: ‘Never completed the tests required for transplant;’ ‘Still in the process of completing the tests required;’ ‘Was no longer interested in transplant;’ ‘Was told I was not a candidate for kidney transplant;’ ‘Never heard back from the transplant center;’ ‘Worried about how long the wait for a kidney would be;’ ‘Scared of getting a transplant;’ ‘Cannot afford the transplant and/or medications;’ ‘Don’t understand the transplant process;’ ‘Don’t understand the benefits of transplant;’ and an open “Other” category. Participants were encouraged to circle all reasons that applied to them.
We also collected patient age, race/ethnicity, years on dialysis and primary language. Descriptive statistics were used to provide summaries of the responses. The responses were summarized in the entire population and then by race/ethnicity. Chi-square tests were used to compare the responses among races/ethnicities. Multivariate regression was used to examine differences across races/ethnicities. The covariates included in the fully adjusted model include age, gender and time on dialysis. Statistical significance for all analyses was set at p<0.05. All analyses were performed using SAS 9.4 (SAS Institute, Cary, NC, USA).
Results
A total of 261 hemodialysis patients were eligible for the study and responses were received from 167 patients for a response rate of 63.9%. Those who did not complete the survey either declined to participate or did not show up for their dialysis treatment. Characteristics of the participants are shown in Table 1. The majority of participants were male between the ages of 50-79 years and were Hispanic (49%) or Non-Hispanic Black (31.7%). Only 15.6% were Non-Hispanic white. Almost 20% of patients had been on dialysis for one year or less whereas 29.3% had been on dialysis for more than 6 years.
Table 1.
Characteristics of Hemodialysis Study Participants
| Characteristic | N(%) |
|---|---|
| Age (years) | |
| < 30 | 4 (2.4) |
| 30-39 | 3 (1.8) |
| 40-49 | 23 (13.8) |
| 50-59 | 45 (26.9) |
| 60-69 | 48 (28.7) |
| 70-79 | 35 (21.0) |
| > 80 | 9 (5.4) |
| Gender | |
| Male | 62 (37.1) |
| Female | 105 (62.9) |
| Race/Ethnicity | |
| Non-Hispanic White | 26 (15.6) |
| Non-Hispanic Black | 53 (31.7) |
| Hispanic | 77 (46.1) |
| Other | 11 (6.6) |
| Primary Language | |
| English | 119 (71.3) |
| Spanish | 44 (26.3) |
| Dialysis Vintage | |
| ≤ 1 year | 33 (19.8) |
| 2 years | 38 (22.8) |
| 3 years | 19 (11.4) |
| 4 years | 12 (17.2) |
| 5 years | 15 (9.0) |
| > 6 years | 49 (29.3) |
The majority of participants (n=140, 84.0%) reported that a doctor had talked to them about kidney transplantation (Figure 1). Twenty-five patients (15.0%) responded that a doctor had not discussed transplant with them or were unsure if they had and two did not respond to the question. Over 90% of Non-Hispanic whites, 83% of Non-Hispanic Blacks and 84.4% of Hispanics reported a discussion regarding transplant with their doctor (Figure 1).
Figure 1.
