Abstract
Background
Substance use disorders (SUD) are associated with non-adherence to medical care and high utilization of hospital services. This study characterized patterns and correlates of rehospitalization among patients seen by a hospital-based SUD consultation-liaison (CL) team.
Methods
This study was a retrospective medical record review of patients in a large urban academic hospital who received SUD consultation and were diagnosed with opioid, cocaine, and/or alcohol use disorder (N=267). Data were collected on patient characteristics, substance-specific SUD diagnoses (opioids, cocaine, and alcohol), opioid agonist treatment (OAT) with methadone or buprenorphine (treatment status at admission; in-hospital initiation of OAT), and rehospitalization through 180 days post-discharge. Associations with rehospitalization were examined using bivariate tests of independence and multivariate logistic regression, with patient background and medical characteristics, substance-specific SUD diagnoses, and OAT status (at admission and in-hospital initiation) as predictors.
Results
Rehospitalization rates were higher among patients with current opioid (38% vs. 24%; p<.05) and cocaine use disorders (39% vs. 26%; p<.05) compared to patients without these diagnoses. In multivariate logistic regression analysis, the number of medical comorbidities [Adjusted Odds Ratio (AOR)=1.2; p<.01] and opioid use disorder (AOR=2.4, p<.05) were independently associated with rehospitalization.
Conclusions
In this sample of hospital patients receiving SUD CL services, the risk of rehospitalization differed by type of SUD diagnosis. In-hospital initiation of OAT is promising for facilitating treatment linkage post-discharge, but this small study did not show differences in rehospitalization based on OAT initiation. These findings could inform services for hospital patients with comorbid SUDs.
Keywords: Hospital, Addiction, Consultation Liaison, Readmission, Treatment Linkage, Opioid Use Disorder
1. Introduction
Substance use disorders (SUD) are associated with non-adherence to medical care and overutilization of hospital and emergency department services (Fuller et al., 2013; Mark et al., 2013; McGeary and French, 2000; Raven et al., 2009; Raven et al., 2010; Schrag et al., 2006; Walley et al., 2012). A number of these hospitalizations result from medical problems caused or exacerbated by substance use problems (Weintraub et al., 2001). Frequent causes of hospitalizations can be directly attributed to substance use, such as overdose, soft tissue infections, endocarditis, and intoxication-related injury or trauma (Weintraub et al., 2001; Macdonald et al., 2003; Takahashi et al., 2003). Following trends in opioid use over the last decade, research has found a dramatic increase in nationwide hospitalizations related to serious infections and endocarditis among those with intravenous drug use (Ronan et al., 2016; Wurcel et al., 2016). SUDs can also contribute to poor prognosis due to prioritization of substance use over self-care and routine healthcare. Patients with SUDs are less likely to adhere to recommended discharge plans and medical treatment (Tawk et al., 2013; Gonzalez et al., 2011). As comorbidity, SUDs elevate the risk of hospital readmission for other medical problems, including heart failure and pneumonia (Ahmenadi et al., 2015). Research shows that approximately 25% of rapid rehospitalizations could be considered avoidable (van Walraven et al., 2011; van Walraven et al., 2012). Due to high risk of poor adherence to medical follow-up care, effects of acute intoxication that could lead to injuries or overdose, and other factors, individuals with SUDs could contribute to a large percentage of preventable rehospitalizations.
Given the over-utilization of hospital services through repeat hospitalizations, the minimization of healthcare costs has become a focal issue in public health and a crucial performance metric for hospitals (Joynt and Jha, 2013; Mittler et al., 2013). A recent study found that there were approximately 3.3 million readmissions within 30-days from original discharge in the US across all payers; over half of those readmissions were Medicare patients who accounted for 58.2% of the total annual cost of $41.3 billion (Hines et al., 2014). As a result, Medicare has begun imposing reimbursement penalties on hospitals with high 30-day readmission rates for a select number of diseases to incentivize hospitals to improve the continuum of care and ensure a smooth transition from hospital to community outpatient services (Joynt and Jha, 2013). Given the need to drive down healthcare costs and hospital service utilization, research has begun to examine post-discharge planning among populations with high levels of hospital service utilization, including patients with SUDs and related problems. Research has found that SUDs often go undetected among inpatient populations, and hospital-initiated interventions for SUDs are underutilized (Rosenthal et al., 2016; Smothers et al., 2004). There is evidence that interventions to address SUDs among hospital patients can prompt engagement in SUD treatment, and reduce high-cost healthcare utilization (Wei et al., 2015). Likewise, research has found that integrating SUD and medical care in a specialty acute-care day hospital can facilitate SUD treatment entry and utilization of ambulatory medical care (O’Toole et al., 2002; 2006).
