Abstract
Waterpipe smoking (WS), an emerging trend has major health concerns. It is prevalent worldwide as a recreational activity both indoors and outdoors. The aim of this review was to assess the impact of waterpipe smoke on the oral and respiratory system (oral cavity and pulmonary tissues). A number of studies have shown that periodontal health status is compromised in waterpipe smokers compared with non-smokers. Some studies have associated WS with oral premalignant and malignant lesions; however, due to the poor quality of these studies, the presented outcomes should be interpreted with caution. Although cigarette smoking has been considered as a potential risk factor for dental caries; there are no studies in indexed literature that have shown an association to exist between dental caries and WS. Inhaled waterpipe smoke imposes oxidative stress and inflammatory responses, and compromises the ventilatory capacity of the lungs and may lead to an increased risk of decline in lung function. WS may cause oral and pulmonary diseases, such as periodontal disease and chronic obstructive airway disease, respectively. The association between WS and development of dental caries and oral pre-cancer and their relationships with chronic airways disease requires investigations. This review discusses the current evidence of waterpipe smoke effects on the oral health and respiratory system based on basic and clinical science, and provides future directions for research and regulatory science on how WS can affect the oral cavity and the respiratory/pulmonary system.
Keywords: Dental, Hookah, Narghile, Oral, Periodontal, Pulmonary, Smoking Waterpipe, Cancer, COPD
INTRODUCTION
Waterpipe, also known as hookah, narghile or narghila, shisha or sheesha, and hubbly-bubbly, is a tobacco-smoking device. In this form of tobacco smoking, charcoal-heated air is passed through a perforated aluminium foil and across flavored tobacco to become smoke that bubbles through water before being inhaled. Nearly 100 million people use waterpipe on a daily basis (Wolfram et al., 2003); and this form of smoking causes approximately 5 million deaths per annum (Neergaard et al., 2007). WS is a cultural custom in many Middle-Eastern countries including Bahrain, Egypt, Jordan, Qatar, Saudi Arabia, Syria, Turkey, Lebanon, and the United Arab Emirates (Natto, 2005, Moh’d Al-Mulla et al., 2008, Maziak et al., 2009, Borgan et al., 2014, Jaghbir et al., 2014, Almutairi, 2015, Maziak et al., 2015a, Javed et al., 2016a); However, this form of tobacco smoking has gained popularity in many other countries including Canada, Denmark, Greece, India, Pakistan, Malaysia, Sweden, United Kingdom and the United States (U.S.) (Jensen et al., 2010, Kassim et al., 2014, Ramji et al., 2015, Hammal et al., 2016, Sidani et al., 2016). In the U.S., the Tobacco Products and Risk Perceptions Surveys of 2014 and 2015 found a prevalence of 15.8% of ever smoking waterpipe among adults (Majeed et al., 2017).
Waterpipe smoke contains toxins, such as carbon monoxide (CO), carcinogenic polycyclic aromatic volatile aldehydes and hydrocarbons, which are similar to the toxins found in cigarettes (Eissenberg & Shihadeh, 2009, Cobb et al., 2010, Cobb et al., 2011); however, waterpipe smoking (WS) is associated with nearly a 4-fold greater CO exposure and 56-fold greater inhaled smoke volume (Cobb et al., 2011). It has also been reported that levels of plasma nicotine concentration among individuals smoking waterpipe once daily are comparable to cigarette smokers who smoke up to 10 cigarettes a day (Maziak et al., 2004, Rastam et al., 2011). Moreover, waterpipe and cigarette smoking have been associated with the same health hazards, such as nicotine addiction and increased risk for a variety of oral and systemic diseases including periodontal disease and pulmonary disorders, respectively (Joseph et al., 2012, Radwan et al., 2013, Layoun et al., 2014, Javed et al., 2016a). In a retrospective study, Javed et al. (2016a) compared the clinical and radiographic periodontal status among habitual waterpipe smokers (WSS), cigarette smokers and never smokers (individuals who reported to have never consumed any form of tobacco product). The results showed that numbers of missing teeth, plaque index (PI), clinical attachment loss (CAL), probing depth (PD) ≥ 4 mm, and marginal bone loss (MBL) around teeth were statistically significantly higher among WSS and cigarette smokers compared with non-smokers. Interestingly, the results showed no statistically significant difference in these periodontal inflammatory parameters among WSS and cigarette smokers (Javed et al., 2016a). Similar results were reported by Khemiss et al. (2016) on periodontal inflammatory parameters among WSS and cigarette smokers. Results of an experimental study by Walters et al. (2017) showed that light waterpipe usage is associated with epigenetic changes and related transcriptional modifications in the investigated the effect of WS on DNA methylation of the small airway epithelium; a pathologic characteristic also manifested in cigarette smokers (Buro-Auriemma et al., 2013). To date, 300 chemical compounds have been identified in inhaled waterpipe tobacco and smoke out of which, 82 chemicals have been labelled as “toxicants” (Shihadeh and Saleh, 2005, Shihadeh et al., 2015). Examples of toxicants identified in waterpipe smoke include polyaromatic hydrocarbons (such as acenaphtylene, naphthalene and pyrene), heterocyclic compounds, carbonylic compounds (such as formaldehyde and aldehyde) and volatile organic compounds (including benzene, isoprene and styrene) (Shihadeh et al., 2015). Aside from high concentrations of tar, nicotine, carbon monoxide, other chemicals include carbonylic compounds in micrograms, such as formaldehyde, acetaldehyde, priopionaldehyde, butyraldehyde, nitosamines (N-nitrosanatabine, N′-nitrosonornicotine, N-nitrosoanabasine, polyaromatic hydrocarbons (naphthalene, acenaphtylene, fluoranthene, pyrene, heavy metals (arsenic, beryllium, lead, copper, zinc, lead, cobalt, beryllium, chromium), metal nanoparticles, phenolic compounds (catechol, resorcinol, hydroquinone, and flavoring chemicals (base propylene glycol, glycerol, vanillin, cinnamaldehyde), and free radicals which induce oral and pulmonary toxicity (Shihadeh et al., 2012). Most of these toxicants are present in cigarette smoke and have been proven to cause oral and systemic diseases, including periodontal diseases and pulmonary disorders. Since one session of waterpipe tobacco smoke inhalation is equivalent to smoking up to 10 cigarettes (Maziak et al., 2004, Rastam et al., 2011); and that WS jeopardizes oral and pulmonary health in a manner similar to conventional cigarette smoking (Buro-Auriemma et al., 2013, Javed et al., 2016a, Walters et al., 2017), it is thus hypothesized that the oral and pulmonary health statuses are compromised in WSS compared with non-smokers. Further, several studies are available on the magnitude of association between cigarette smoking and oral diseases; however, only a limited number of studies have assessed the relationship between oral inflammatory conditions (such as periodontal disease and oral cancer) among WSS. To our knowledge from indexed literature, there are no studies that have assessed the dental caries status among WSS and non-smokers. In the present study, we postulated that WSS are more susceptible to dental caries compared with non-smokers. Certainly, this hypothesis is based on the premise that smokers are prone for oral and pulmonary diseases, and we envisage similar damaging effects by WS. Overall, the aim of the present literature review was to assess the impact of waterpipe (narghile) smoking and its flavorings on oral and pulmonary tissues (oral respiratory systems).
Flavored tobacco/molasses used in waterpipe
The introduction of flavorings in tobacco (such as candy, apple, strawberry, cinnamon, grape, melon, mint, cherry, chocolate, coconut, licorice, cappuccino, spices including herbal compounds, watermelon and alcoholic beverages, such as pina colada) spurred the popularity of WS and also tempted never-smokers to start smoking (Schubert et al. 2013 Jawad and Millett, 2014, Corey et al. 2016, Cornacchione et al. 2016). There is growing evidence that flavored tobacco products have a unique appeal and may attract young users and serve as starter products to regular tobacco use (Salloum et al., 2017, Villanti et al., 2017). A systematic review of qualitative studies examining perceptions of and experiences with flavored non-menthol tobacco products found that participants believed flavored tobacco products to be less harmful than cigarettes (Kowitt et al., 2017). However, a study using gas-chromatography–mass spectrometry identified 79 volatile flavoring compounds present in waterpipe tobacco containing high amounts of the fragrance benzyl alcohol as well as considerable levels of limonene, linalool and eugenol, all of which are known as being allergenic in human skin (Schubert et al., 2013). The toxicity of these flavorings on oral and pulmonary health including obstructive lung and allergic airway diseases requires investigations. Further, there are no studies that assessed the association between oral health status and herbal fillings (herbal molasses) in waterpipe, or on flavored tobacco/molasses used in waterpipe. Certainly, this is an emerging area of research as the new products are being launched every day. The effects of flavoring chemicals used in molasses on dental/oral and pulmonary health require investigations.
Impact of waterpipe smoking on oral tissues
Oral pre-cancer and cancer
Abundant evidence has shown that pre-malignant and malignant oral lesions (such as leukoplakia and oral squamous cell carcinoma, respectively) are more often manifested in cigarette smokers compared with non-smokers (Llewellyn et al., 2004, Nayak et al., 2012, Chher et al., 2016, Ramoa et al., 2017). Similar effects of oxidative stress and inflammation are seen in plasma and lungs of smokers and patients with chronic obstructive pulmonary disease (COPD) (Rahman et al., 1996, Rahman et al., 2002). The possibility that WS is a potential risk factor for pre-malignant and malignant oral lesions cannot be disregarded since the aldehyde compounds found in waterpipe smoke are known to be carcinogenic and toxic (Al Rashidi et al., 2008). Moreover, according to Daher et al. (2010), amounts of carcinogenic volatile aldehydes and carbon monoxide emitted in the side-stream are approximately 4 and 30 times higher, respectively during a single session of WS compared with smoking one cigarette. Furthermore, concentrations of tar and its constituents are higher in waterpipe smoke compared with cigarette smoke (Shihadeh, 2003, Dar-Odeh & Abu-Hammad, 2009, Primack et al., 2016), which may undergo Fenton Chemical reactions to generate deleterious hydroxyl radicals with heavy metals (iron). Studies have shown that WS is a risk factor for malignancies of systemic organs including bladder cancer (Bedwani et al., 1997, Letasiova et al., 2012), lung cancer ( Chaouachi & Sajid, 2010, Aoun et al., 2013), esophageal cancer (Gunaid et al., 1995; Shakeri et al. 2012) and pancreatic cancer (Lo et al., 2007); however, upon an exhaustive literature search, 8 studies (El-Hakim & Uthman, 1999, Nasrollahzadeh et al., 2008, Feng et al., 2009, Malik et al., 2010, Khan et al., 2011, Dangi et al., 2012, Dar et al., 2012, Khlifi et al., 2013) that investigated the association between WS and oral cancer were identified (Table 1). The evidence from these studies (El-Hakim & Uthman, 1999, Nasrollahzadeh et al., 2008, Feng et al., 2009, Malik et al., 2010, Khan et al., 2011, Dangi et al., 2012, Dar et al., 2012, Khlifi et al., 2013) has shown that WS is possibly associated with a number of harmful health consequences including head and neck cancer. Though high-quality studies with a large sample size that have shown an association to exist between WS and oral cancer are to date unavailable; the likelihood that WS is a potential risk factor for pre-malignant and malignant oral lesions cannot be overruled. However, more research is needed in this regard.
Table 1.
Studies assessing the association between waterpipe smoking and oral cancer
| Authors | Study design | Number of subjects/patients | Duration of WS | Health outcome | Results |
|---|---|---|---|---|---|
| El-Hakim and Uthman (1999) | Case-report | 3 | Case-1: 4 years Case 2: 5 years Case 3: 20 years |
Carcinoma of the oral mucosa or lip | There might be an association between WS and oral SCC. |
| Nasrollahzadeh et al. (2008) | Case-control/Questionnaire | WSS: 20 individuals NS: 23 individuals |
≤ 19 years: 15 individuals >19 years: 5 individuals |
esophageal SSC | WS was associated with an increased risk of esophageal SSC. |
| Khan et al. (2011) | Case-control/Survey | 100 esophageal SSC patients 100 healthy controls |
NA | esophageal SSC | WS was associated with an increased risk of esophageal SSC. |
| Dangi et al. (2012) | Case-control/Survey | 761 patients with oral SSC | NA | Oral SSC | WS was associated with an increased risk of oral cancer. |
| Feng et al. (2009) | Case-control | 636 nasopharyngeal carcinoma patients 615 healthy controls |
NA | Nasopharyngeal carcinoma | WS was not associated with an increased risk of oral cancer. |
| Khlifi et al. (2013) | Case-control | 159 head and neck cancer patients 351 healthy controls |
Over 1 year | Blood Chromium and Nickel content | Blood Chromium and Nickel concentrations were significantly higher in smokers than non-smokers. |
| Dar et al. (2012) | Case-control | 702 patients with esophageal SSC 1,663 healthy controls |
Up to 33 years=318 individuals 34–45 years=423 individuals Over 46 years=376 individuals |
esophageal SSC | WS was associated with an increased risk of esophageal SSC. |
| Malik et al. (2010) | Case-control | 135 patients with esophageal SSC 195 healthy controls |
NA | esophageal SSC | WS was associated with an increased risk of esophageal SSC. |
NA: Not available; SSC: Squamous cell carcinoma; WS: Waterpipe smoking; WSS: Waterpipe smokers
Periodontal disease
There is a dearth of studies that have assessed the influence of WS on oral mucosal and periodontal tissues (Ramoa et al., 2017). It is often perceived that WS is less hazardous to health compared with cigarette smoking as the tobacco smoke in the former gets filtered through water, which absorbs a considerable amount of nicotine (Jacob et al., 2013, Jukema et al., 2014, Maziak et al., 2015b); however, results by Javed et al. (2016a) showed that WS is as hazardous to periodontal health as traditional cigarette-smoking. In this study, the authors compared the clinical (PI, PD and CAL) and radiographic (MBL) parameters of periodontal inflammation among WSS, cigarette smokers, and non-smokers. Although the results showed that compared with non-smokers, the clinical and radiographic parameters of periodontal inflammation were poorer in WSS and cigarette smokers (Javed et al., 2016a); there was no statistically significant difference in these parameters among WSS and cigarette smokers (Javed et al., 2016a). Moreover, clinical results by Natto et al. (2005) showed that the prevalence of periodontal disease is significantly greater in WSS and cigarette smokers compared with non-smokers. This study (Natto et al., 2005) concluded that the impact of smoking waterpipe towards periodontal destruction was similar to that of cigarette smoking. Similar results have been reported by other studies (Baljoon et al., 2005, Natto, 2005) (Table 2).
Table 2.
Studies assessing the impact of waterpipe smoking on periodontal tissues
| Authors et al. | Study design | Participants | Parameters assessed | Conclusion |
|---|---|---|---|---|
| Javed et al. (2016a) | Cross-sectional | WS and NS | PI, CAL, PD, MT and MBL | WS is associated with a poorer periodontal health status. |
| Natto SB (2005) | Cross-sectional | WS and NS | PI, GI, MBL and PD | WS is associated with a poorer periodontal health status. |
| Khemiss et al. (2016) | Cross-sectional | WS and NS | MBL | WS is associated with a poorer periodontal health status. |
| Natto et al. (2005) | Cross-sectional | WS and NS | PI, GI and PD | WS is associated with a poorer periodontal health status. |
| Baljoon et al. (2005) | Cross-sectional | WS and NS | MBL | WS is associated with a poorer periodontal health status. |
CAL: Clinical attachment loss; GI: Gingival index; PD: Probing depth; PI: Plaque index; MBL: Marginal bone loss; MT: Missing teeth; NS Never smokers; WS: Waterpipe smoking; WSS: Waterpipe Smokers
Association with dental caries
Dental caries is a disease of the mineralized tissues of teeth (enamel, dentin and cementum) caused by the action of cariogenic bacteria (such as streptococci and lactobacilli species) on fermentable carbohydrates, which if left uncontrolled/untreated may lead to the demineralization of these tissues and disintegration of their organic matrix (Javed et al., 2016b). A number of studies have reported that tobacco smoking is a risk factor for dental caries (particularly root surface caries) (Sugihara et al., 2010, Bharateesh & Kokila, 2014, Christensen et al., 2015, Edman et al., 2016). One explanation is that since scores of PI, CAL and MBL around teeth are significantly higher in cigarette smokers than non-smokers, the exposed root surfaces are predisposed to caries (Javed et al., 2007, Javed et al., 2016a). To date, there are no studies in indexed literature that have assessed the dental caries status among WSS. A similar mechanism may be possible for WSS rendering susceptible to infections. However, since high scores of PI and CAL have been in WSS compared with non-smokers (Javed et al., 2016a); it is hypothesized that WSS are more susceptible to develop dental caries (most probably root caries) than non-smokers (see above sections). Further studies are required to test this hypothesis.
Impact of waterpipe smoking on pulmonary tissues
According to Strulovici-Barel et al. (2016), compared with non-smokers, WSS exhibit the following characteristics: (a) more often coughing with sputum expectoration; (b) lower lung diffusing capacity; (c) abnormal epithelial lining fluid metabolome profile; (d) reduced amounts of small airway epithelia ciliated and basal cells; and (e) raised levels of apoptotic endothelial cell microparticles. Nearly 3 decades ago, in a study from Saudi Arabia, Al-Fayez et al. (1988) reported that WS is associated with a suppressed pulmonary function, which may lead to an increased risk of COPD. The authors also emphasized that WS is as hazardous to health as cigarette smoking and jeopardizes the ventilatory capacity of the lungs in WSS (Al-Fayez et al., 1988). Similarly, tobacco smoking has been associated with oxidative stress and inflammatory responses in the pathogenesis of COPD (Rahman et al., 1996, Rahman et al., 2002). Walters et al. (2017) investigated the effect of WS on DNA methylation of small airway epithelium. The results showed that waterpipe usage at least 3 times a week is associated with epigenetic changes and related transcriptional modifications in small airway epithelial cells (Walters et al., 2017), a pathologic characteristic also manifested in cigarette smokers (Buro-Auriemma et al., 2013). Waterpipe smoke reduces the proliferation of alveolar epithelial cells, causes their cell cycle arrest and increases their doubling time (Shihadeh et al., 2014), which may be associated with increased oxidative stress. In a recent experimental study on mice, chronic exposure to waterpipe smoke was associated with a statistically significant increase in the number of airway inflammatory cells (Al-Sawalha et al., 2017). In another histological study on mice, Charab et al. (2016) assessed the association between waterpipe smoke exposure and oxidative stress in lungs. Mice in the test-group were exposed to waterpipe smoke 4 times every other day for within 8 successive days and in the control-group, the mice received no exposure. The results showed that lipid peroxidation markers malondialdehyde and nitric oxide levels were statistically significantly higher in the lungs and liver of mice in the test-group compared with mice in the control-group (Charab et al., 2016). The study concluded that waterpipe smoke induces oxidative stress in the lungs (Charab et al., 2016). Moreover, it has been shown in-vitro that waterpipe smoke (a) impairs endothelial vasodilatory function and repair mechanisms, (b) increases the transcriptional expression of matrix metalloproteinase (MMP)-2 and MMP-9 and an immune response regulator, Toll Like Receptor-4 and (c) contributes in the pathogenesis of COPD by inducing inflammation and impairing cellular growth (Rammah et al., 2012, Shihadeh et al., 2014). Waterpipe smoke inhalation has also been associated with elevation in the total white blood cell count, platelet activation, and increased expression of proinflammatory cytokines (such as interleukin-6 and tumor necrosis factor-alpha) in the bronchoalveolar lavage fluid (Khabour et al., 2012). Furthermore, from a clinical perspective, habitual WS has been associated with medical conditions such as tachycardia, hypertension, and compromised pulmonary function conditions and health consequences including COPD, bronchitis and oral and lung cancer (Haddad et al., 2016, Waziry et al., 2016, Montazeri et al., 2017). WS has also been associated with low birth weight, metabolic syndrome and mental illnesses including schizophrenia, major depressive disorder and bipolar affective disorder (Hamadeh et al., 2016).
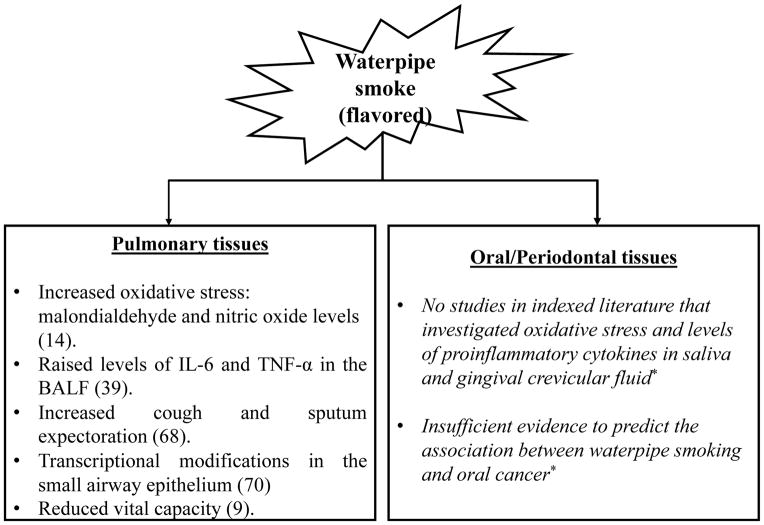
Although WS has adverse effects on pulmonary function tests (such as vital capacity, submaximal aerobic capacity and total lung capacity) (Ben Saad et al., 2013, Ben Saad et al., 2014); these negative effects have been reported to be more intense in cigarette smoking than WS (Ben Saad et al., 2013). Nevertheless, based on this, it is imprudent to consider WS as a “non-injurious” form of smoking. It is pertinent to mention that children exposed to waterpipe smoke through the environment may also demonstrate variations in their normal pulmonary function. Interestingly, results from a study from Syria showed an increased prevalence of nocturnal coughing and wheezing among children exposed to waterpipe smoke by their parents as compared to children not exposed to environmental tobacco smoke (Mohammad et al., 2014) (Table 3). Recent results from an experimental study on a mouse model showed an association between waterpipe tobacco smoke inhalation and airway inflammation (Al-Sawalha et al., 2017). WS may affect the respiratory system and the oral cavity increasing their susceptibility to infections by bacteria and viruses. Similarly, the biochemical and molecular mechanisms of waterpipe and its flavoring toxicity in users must be studied for biomarkers of toxicity (Table 4) (Rahman & Biswas, 2004), and progression of the disease so as to provide the mechanistic insights for therapeutic interventions. Further studies are required to assess the biomarkers of inflammation in the oral/periodontal tissues among WSS. The deleterious effects of WS on pulmonary health are summarized in Figure 1.
Table 3.
Studies assessing the impact of waterpipe smoking (WS) on pulmonary tissues
| Authors et al. | Study design | Participants/Subjects | Parameters assessed | Conclusion |
|---|---|---|---|---|
| Walters et al. (2017) | Experimental | Waterpipe smokers and non-smokers | Small airway epithelial cell DNA methylation | WS induces epigenetic changes and related transcriptional modifications. |
| Aoun et al. (2013) | Case-control | Lung cancer patients Healthy individuals |
Health questionnaire | WS significantly correlated with lung cancer. |
| Strulovici-Barel et al (2016) | Case-control | Waterpipe smokers Non-smokers |
Cough and sputum scores, lung function, small airway epithelial cells, plasma apoptotic endothelial cell microparticles | WS increases cough and sputum scores, lung function, small airway epithelium, plasma apoptotic endothelial cell microparticles. |
| Al-Sawalha et al. (2017) | Experimental | Mice exposed to waterpipe smoke Control mice (no exposure) |
Bronchoalveolar lavage fluid | WS augments airway inflammation by increasing the number of eosinophils, neutrophils, macrophages and lymphocytes in the bronchoalveolar lavage fluid. |
| Ben Saad et al. (2013) | Case-control | Waterpipe smokers Cigarette smokers |
Pulmonary function tests | Forced expiratory volume and forced vital capacity are compromised to a significantly greater extent in cigarette smokers than waterpipe smokers. |
Table 4.
Biomarkers and targets for periodontal and lung diseases by waterpipe smoke
| Biomarkers | Targets |
|---|---|
| Oxidative stress | Lipid peroxidation products 4-hydroxy-2-nonenal, malondialdehyde, F2-isoprostanes |
| Inflammatory responses (cytokines and prostaglandins) | NF-kappa B, Toll like receptors, NLRP3 inflammasome IL-6, IL-8, TNF-alpha |
| Exosomes/Microparticles | Distinct micro-vesicles |
| Innate host defense | RAGE receptors (S100A8 and S100A9) Advanced glycation end products Histone deacetylases (HDACs) |
| DNA methylation/epigenetic modifications | Differential |
| Proteases | Matrix metalloproteases (MMP-2, MMP-9) |
| Growth factors and proliferation of cells | VEGF, FGF, fibroblast growth factor (FGF), PDGF, TGF-β |
| Clinical parameters | PI, PD and CAL Pulmonary function (FEV1, FVC, and ratio) |
Figure 1. Summary of the impact of waterpipe smoke inhalation of pulmonary and oral tissues.
Figure showing various markers of oxidative stress and inflammation by waterpipe smoking in human biological fluids including bronchalveolar lavage fluid (BALF) as well as pathophysiological responses. IL: Interleukin; TNF-α: Tumor necrosis factor alpha
*Further studies are needed to assess the biomarkers of inflammation in the oral/periodontal tissues among waterpipe smokers
CONCLUSIONS AND FUTURE DIRECTIONS
There is sufficient evidence to confirm that WS compromises pulmonary tissues and chronic exposure to waterpipe smoke may expose its consumers to respiratory diseases. Although, there is a dearth of studies assessing the oral health status among WSS; there is a possibility that there is an increased prevalence of oral inflammatory conditions (including periodontal diseases and oral cancer) among WSS compared with non-smokers. Future studies will be directed to determine the prevalence of waterpipe (or Hookah) smoking use, and to assess the periodontal and pulmonary health status in a population by using a self-administered survey. Such cross-sectional and longitudinal studies will also help determine a possible relationship between periodontal – pulmonary diseases and waterpipe use in single or dual/poly-products (smokers and waterpipe users).
WS may cause oral and pulmonary diseases, such as periodontal disease and chronic obstructive airway disease, respectively. The association between WS and development of dental caries and oral pre-cancer and their relationships with chronic airways disease requires further investigations. Further research on WS and its flavoring detrimental effects on the oral cavity and the respiratory system based on basic and clinical science, will provide toxicological mechanisms of oral and pulmonary diseases which would be important for therapeutic targets/devising agents and tobacco regulatory science.
Acknowledgments
This study was supported by the NIH 1R01HL135613, NIH 1R01HL085613 and NIH 1R01HL085613-S1 (to I.R.), and NIH-FDA-CTP 1R01DA042470. Research reported in this publication was supported by NIDA/NIH and FDA Center for Tobacco Products (CTP). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH or the Food and Drug Administration.”
Footnotes
Authors contributions:
Drs. Fawad Javed, Shatha Subhi ALHarthi, Munerah Saleh BinShabaib, Sangeeta Gajendra, Georgios E. Romanos and Irfan Rahman wrote and edited the manuscript.
Competing Conflict of Interests Statement
The authors have declared that no conflict of interest exists.
Contributor Information
Fawad Javed, Department of General Dentistry, Eastman Institute for Oral Health, University of Rochester, NY, USA.
Shatha Subhi ALHarthi, Department of Periodontology, College of Dentistry, Princess Nourah Bint Abdulrahman University, Riyadh, Kingdom of Saudi Arabia.
Munerah Saleh BinShabaib, Department of Periodontology, College of Dentistry, Princess Nourah Bint Abdulrahman University, Riyadh, Kingdom of Saudi Arabia.
Sangeeta Gajendra, Department of Community Dentistry, Eastman Institute for Oral Health, University of Rochester, NY, USA.
Georgios E. Romanos, Department of Periodontology, School of Dental Medicine, Stony Brook University, Stony Brook, NY, USA
Irfan Rahman, Department of Environmental Medicine, School of Medicine and Dentistry, University of Rochester, Rochester, NY, USA.
References
- Al-Fayez SF, Salleh M, Ardawi M, Zahran FM. Effects of sheesha and cigarette smoking on pulmonary function of Saudi males and females. Trop Geogr Med. 1988;40(2):115–123. [PubMed] [Google Scholar]
- Al-Sawalha NA, Migdadi AM, Alzoubi KH, Khabour OF, Qinna NA. Effect of waterpipe tobacco smoking on airway inflammation in murine model of asthma. Inhal Toxicol. 2017;29(2):46–52. doi: 10.1080/08958378.2017.1280105. [DOI] [PubMed] [Google Scholar]
- Al Rashidi M, Shihadeh A, Saliba NA. Volatile aldehydes in the mainstream smoke of the narghile waterpipe. Food Chem Toxicol. 2008;46(11):3546–3549. doi: 10.1016/j.fct.2008.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Almutairi KM. Predicting Relationship of Smoking Behavior Among Male Saudi Arabian College Students Related to Their Religious Practice. J Relig Health. 2015 doi: 10.1007/s10943-015-0003-z. [DOI] [PubMed] [Google Scholar]
- Aoun J, Saleh N, Waked M, Salame J, Salameh P. Lung cancer correlates in Lebanese adults: a pilot case--control study. J Epidemiol Glob Health. 2013;3(4):235–244. doi: 10.1016/j.jegh.2013.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baljoon M, Natto S, Abanmy A, