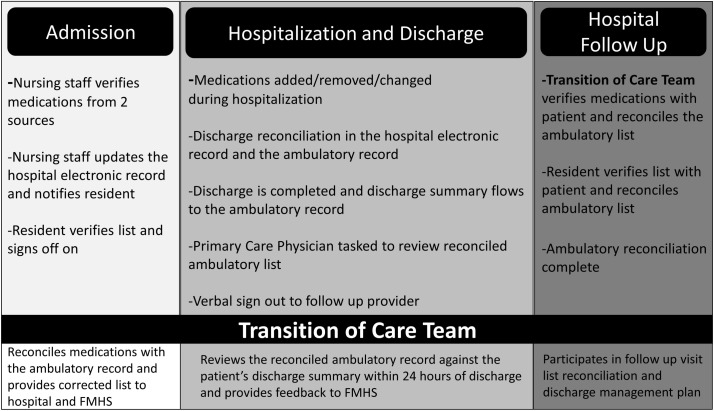
Figure 1.
Medication reconciliation process at hospital admission, discharge and follow-up visit. At hospital admission, nursing staff complete a two-step verification of medications, update the electronic record and notify the resident to sign off on the list. At discharge, medications are reconciled in the hospital and ambulatory records are forwarded to the patient’s provider. At hospital follow-up visit, both nursing staff and residents verify the medication list. Frequently, the admitting, verifying, discharging and hospital follow-up residents are different individuals. The Transition of Care Team begins ambulatory medication reconciliation at admission, reviews the list again within 24 hours of discharge and attends the follow-up visit to provide continuity of care. Use of the Transition of Care Team removed the silo structure of the initial medication reconciliation process. FMHS, Family Medicine Hospitalist Service.