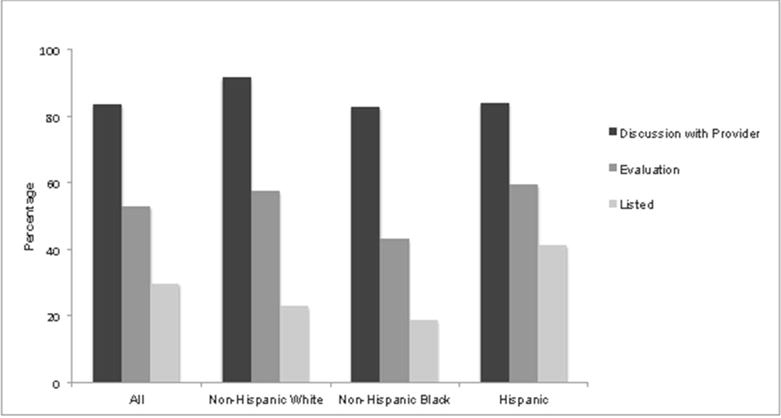
Percentage of Participants Self-Reporting ever having a Transplant Discussion, Initial Transplant Evaluation and/or ever Being Listed for a Transplant
Only 53.2% (n=89) of all participants had an initial transplant evaluation (Figure 1). Fewer Non-Hispanic Blacks reported having a transplant evaluation than Non-Hispanic whites or Hispanics (43.4% vs. 57.7% (Whites) and 59.7% (Hispanics)), which trended towards statistical significance in univariate analysis, p=0.07. After adjustment for age, gender and years on dialysis, Blacks were significantly less likely than Whites and Hispanics to have had a transplant evaluation, p=0.03). When asked why they had not been evaluated for transplant, the majority responded they had not been referred for an evaluation by the transplant team by their primary nephrology provider (46%), did not know how to proceed (43.4%) or did not understand the benefits (39.5%) or transplant process (38.2%). Reasons for not having a transplant evaluation by race/ethnicity are shown in Figure 2. Compared to Non-Hispanic Whites, Blacks and Hispanics reported less understanding of the benefits (p=0.03) and process of transplant (p=0.08). After adjustment for age, gender and years on dialysis Blacks and Hispanics were still less likely to understand the benefits (p=0.03 for Blacks and p=0.04 for Hispanics) and process (p=0.02 for Blacks and p=0.03) of transplant. Additionally, more Blacks reported not being referred by their provider as a reason for not receiving a transplant evaluation than whites (55.2% vs. 36.3%) but it did not reach statistical significance in unadjusted or adjusted models (p=0.12 for both).
Figure 2.
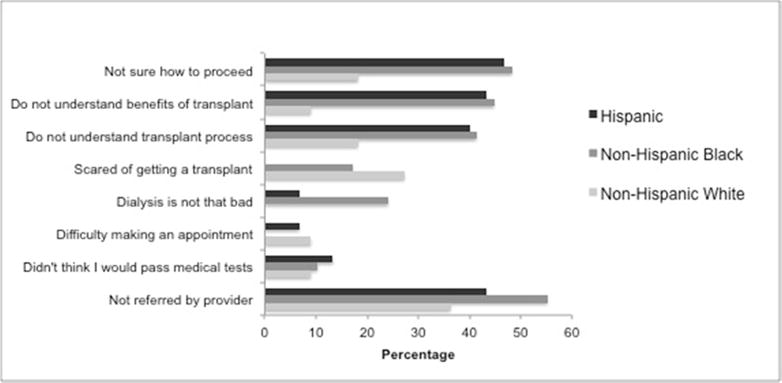
Self-Reported Reasons for not having an Initial Transplant Evaluation by Race/Ethnicity
There were 48 patients (28.7%) whose primary language was not English. Of these patients, 62.5% had a transplant evaluation. Of those who had not been evaluated (N=17), the majority reported they had not been referred (64.7%), did not know how to proceed (64.7%) or did not understand the benefits (58.9%) or transplant process (52.9%).
Of the patients that had a transplant evaluation, 56% were on the transplant waitlist. In unadjusted analysis, Hispanics were significantly more likely to be listed for transplant than Non-Hispanic whites or blacks (p=0.03), but in the fully adjusted model this association no longer remained significant (p=0.09). There were 36 patients that had completed a transplant evaluation but were not on the waitlist. When asked why they were not listed for transplant the majority reported they were still in the process of completing the tests (41.7%), were told they were not a transplant candidate (25.0%) or were no longer interested in transplant after the evaluation (22.2%), Figure 3. Only one patient responded they were not listed due to not understanding the transplant process and only two stated it was due to not understanding the benefits of transplant. Reasons for not being on the waiting list did not differ by race/ethnicity.
Figure 3.
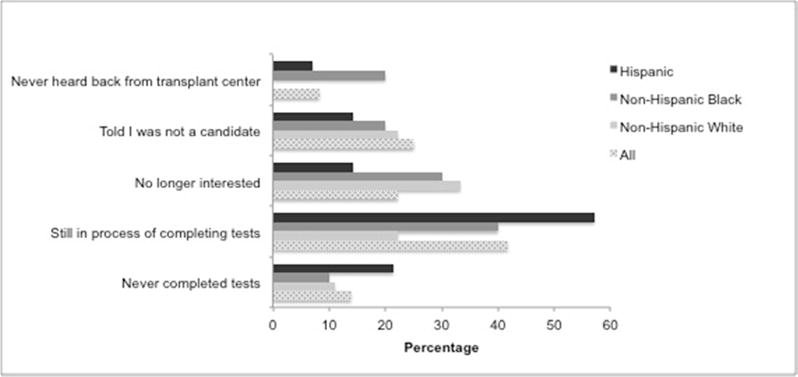
Self-Reported Reasons for not ever being Listed on Transplant Waitlist
DISCUSSION
We found that while most patients had discussed kidney transplantation with their doctor only half reported having an evaluation for transplant. The most commonly cited reasons for not having had an evaluation were not being referred by their primary nephrology provider, not knowing how to proceed or not understanding the benefits of transplant or the transplant process. Furthermore, we found that compared to Non-Hispanic whites and Hispanics, fewer Non-Hispanic blacks had been evaluated for transplant.
Racial/ethnic disparities in access to kidney transplantation have been well described and it is clear that the disparity arises long before the actual day of transplantation. There are multiple steps in the pathway to kidney transplantation, which starts with education about transplantation and referral to a transplant center. Navigating the process from education to completing an evaluation and being listed on the waitlist can be overwhelming. Patients may have no desire to proceed based on preconceptions about the need to meet certain medical, psychological, social, and financial criteria. Thus, lack of patient knowledge regarding transplantation may be a key reason for disparities in transplant evaluations. Compared to whites, African Americans are less likely to be referred for and complete a transplant evaluation [5,7,8]. Hispanics are also less likely to be referred and face barriers in some but not all stages in the evaluation process [10]. Studies have shown that African Americans express more confidence regarding their prognosis on dialysis and report a significant fear of dying following a kidney transplant [11]. This is concerning given that transplant is associated with a better prognosis. On average, African Americans presenting for transplant knew only 21% of basic transplant knowledge questions compared with whites that knew 50% [12]. Average health literacy rates among Hispanics in the general population are reportedly lower than rates among whites [13]. In our study, the two most commonly cited reasons by African Americans and Hispanics for not having a transplant evaluation were that they did not understand the benefits of transplant or transplant process, both of which are modifiable with education. Studies have found that once African American and Hispanic patients’ transplant knowledge is improved there is an increased willingness to pursue transplantation [14–16]. Hence, patient education is a critical step in increasing access to transplantation. In our study, we did not find any difference in initial transplant evaluations between Hispanics and non-Hispanic whites. In a study by Hall et al [17] they also found no difference in access to transplantation between Hispanics and whites, but did find that time to transplantation among those waitlisted was longer in Hispanics. We did not evaluate time to transplantation in our study. Thus, the disparity in access to the waitlist among Hispanics appears to be decreasing but interventions are still needed to reduce time to transplantation after waitlisting.
African Americans are less likely to be referred for transplant even when they are considered appropriate candidates whereas whites are more likely to be referred even when they are considered inappropriate candidates [18]. Lack of knowledge by providers regarding the benefits of transplantation in ethnic minorities likely leads to lower referral rates. In one study, nearly a third of physicians were less likely to believe that transplantation prolongs survival compared to dialysis in African Americans [19]. Thus, providers may carry an inherent bias and not make potentially qualified patients aware of their option for transplantation. In our study, more blacks reported not being referred to transplant by their provider than whites. The difference did not reach statistical significance, which may be due to our small sample size. The reason for the lower rate of referral is not clear but may be due to lack of provider knowledge and poor patient-provider communication. In a study of dialysis providers from 254 dialysis centers, only 41% of providers felt knowledgeable to answer patients’ questions regarding transplantation [20]. Furthermore, African Americans report less communication regarding information about transplantation from their physicians [21, 22]. Studies have found that poor patient-provider communication and family-provider communication contributes to the lower level of knowledge regarding the benefits of kidney transplantation in African Americans [23].
Hispanics also have lower referral rates for transplantation than whites, primarily in preemptive (prior to starting dialysis) evaluations [24]. In our population, there was no difference in the rate of referral between Hispanics and whites. However, we did not explore how many of the patients had received an evaluation prior to starting dialysis and this needs to be examined in future studies. Additionally, studies have found that non-English speakers are less likely to be evaluated and listed for transplant [25]. In our study, 28.7% of the Hispanics were non-English speaking. Of those 48 patients, we found that 63% had been evaluated for transplant and there was no difference in the rate of referral compared with English speakers. The difference in our findings with others may be due to the fact that we have a large Hispanic population in our dialysis units and have Spanish speaking transplant coordinators to assist with the evaluation process.
Our study has some limitations. First, we only examined responses from patients in the Denver Metro area and our findings may not be relevant to other programs. Second, since the results rely on the patients self-report of their own care, recall bias may be an issue. Third, since the survey was anonymous we could not perform a review of the medical record to confirm whether or not a patient had been evaluated or listed for transplant. Fourth, we did not collect information on socioeconomic status, education or comorbidities, which are all important confounders in assessing barriers to transplantation. Fifth, we did not use ranked reasons for not having a transplant evaluation. This may have been a better approach to see which barriers held the greatest weight in contribution to not having an evaluation. Additionally, we only included prevalent dialysis patients and findings may be different in incident dialysis patients. We did not collect data on the time from evaluation to being placed on the waiting list so were unable to determine if there were differences by race/ethnicity. Finally, with the small sample size and design of our study we were unable to determine the reliability of our additional question to the original survey. Our study also has several strengths including that we were able to examine perceived barriers to transplantation in our dialysis population. Additionally, we had a large Hispanic and Spanish as a primary language population and thus the data can be used to target interventions for these specific groups.
The barriers to kidney transplant evaluation identified in our study are modifiable and can be overcome through quality improvement interventions targeting patients, providers and facilities. Providing universal comprehensive education to patients and providers may significantly improve access to transplantation. Patients unaware of the health incentives could receive tailored decision aids to develop their understanding. Many providers do not know the benefits of transplant in minority patients and are not comfortable providing transplant education [20]. Improving provider knowledge and counseling skills may improve provider driven patient education. With limited time by physicians to discuss transplant options with an individual patient, other providers in the practice, including members of the multidisciplinary CKD team such as a trained nurse, advanced practitioner, or social worker, can perform discussions and education. Additionally, providing physicians and clinics with performance statistics of transplant referrals may help identify disparities in referral rates. Providers with low referral rates could be made aware by receiving provider-specific feedback and be required to attend additional education sessions. In fact, a recent pragmatic trial performed in 134 dialysis facilities in George found that dialysis units that received an intervention consisting of transplant education and engagement of facilities, providers, staff and patients referred a higher proportion of the patients for transplant after one year [26]. Thus, dialysis units should consider a multidimensional approach targeting patient, provider and facility level factors to overcome racial/ethnic disparities in access to kidney transplantation.
Acknowledgments
Support: This work was supported by the National Institute of Diabetes and Digestive and Kidney Disease (NIDDK) grant K23 DK087859 (Kendrick) and the National Heart, Blood and Lung Institute grant R56 HL132868 (Kendrick).
Footnotes
Conflict of Interest: Authors have nothing to disclose
Financial Disclosures: Authors have nothing to disclose.
References
- 1.United States Renal Data System, USRDS 2012 annual data report. Atlas of chronic kidney disease and end-stage renal disease in the United States. National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases; Bethesda, MD: 2012. [Google Scholar]
- 2.Evans RW, Manninen DL, Garrison LP, Jr, Hart LG, Blagg CR, Gutman RA, Hull AR, Lowrie EG. The quality of life of patients with end-stage renal disease. N Engl J Med. 1985;12:553–559. doi: 10.1056/NEJM198502283120905. [DOI] [PubMed] [Google Scholar]
- 3.Hunsicker LG. A survival advantage for renal transplantation. N Engl J Med. 1999;341:1762–1763. doi: 10.1056/NEJM199912023412310. [DOI] [PubMed] [Google Scholar]
- 4.Port FK, Wolfe RA, Mauger EA, Berling DP, Jiang K. Comparison of survival probabilities for dialysis patients vs cadaveric renal transplant patients. JAMA. 1993;270:1339–1343. [PubMed] [Google Scholar]
- 5.Myaskovsky L, Almario Doebler D, Posluszny DM, Dew MA, Unruh M, Fried LF, Switzer GE, Kim S, Chang CC, Ramkumar M, Shapiro R. Perceived discrimination predicts longer time to be accepted for kidney transplant. Transplantation. 2012;93:423–429. doi: 10.1097/TP.0b013e318241d0cd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Meier-Kriesche HU, Port FK, Ojo AO, Rudich SM, Hanson JA, Cibrik Dm, Leichtman AB, Kaplan B. Effect of waiting time on renal transplant outcome. Kidney Int. 2000;58:1311–1317. doi: 10.1046/j.1523-1755.2000.00287.x. [DOI] [PubMed] [Google Scholar]
- 7.Ayanian JZ, Cleary PD, Weissman JS, Epstein AM. The effect of patients’ preferences on racial differences in access to renal transplantation. N Engl J Med. 1999;341:1661–1669. doi: 10.1056/NEJM199911253412206. [DOI] [PubMed] [Google Scholar]
- 8.Waterman AD, Rodrigue JR, Purnell TS, Ladin K, Boulware LE. Addressing racial and ethnic disparities in live donor kidney transplantation: priorities for research and intervention. Semin Nephrol. 2010;30:90–98. doi: 10.1016/j.semnephrol.2009.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kazley AS, Simpson KN, Chavin KD, Baliga P. Barriers facing patients referred for kidney transplant cause loss to follow-up. Kidney Int. 2012;82:1018–1023. doi: 10.1038/ki.2012.255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sequist TD, Narva AS, Stiles SK, et al. Access to renal transplantation among American Indians and Hispanics. Am J Kidney Dis. 2004;44:344–352. doi: 10.1053/j.ajkd.2004.04.039. [DOI] [PubMed] [Google Scholar]
- 11.Wachterman MW, McCarthy EP, Marcantonio ER, Ersek M. Mistrust, misperceptions, and miscommunication: a qualitative study of preferences about kidney transplantation among African Americans. Transplant Proc. 2015;47:240–246. doi: 10.1016/j.transproceed.2015.01.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Waterman AD, Peipert JD, Hyland SS, McCabe MS, Schenk EA, Liu J. Modifiable patient characteristics and racial disparities in evaluation completion and living donor transplant. Clin J Am Soc Nephrol. 2013;8:995–1002. doi: 10.2215/CJN.08880812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Purnell TS, Hall YN, Boulware LE. Understanding and overcoming barriers to living kidney donation among racial and ethnic minorities in the United States. Adv Chronic Kidney Dis. 2012 Jul;19(4):244–51. doi: 10.1053/j.ackd.2012.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Patzer RE, Perryman JP, Pastan S, Amaral S, Gazmararian JA, Klein M, Kutner N, McClellan WM. Impact of a patient education program on disparities in kidney transplant evaluation. Clin J Am Soc Nephrol. 2012;7:648–655. doi: 10.2215/CJN.10071011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gordon EJ, Reddy E, Gil S, et al. Culturally competent transplant program improves Hispanics’ knowledge and attitudes about live kidney donation and transplant. Prog Transplant. 2014;24:56–68. doi: 10.7182/pit2014378. [DOI] [PubMed] [Google Scholar]
- 16.Rodrigue JR, Cornell DL, Kaplan B, Howard RJ. A randomized trial of a home-based educational approach to increase live donor kidney transplantation: effects in blacks and whites. Am J Kidney Dis. 2008;51:663–670. doi: 10.1053/j.ajkd.2007.11.027. [DOI] [PubMed] [Google Scholar]
- 17.Hall YN, Choi AI, Xu P, O’Hare AM, Chertow GM. Racial ethnic differences in rates and determinants of deceased donor kidney transplantation. J Am Soc Nephrol. 2011;22:743–751. doi: 10.1681/ASN.2010080819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Epstein AM, Ayanian JZ, Keogh JH, Noonan SJ, Armistead N, Cleary PD, Weissman JS, David-Kasdan JA, Carlson D, Fuller J, Marsh D, Conti RM. Racial disparities in access to renal transplantation–clinically appropriate or due to underuse or overuse? N Engl J Med. 2000;343:1537–1544. doi: 10.1056/NEJM200011233432106. 1532 p preceding 1537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ayanian JZ, Cleary PD, Keogh JH, Noonan SJ, David-Kasdan JA, Epstein AM. Physicians’ beliefs about racial differences in referral for renal transplantation. Am J Kidney Dis. 2004;43:350–357. doi: 10.1053/j.ajkd.2003.10.022. [DOI] [PubMed] [Google Scholar]
- 20.Waterman ADGC, Hyland S. Dialysis providers ability to educate patients about transplant: Good education partners?. American Transplant Conference; Boston, MA. 2009. [Google Scholar]
- 21.Ayanian JZ, Cleary PD, Weissman JS, Epstein AM. The effect of patients’ preferences on racial differences in access to renal transplantation. N Engl J Med. 1999;341:1661–1669. doi: 10.1056/NEJM199911253412206. [DOI] [PubMed] [Google Scholar]
- 22.Ayanian JZ, Cleary PD, Keogh JH, Noonan SJ, David-Kasdan JA, Epstein AM. Physicians’ beliefs about racial differences in referral for renal transplantation. Am J Kidney Dis. 2004;43:350–357. doi: 10.1053/j.ajkd.2003.10.022. [DOI] [PubMed] [Google Scholar]
- 23.Traino HM, West SM, Nonterah CW, Russell J, Yuen E. Communicating About Choices in Transplantation (COACH): Results of a Pilot Test Using Matched Controls. Prog Transplant. 2017;27:31–38. doi: 10.1177/1526924816679844. [DOI] [PubMed] [Google Scholar]
- 24.Joshi S, Gaynor JJ, Bayers S, Guerra G, Eldefrawy A, Chediak Z, Companioni L, Sageshima J, Chen L, Kupin W, Roth D, Mattiazzi A, Burke GW, 3rd, Ciancio G. Disparities among Blacks, Hispanic and Whites in time from starting dialysis to kidney transplant waitlisting. Transplantation. 2013;95:308–318. doi: 10.1097/TP.0b013e31827191d4. [DOI] [PubMed] [Google Scholar]
- 25.Talamantes E, Norris KC, Mangione CM, Moreno G, Waterman AD, Peipert JD, Bunnapradist S, Huang E. Linguistic isolation and access to the active kidney transplant waiting list in the United States. 2017;12:483–492. doi: 10.2215/CJN.07150716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Patzer RE, Paul S, Plantinga L, Gander J, Sauls L, Krisher J, Mulloy LL, Gibney EM, Browne T, Zayas CF, McClellan WM, Arriola KJ, Pastan SO, Southeastern Kidney Transplant Coalition J Am Soc Nephrol. 2017;28:935–942. doi: 10.1681/ASN.2016030320. [DOI] [PMC free article] [PubMed] [Google Scholar]