In recognition of the important role that SUDs can play in patient health and medical prognosis, some hospitals have formed specialized SUD consultation-liaison (CL) services. Such CL services can provide specialist recommendations to the care team regarding withdrawal symptom management, initiation of SUD treatment in the hospital, and referrals to treatment, among other services (Aszalos et al., 1999; Fuller and Jordan, 1994; McDuff et al., 1997; Murphy et al., 2009; Trowbridge et al., 2017; Wakeman et al., 2017)
The present study was a retrospective review of electronic medical record information for patients seen by the CL service. This study sought to investigate four specific questions regarding this population. The aims of the study were to: (1) describe the services provided by the hospital SUD CL service; (2) characterize the patient population receiving SUD consultation; (3) examine rehospitalization based on (a) specific SUD diagnoses, (b) enrollment in opioid use disorder pharmacotherapy with methadone or buprenorphine at the time of admission, and (c) initiation of such treatment in the hospital; and (4) examine linkage to SUD treatment post-discharge, as available.
2. Methods
2.1. Program Description
The University of Maryland Medical Center (UMMC) is a largely urban, tertiary care academic hospital with 750 beds, over 29,800 annual admissions, a level 1 Trauma Center with over 8,600 annual admissions, and over 61,400 observation and emergency department visits. It has a long-standing SUD CL service that has been in continuous operation for more than 3 decades (McDuff et al., 1997). This service sees patients from a variety of hospital units (e.g., internal medicine, surgery, trauma, labor, and delivery), and is called in whenever the medical/surgical team suspects that a patient may have a substance use problem. The CL service is comprised of an interdisciplinary team, including a psychiatrist director, two part-time addiction-boarded psychiatrists, a licensed addiction counselor, licensed social worker, two nurses, as well as medical and psychiatric residents and addiction medicine fellows. The patient’s treating physicians typically consult the CL service for their patients whose history, physical, or laboratory tests indicate potential alcohol or drug problem. The CL team conducts assessments, provides motivationally-focused bedside counseling, and makes recommendations to the medical team regarding alcohol or opioid intoxication and withdrawal management, and initiation of methadone or buprenorphine maintenance treatment. Additionally, the CL staff regularly makes referrals for follow-up care with various community-based SUD treatment providers upon discharge from the hospital. The team is well-established and widely utilized in the hospital, servicing a high volume of high-risk patients (approximately 2,000 annually).
2.2. Data Collection
This study was a retrospective review of medical records for patients who received services from the UMMC SUD CL service. The purpose of the study was to characterize the patient population and services delivered by the CL team, in preparation for a clinical trial to reduce hospital readmissions for patients with comorbid SUDs. To properly characterize the target population of the future study, inclusion criteria for record extraction were: (a) primary residence in Baltimore City; and (b) discharged from the hospital alive.
The CL team provided research staff with a complete list of patients for whom consultations had been conducted during a pre-specified four-month period (September 2012 through December 2012). Research staff used this patient list to cross-check hospital medical records, retrospectively by date, sequentially. Data were abstracted from electronic medical records across several systems, including the hospital electronic medical record, SUD CL service electronic and hardcopy chart records, and admissions records to two hospital-affiliated programs that provided opioid agonist treatment (OAT). These programs included a methadone treatment program and an outpatient drug treatment program that offered buprenorphine. Data were compiled into a password-protected spreadsheet, and de-identified following record cross-check and linkage. Data were recorded only for patients who met the inclusion criteria defined above. In cases of multiple admissions and addictions consultations during the four-month period, the first admission record was treated as the index admission.
There were 659 hospital admissions in the period of interest that received a SUD consultation, of which 328 (49.8%) lived in Baltimore City. Of these, 29 cases were repeated consultations during readmission, leaving 299 index cases of Baltimore City residents who received addictions consultation services during hospitalization. We subsequently excluded 32 patients from this analysis who did not have a current diagnosis of alcohol, opioid, or cocaine use disorder (DSM-IV abuse or dependence), leaving N=267 for this analysis. For each case, hospital readmission dates were recorded for 180 days after initial discharge.
The data collected from the electronic medical records included: patient characteristics (age, race, gender), reason for hospital admission, admission and discharge dates, type of substance used and substance use diagnoses (DSM-IV abuse or dependence) for alcohol, opioids, and cocaine, prior treatment history, injection drug use status (past year), medical history related to substance use, withdrawal management (including initiation of OAT with methadone or buprenorphine), referrals to SUD treatment, and follow-up care received (if applicable). SUD treatment admission records were limited to programs affiliated with the University Hospital, which included an outpatient SUD treatment program (which offered buprenorphine treatment as well as various psychosocial counseling services) and a methadone treatment program. SUD treatment entry data were recorded if the patient attended their scheduled intake appointment; however, no information was available regarding treatment retention beyond this initial appointment. Hospital readmission data were limited to recorded encounters at the University of Maryland Medical Center. Data were analyzed to examine demographic characteristics of patients seen by the CL team, as well as the prevalence of opioid, cocaine, and alcohol use disorders, rates of hospital readmission (within 30-, 60-, 90- and 180-days), and SUD treatment intake appointments kept, as available. This retrospective record review was approved by the Friends Research Institute and University of Maryland School of Medicine’s Institutional Review Boards.
