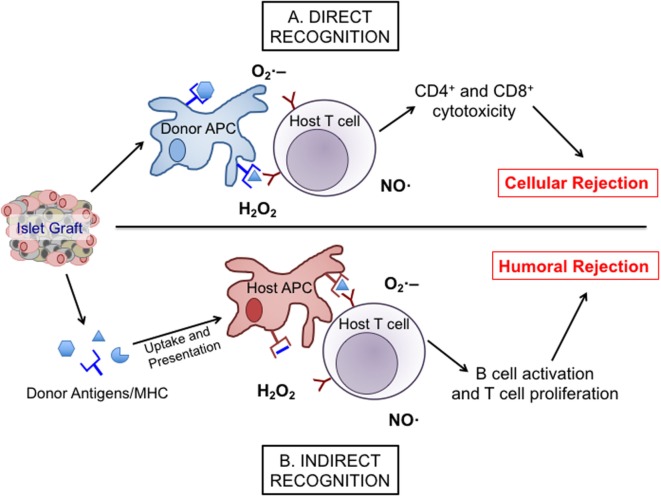
Figure 1.
The direct and indirect recognition pathways of islet allograft destruction. After transplantation, islet-resident antigen-presenting cells (APCs) from the donor graft can present directly to host T cells with stimulatory signals provided by reactive oxygen species, such as , •OH, and H2O2 to promote the expansion and activation of alloreactive cytotoxic T cell subsets. This stimulation can then activate inducible nitric oxide synthase (iNOS), NAD(P)H oxidase, and mitochondrial oxidative pathways within the T cell to produce more nitric oxide (NO), hydrogen peroxide, and superoxide, eventually leading to cellular rejection via the direct pathway (A). Alternatively, islet antigens can be shed into the surrounding environment following transplantation to be engulfed and presented by host APCs and then indirectly presented to host T cells. Through co-stimulation and the release of , •OH, H2O2, and NO, those APCs promote a classical antibody response involving the activation and expansion of alloreactive T cells and humoral rejection (B).