2.3. Statistical Analysis
Descriptive statistics were used to examine the types of services delivered by the CL team (Aim 1) and the characteristics of the patient population (Aim 2). Bivariate associations of patient characteristics with rehospitalization (Aim 3) were examined using χ2 tests of independence. In addition, a multivariate logistic regression model examined rehospitalization within 180 days, using predictors of patient gender, race, and age, type of SUD diagnosis (opioid, cocaine, alcohol), injection drug use, index hospitalization for one of the Medicare-defined targets for readmission reduction (pneumonia, congestive heart failure, acute myocardial infarction, total hip/knee arthroplasty, and chronic obstructive pulmonary disease), number of medical comorbidities listed in the medical history, and OAT with buprenorphine or methadone (enrollment at time of admission, and initiation of such treatment in the hospital). The medication treatment variables can be estimated with the full sample because the model accounts for the prerequisite condition of opioid use disorder diagnosis (Dziak and Henry, 2017). Medication treatment variables were also examined in analyses restricted to the subgroup of patients with current opioid use disorder, yielding similar results. In addition to examining rehospitalization as a binary event, time-to-first rehospitalization through 180 days was also examined using proportional hazards Cox regression. Descriptive statistics and cross-tabulations with χ2 tests of independence were used to examine the relationship between in-hospital initiation of OAT and SUD treatment entry in the subset of cases for which this information was available (Aim 4).
3. Results
3.1. Services Delivered by the SUD Consultation-liaison
The major services and referral recommendations provided by the CL team are reported in Table 1. In addition to referrals to outpatient treatment programs, the CL frequently delivered brief advice at the bedside (e.g., encouragement to discontinue drug use, education about health risks related to continued drug use). Approximately 22% received brief advice, without another service recorded. Patients who were already in treatment were recommended to return to their treatment programs upon hospital discharge (24%). The most common service recommendation recorded was a referral to a SUD treatment program affiliated with the hospital (30%), while 9% were referred to a non-affiliated program. OAT with buprenorphine or methadone was newly initiated for 14% of the sample. One in ten patients expressed no interest in treatment or refused a formal consultation.
Table 1.
Characteristics of hospitalized city residents with alcohol, opioid, and/or cocaine use disorders seen by the hospital substance use disorder consultation liaison service (N=267).
| N (%) | |
|---|---|
| Patient Characteristics | |
| Age | mean= 48.6 (SD= 11.6) |
| Female | 113 (42.3) |
| African American | 198 (74.2) |
| White | 65 (24.3) |
| Other Race | 4 (1.5) |
| Use drugs by injection | 67 (25.5) |
| Hospital Unit | |
| Internal Medicine | 179 (67.0) |
| Labor & Delivery | 9 (3.4) |
| Shock Trauma/Intensive Care | 54 (20.3) |
| Surgery | 22 (8.2) |
| Other | 3 (1.2) |
| Patient Insurance | |
| Medicare | 47 (17.6) |
| Medicaid | 194 (72.7) |
| Private/Commercial | 15 (5.6) |
| None noted | 11 (4.1) |
| Medical Characteristics | |
| Length of Stay at index hospitalization (days) | mean= 4.9 (SD= 6.4)2 |
| Number of medical comorbidities listed in EHR | mean= 3.2 (SD=2.3)3 |
| Hospitalized for one of the five Medicare-defined target conditions1 | 22 (8.2) |
| SUD Treatment | |
| In opioid agonist treatment at hospital admission | 70 (26.2) |
| Newly started on opioid agonist treatment in hospital | 38 (14.2) |
| SUD Diagnoses (current) | |
| Opioid | 152 (56.9) |
| Cocaine | 114 (42.7) |
| Alcohol | 161 (60.3) |
| Rehospitalization | |
| within 30 days | 37 (13.9) |
| within 60 days | 53 (19.9) |
| within 90 days | 68 (25.5) |
| within 180 days | 84 (31.5) |
| Main Service/Recommendation Recorded | |
| Recommend return to SUD treatment (already enrolled) | 64 (24.0) |
| Brief counseling at bedside | 59 (22.1) |
| Referral to affiliated outpatient treatment program | 79 (29.6) |
| Referral to unaffiliated treatment program | 23 (8.6) |
| Refused consultation/no interest in treatment | 26 (9.7) |
| Other recommendation (e.g., psychiatric) | 3 (1.1) |
| No recommendation recorded | 13 (4.9) |
Note: Substance Use Disorder (SUD) diagnoses for different substances can overlap.
Pneumonia, acute myocardial infarction, chronic obstructive pulmonary disease, heart failure, and total knee or hip anthroplasty.
median= 3 (25th, 75th percentiles= 1, 6).
median= 3 (25th, 75th percentiles= 1, 5).
3.2. Patient Characteristics
Characteristics of the 267 patients in the analysis sample are shown in Table 1. The sample was majority African American (74%), male (58%), with a mean age of 49 years (SD= 12). The majority of patients had Medicaid insurance (73%) and were admitted to the Internal Medicine unit (67%).
3.3. Hospital Readmissions
Hospital readmission rates for the analysis sample of 267 patients were 14% at 30 days, 20% at 60 days, 25% at 90 days, and 31% at 180 days after the index admission. Within 180 days of the index admission, 19% were rehospitalized once, while 12% had multiple hospital readmissions.
Table 2 shows 180-day readmission rates based on substance-specific SUD diagnoses at the time of the index admission. In bivariate analyses, rehospitalization rates were significantly higher among patients with vs. without current diagnoses of opioid use disorder (38% vs. 23%; p=.01) and cocaine use disorder (39% vs. 26%; p=.03), but not alcohol use disorder (30% vs. 34%; p=.48). There were no significant differences in 180-day rehospitalization rates by gender, race, age, or injection drug use status. Likewise, among patients with current opioid use disorder (n= 152), there were no differences in rehospitalization based on current enrollment in methadone or buprenorphine treatment (39% out-of-treatment vs. 36% in treatment), or initiation of such treatment while hospitalized (38% treatment not initiated vs. 37% treatment initiated).
Table 2.
Rehospitalization within 180 days of index admission by current absence/presence of specific substance use disorder diagnoses (N = 267).
| Rehospitalized within 180 days n (%) |
|
|---|---|
| Opioid Use Disorder (p= .01) | |
| No | 27 (23%) |
| Yes | 57 (38%) |
|
| |
| Cocaine Use Disorder (p= .03) | |
| No | 40 (26%) |
| Yes | 44 (39%) |
|
| |
| Alcohol Use Disorder (p= .48) | |
| No | 36 (34%) |
| Yes | 48 (30%) |
Note: p-values are from bivariate likelihood-ratio χ2 tests. Values represent the number and rate of patients experiencing the outcome of interest (rehospitalization) by substance use disorder status. Substance use disorder diagnoses can overlap.
In the multivariate logistic regression model predicting rehospitalization within 180 days of the index admission (Table 3), significant predictors of rehospitalization included opioid use disorder diagnosis [Adjusted Odds Ratio (AOR) = 2.38; 95% Confidence Interval (95% CI) = 1.01, 5.61; p< .05] and number of medical comorbidities (AOR= 1.20; 95% CI= 1.06, 1.37; p< .01). Neither initiation of methadone or buprenorphine treatment at the hospital, nor enrollment in such treatment at the time of admission, were significantly associated with rehospitalization. To examine the possible interactive effect of different SUDs, we fit models with all two-way interactions between opioid, cocaine, and alcohol use disorder diagnoses. None of these interactions were significant (all ps>.05); thus, these interaction terms were dropped from the model.
Table 3.
Logistic regression model predicting rehospitalization within 180 days (N = 267).
| Odds Ratio | 95% CI | p-value | |
|---|---|---|---|
| Opioid Use Disorder (current) | 2.38 | (1.01, 5.61) | .047 |
| Cocaine Use Disorder (current) | 1.79 | (0.99, 3.20) | .052 |
| Alcohol Use Disorder (current) | 1.28 | (0.66, 2.49) | .49 |
| Female | 1.05 | (0.58, 1.90) | .88 |
| African American | 1.39 | (0.70, 2.74) | .35 |
| Age (years) | 0.99 | (0.96, 1.02) | .49 |
| Injection drug use (past year) | 0.84 | (0.40, 1.77) | .65 |
| Enrolled in methadone or buprenorphine at time of admission | 0.74 | (0.29, 1.53) | .34 |
| Initiated methadone or buprenorphine in the hospital | 0.69 | (0.32, 2.02) | .64 |
| Presenting illness of Medicare target conditions1 | 2.52 | (0.97, 6.55) | .058 |
| Number of medical comorbidities | 1.20 | (1.06, 1.37) | .005 |
Pneumonia, acute myocardial infarction, chronic obstructive pulmonary disease, heart failure, and total knee or hip anthroplasty.
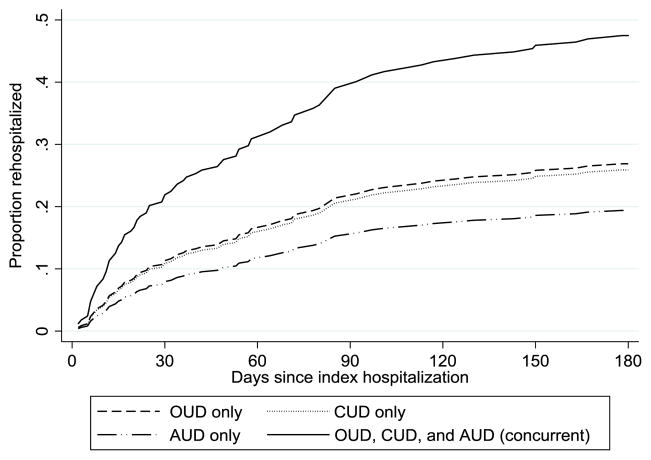
We also examined time-to-first rehospitalization using proportional hazards Cox regression (Table 4), which yielded estimates of similar magnitude but with slightly different findings, with significantly higher rehospitalization risk for patients with cocaine use disorder compared to patients without cocaine use disorder [Hazard Ratio (HR)=1.69; 95% CI= 1.06, 2.70; p= .03]. However, opioid use disorder was non-significant in this model at the .05 level (HR=1.77, 95% CI= 0.92, 3.39; p=.09). Number of comorbidities remained positively associated with rehospitalization (HR=1.15; 95% CI= 1.05, 1.27; p<.01). Figure 1 plots smoothed time-to-rehospitalization curves for substance use disorder diagnosis for opioid, cocaine, and alcohol use disorder alone, and in combination, based on the Cox model.
Table 4.
Cox proportional hazards model predicting rehospitalization within 180 days (N=267).
| Hazard Ratio | 95% CI | p-value | |
|---|---|---|---|
| Opioid Use Disorder (current) | 1.77 | (0.92, 3.39) | .088 |
| Cocaine Use Disorder (current) | 1.69 | (1.06, 2.70) | .028 |
| Alcohol Use Disorder (current) | 1.22 | (0.74, 2.01) | .446 |
| Female | 1.03 | (0.64, 1.65) | .917 |
| African American | 1.25 | (0.72, 2.16) | .433 |
| Age (years) | 0.99 | (0.97, 1.01) | .477 |
| Injection drug use (past year) | 0.96 | (0.55, 1.66) | .881 |
| Enrolled in methadone or buprenorphine at time of admission | 0.86 | (0.46, 1.59) | .621 |
| Initiated methadone or buprenorphine in the hospital | 0.69 | (0.33, 1.44) | .318 |
| Presenting illness of Medicare target conditions1 | 1.91 | (0.98, 3.71) | .056 |
| Number of medical comorbidities | 1.15 | (1.05, 1.27) | .004 |
Pneumonia, acute myocardial infarction, chronic obstructive pulmonary disease, heart failure, and total knee or hip anthroplasty
Figure 1.
Predicted time-to-rehospitalization by substance use disorder diagnoses.
Note: Smoothed curves are derived from the Cox regression model. OUD= Opioid Use Disorder, CUD= Cocaine Use Disorder, AUD= Alcohol Use Disorder.
3.4. SUD Treatment Linkage
In the full sample of patients not in SUD treatment who were referred to an affiliated SUD treatment program and for whom program intake data were available (n= 77), 27% kept their intake appointment after discharge. In the subset of patients with current opioid use disorder who were referred to an affiliated program (n=45), 42% of patients who were newly initiated on OAT in the hospital kept their intake appointment, compared with 17% for those who did not initiate OAT. However, this difference was not statistically significant (p= .096) in this small subset.
4. Discussion
Hospital CL services specializing in substance use disorders offer a promising form of intervention that can help address the complex needs of those with ongoing medical problems that may be directly caused or exacerbated by substance use. Such services can feasibly be developed and integrated into hospital settings (Aszalos et al., 1999; Fuller and Jordan, 1994; McDuff et al., 1997; Murphy et al., 2009; Trowbridge et al., 2017; Wakeman et al., 2017). These service teams can focus on SUD-related problems (e.g., acute opioid withdrawal) and provide attending medical/surgical teams with recommendations regarding the management of such problems, augmenting the overall care of this population by directly addressing their SUD and related medical issues.
This study found that even within a high-risk group of hospital patients with SUDs receiving specialty CL services, patients with opioid use disorders are at especially elevated risk of rehospitalization. Opioid use disorder is a public health problem of epidemic proportions in the US that contributes to a myriad of acute and chronic health problems. Hospitalizations stemming from opioid use disorder and its consequences have increased rapidly over the last decade, particularly among those who inject drugs (Ronan et al., 2016; Wurcel et al., 2016). Additionally, untreated opioid use disorders can contribute to non-adherence to health care (Tawk et al., 2013; Gonzalez et al., 2011). A recent national study found that each year about 1 in 4 individuals with OUD experience inpatient hospitalization (Gryczynski et al., 2016). Some of these hospitalizations may be avoidable with engagement in preventive care or improved adherence to medical advice and medication regimens. Hospitalization offered a potential “reachable moment” to engage patients with substance use disorders in addiction treatment and recommended post-discharge health care, who may not otherwise seek such services (Trowbridge et al., 2017).
Research shows that initiation of pharmacotherapy for OUD during hospital admission has the promise to improve linkage to outpatient OUD treatment (Aszalos et al., 1999; Lee et al., 2017; Liebschutz et al., 2014; Shanahan et al., 2010). A hospital-based program model dedicated to transitioning hospital patients with OUD to outpatient care was found to be effective in linking a large majority of patients to outpatient methadone treatment after medication initiation during hospitalization (Shanahan et al., 2010). A randomized trial of initiating buprenorphine treatment during hospital admission found that this approach was far superior to providing medically managed opioid withdrawal for linking patients to continued treatment in the community (Liebshutz et al., 2014). Likewise, a randomized trial found significantly higher rates of treatment entry among patients who initiated buprenorphine in an Emergency Department compared with those who received brief intervention or referral (D’Onofrio et al., 2015; D’Onofrio et al., 2017). However, the current study did not find that in-hospital initiation of opioid agonist treatment led to a reduction in subsequent rehospitalization, although this small study was likely underpowered to detect such a relationship. More rigorous research is needed on the ability of opioid agonist treatment and other services to reduce hospital readmissions and improve patient outcomes. Other services combined with pharmacotherapy, such as patient navigation, proactive case management, or contingency management could potentially help improve outpatient SUD and medical treatment adherence post-discharge.
In addition to the higher risk of hospitalization among patients with opioid use disorder, cocaine use disorder was also associated with rehospitalization in some analyses. Perhaps unsurprisingly, findings also suggest that the risk of rehospitalization is elevated for patients with multiple concurrent substance use disorders. However, with the exception of a number of medical comorbidities, none of the other patient characteristics examined were associated with rehospitalization in this sample. It is important to note that the current study sample was limited to patients seen by the SUD CL service with current opioid, cocaine, and/or alcohol use disorder at the index admission. Thus, the findings must be interpreted in light of this high-risk sample with comorbid SUDs. While not reflective of a broader hospital patient sample, the current sample does reflect the most common SUD diagnostic mix among local city resident patients that are seen by this large urban hospital’s SUD consultation-liaison service. Different SUDs and use patterns could interact with specific health problems in unique ways to shape rehospitalization risk. Hospital-based SUD consultation services can play an important role in the care of a particularly vulnerable patient population.
4.1. Limitations
Our findings should be considered in light of study design and limitations. Notably, the interventions and services delivered by this specialized SUD CL team have been well-developed over time and are often tailored to individual needs (e.g., dependent on insurance status, the location of residence, mobility status). As a result, their services likely go beyond the typical care in other hospitals without an established CL service. Nevertheless, more hospitals are establishing and expanding such services in recognition of the prominent role that substance use problems play in many patients’ presenting problems and clinical prognosis, as well as costs and inefficiencies associated with avoidable hospitalizations in which SUDs may play a role.
Although we assessed linkage to treatment, data were limited to intake information for the hospital’s two outpatient treatment programs. These programs were typically the most common point of referral for continued SUD treatment post-hospitalization, but it is possible that some patients accessed treatment at one of the many other SUD treatment facilities in the city, for which no record was available. Additionally, we were also only able to ascertain whether a patient had kept their initial appointment at these affiliated SUD programs and were not able to evaluate treatment retention. Importantly, data on rehospitalization were limited to the University of Maryland Medical Center. It is likely that there were additional hospitalizations in other local hospitals that we were unable to capture. Because this was a medical records review at a single large hospital, we could not ascertain incarceration, relocation, or death after discharge within the 180-day period under consideration. It is possible that unmeasured factors accounted for patients’ initiation of OAT in the hospital. Likewise, there are other important drivers of hospital readmission, such as housing status and severity of medical illness, that were unable to be considered in this study due to either constraint on scope and resources or lack of consistent information in the medical record. Future studies of hospitalization among medical patients with comorbid SUDs should consider a broader range of prognostic factors and potential confounds.
4.2. Conclusions
Hospital-based SUD consultation-liaison services have great potential to increase the quality of care for SUDs and address their role in shaping medical outcomes. Future research should continue to investigate approaches to facilitating SUD treatment entry and engagement, as well as strategies to reduce avoidable hospitalizations. Strategies to optimize engagement of hospital patients with SUDs in addiction treatment and appropriate follow-up medical care are urgently needed and represent important areas of future investigation.
Highlights.
This study examined rehospitalization in patients seen by a SUD consult service.
Opioid and cocaine use disorders were associated with rehospitalization.
Hospital SUD consultation services have the potential to improve quality of care.
Acknowledgments
Role of Funding Source
This study was supported by the National Institutes of Health, National Institute on Drug Abuse (NIDA) grant R01DA037942. NIDA had no role in the study design and analysis, the writing of the report, or the decision to submit the paper for publication. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Contributors
CD Nordeck led the data collection for the study, conducted literature review, assisted in the statistical analysis for this manuscript, and drafted the manuscript. J Gryczynski acted as the Principal Investigator for the pilot study, designed the study protocol, led the data analyses and contributed to the writing of the manuscript. C Welsh was the director of the consultation liaison service and facilitated the data acquisition and abstraction, with the assistance and guidance of A Cohen. KE O’Grady provided guidance on the data analyses. RP Schwartz and SG Mitchell contributed to the study design and manuscript preparation. All authors contributed to the interpretation of the findings and critically reviewed the final manuscript. All authors approved the final manuscript.
Conflict of Interest
RP Schwartzin the past provided a one -time consultation to Reckitt Benckiser Pharmaceuticals on behalf of his employer Friends Research Institute. Dr. O’Grady has in the past received reimbursement for his time from Reckitt Benckiser Pharmaceuticals. The remaining authors report no conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Aszalos R, McDuff DR, Weintraub E, Montoya I, Schwartz R. Engaging hospitalized heroin-dependent patients into substance abuse treatment. J Subst Abuse Treat. 1999;17:149–158. doi: 10.1016/s0740-5472(98)00075-0. [DOI] [PubMed] [Google Scholar]
- Ahmedani BK, Solberg LI, Copeland LA, Fang-Hollingsworth Y, Stewart C, Hu J, Nerenz DR, Williams LK, Cassidy-Bushrow AE, Waxmonsky J, Lu CY. Psychiatric comorbidity and 30-day readmissions after hospitalization for heart failure, AMI, and pneumonia. Psychiatr Serv. 2015;66:134–140. doi: 10.1176/appi.ps.201300518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- D’Onofrio G, Chawarski MC, O’Connor PG, Pantalon MV, Busch SH, Owens PH, Hawk K, Bernstein SL, Fiellin DA. Emergency department-initiated buprenorphine for opioid dependence with continuation in primary care: Outcomes during and after intervention. J Gen Intern Med. 2017;32:660–666. doi: 10.1007/s11606-017-3993-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- D’Onofrio G, O’Connor PG, Pantalon MV, Chawarski MC, Busch SH, Owens PH, Bernstein SL, Fiellin DA. Emergency department–initiated buprenorphine/naloxone treatment for opioid dependence: A randomized clinical trial. J AMA. 2015;313:1636–1644. doi: 10.1001/jama.2015.3474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dziak JJ, Henry KL. Two-part predictors in regression models. Multivariate Behav Res. 2017;52:551–561. doi: 10.1080/00273171.2017.1333404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fuller RL, Atkinson G, McCullough EC, Hughes JS. Hospital readmission rates: The impacts of age, payer, and mental health diagnoses. J Ambul Care Manage. 2013;36:147–155. doi: 10.1097/JAC.0b013e3182866c1c. [DOI] [PubMed] [Google Scholar]
- Fuller MG, Jordan ML. The substance abuse consultation team: addressing the problem of hospitalized substance abusers. Gen Hosp Psychiatry. 1994;16:73–77. doi: 10.1016/0163-8343(94)90048-5. [DOI] [PubMed] [Google Scholar]
- Gonzalez A, Barinas J, O’Cleirigh C. Substance use: Impact on adherence and HIV medical treatment. Curr HIV/AIDS Reports. 2011;8:223. doi: 10.1007/s11904-011-0093-5. [DOI] [PubMed] [Google Scholar]
- Gryczynski J, Schwartz RP, O’Grady KE, Restivo L, Mitchell SG, Jaffe JH. Understanding patterns of high-cost health care use across different substance user groups. Health Aff. 2016;35:12–19. doi: 10.1377/hlthaff.2015.0618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hines AL, Barrett ML, Jiang HJ, Steiner CA. HCUP Statistical Brief #172. Agency for Healthcare Research and Quality; Rockville, MD: 2014. [accessed February 22, 2018]. Conditions with the largest number of adult hospital readmissions by payer. https://www.hcup-us.ahrq.gov/reports/statbriefs/sb172-Conditions-Readmissions-Payer.jsp. [PubMed] [Google Scholar]
- Joynt KE, Jha AK. A path forward on Medicare readmissions. New Eng J Med. 2013;368:1175–1177. doi: 10.1056/NEJMp1300122. [DOI] [PubMed] [Google Scholar]
- Lee CS, Liebschutz JM, Anderson BJ, Stein MD. Hospitalized opioid-dependent patients: Exploring predictors of buprenorphine treatment entry and retention after discharge. Am J Addict. 2017;26:667–672. doi: 10.1111/ajad.12533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liebschutz JM, Crooks D, Herman D, Anderson B, Tsui J, Meshesha LZ, Dossabhoy S, Stein M. Buprenorphine treatment for hospitalized, opioid-dependent patients: Arandomized clinical trial. JAMA Intern Med. 2014;174:1369–1376. doi: 10.1001/jamainternmed.2014.2556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Macdonald S, Anglin-Bodrug K, Mann RE, Erickson P, Hathaway A, Chipman M, Rylett M. Injury risk associated with cannabis and cocaine use. Drug Alc Depend. 2003;72:99–115. doi: 10.1016/s0376-8716(03)00202-3. [DOI] [PubMed] [Google Scholar]
- Mark T, Tomic KS, Kowlessar N, Chu BC, Vandivort-Warren R, Smith S. Hospital readmission among Medicaid patients with an index hospitalization for mental and/or substance use disorder. J Behav Health Serv Res. 2013;40:207–221. doi: 10.1007/s11414-013-9323-5. [DOI] [PubMed] [Google Scholar]
- McDuff DR, Solounias BL, Beuger M, Cohen A, Klecz M, Weintraub E. A substance abuse consultation service. Am J Addict. 1997;6:256–265. doi: 10.3109/10550499709136993. [DOI] [PubMed] [Google Scholar]
- McGeary KA, French MT. Illicit drug use and emergency room utilization. Health Serv Res. 2000;35:153. [PMC free article] [PubMed] [Google Scholar]
- Mittler JN, O’Hora JL, Harvey JB, Press MJ, Volpp KG, Scanlon DP. Turning readmission reduction policies into results: some lessons from a multistate initiative to reduce readmissions. Pop Health Manag. 2013;16:255–260. doi: 10.1089/pop.2012.0087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy MK, Chabon B, Delgado A, Newville H, Nicolson SE. Development of a substance abuse consultation and referral service in an academic medical center: Challenges, achievements and dissemination. J Clin Psychol Med Settings. 2009;16:77–86. doi: 10.1007/s10880-009-9149-8. [DOI] [PubMed] [Google Scholar]
- O’Toole TP, Conde-Martel A, Young JH, Price J, Bigelow G, Ford DE. Managing acutely ill substance-abusing patients in an integrated day hospital outpatient program: Medical therapies, complications, and overall treatment outcomes. J Gen Int Med. 2006;21:570–576. doi: 10.1111/j.1525-1497.2006.00398.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Toole TP, Stain EC, Wand G, McCaul ME, Barnhart M. Outpatient treatment entry and health care utilization after a combined medical/substance abuse intervention for hospitalized medical patients. J Gen Int Med. 2002;17:334–340. doi: 10.1046/j.1525-1497.2002.10638.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raven MC, Carrier ER, Lee J, Billings JC, Marr M, Gourevitch MN. Substance use treatment barriers for patients with frequent hospital admissions. J Subst Abuse Treat. 2010;38:22–30. doi: 10.1016/j.jsat.2009.05.009. [DOI] [PubMed] [Google Scholar]
- Raven MC, Billings JC, Goldfrank LR, Manheimer ED, Gourevitch MN. Medicaid patients at high risk for frequent hospital admission: real -time identification and remediable risks. J Urban Health. 2009;86:230–241. doi: 10.1007/s11524-008-9336-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ronan MV, Herzig SJ. Hospitalizations related to opioid abuse/dependence and associated serious infections increased sharply, 2002–12. Health Aff. 2016;35:832–837. doi: 10.1377/hlthaff.2015.1424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenthal ES, Karchmer AW, Theisen-Toupal J, Castillo RA, Rowley CF. Suboptimal addiction interventions for patients hospitalized with injection drug use-associated infective endocarditis. Am J Med. 2016;129:481–485. doi: 10.1016/j.amjmed.2015.09.024. [DOI] [PubMed] [Google Scholar]
- Schrag D, Xu F, Hanger M, Elkin E, Bickell NA, Bach PB. Fragmentation of care for frequently hospitalized urban residents. Med Care. 2006;44:560–567. doi: 10.1097/01.mlr.0000215811.68308.ae. [DOI] [PubMed] [Google Scholar]
- Shanahan CW, Beers D, Alford DP, Brigandi E, Samet JH. A transitional opioid program to engage hospitalized drug users. J Gen Int Med. 2010;25:803–808. doi: 10.1007/s11606-010-1311-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smothers BA, Yahr HT, Ruhl CE. Detection of alcohol use disorders in general hospital admissions in the United States. Arch Int Med. 2004;164:749–756. doi: 10.1001/archinte.164.7.749. [DOI] [PubMed] [Google Scholar]
- Tawk R, Freels S, Mullner R. Associations of mental, and medical illnesses with against medical advice discharges: The National Hospital Discharge Survey, 1988–2006. Admin Policy Mental Health and Mental Health Services Res. 2013;40:124–132. doi: 10.1007/s10488-011-0382-8. [DOI] [PubMed] [Google Scholar]
- Trowbridge P, Weinstein ZM, Kerensky T, Roy P, Regan D, Samet JH, Walley AY. Addiction consultation services–Linking hospitalized patients to outpatient addiction treatment. J Subst Abuse Treat. 2017;79:1–5. doi: 10.1016/j.jsat.2017.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takahashi TA, Merrill JO, Boyko EJ, Bradley KA. Type and location of injection drug use-related soft tissue infections predict hospitalization. J Urban Health. 2003;80:127–136. doi: 10.1093/jurban/jtg127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Walraven C, Jennings A, Forster AJ. A meta-analysis of hospital 30-day avoidable readmission rates. J Eval Clin Pract. 2012;18:1211–1218. doi: 10.1111/j.1365-2753.2011.01773.x. [DOI] [PubMed] [Google Scholar]
- van Walraven C, Bennett C, Jennings A, Austin PC, Forster AJ. Proportion of hospital readmissions deemed avoidable: Asystematic review. Can Med Assoc J. 2011;183:E391–402. doi: 10.1503/cmaj.101860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wakeman SE, Metlay JP, Chang Y, Herman GE, Rigotti NA. Inpatient addiction consultation for hospitalized patients increases post-discharge abstinence and reduces addiction severity. J Gen Int Med. 2017;32:909–916. doi: 10.1007/s11606-017-4077-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walley AY, Paasche-Orlow M, Lee EC, Forsythe S, Chetty VK, Mitchell S, Jack BW. Acute care hospital utilization among medical inpatients discharged with a substance use disorder diagnosis. J Addict Med. 2012;6:50–56. doi: 10.1097/ADM.0b013e318231de51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wei J, Defries T, Lozada M, Young N, Huen W, Tulsky J. An inpatient treatment and discharge planning protocol for alcohol dependence: Efficacy in reducing 30-day readmissions and emergency department visits. J Gen Int Med. 2015;30:365–370. doi: 10.1007/s11606-014-2968-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weintraub E, Dixon L, Delahanty J, Schwartz R, Johnson J, Cohen A, Klecz M. Reason for medical hospitalization among adult alcohol and drug abusers. The Am J Addict. 2001;10:167–177. doi: 10.1080/105504901750227813. [DOI] [PubMed] [Google Scholar]
- Wurcel AG, Anderson JE, Chui KK, Skinner S, Knox TA, Snydman DR, Stopka TJ. Increasing infectious endocarditis admissions among young people who inject drugs. Open Forum Infect Dis. 2016:3. doi: 10.1093/ofid/ofw157. [DOI] [PMC free article] [PubMed] [Google Scholar]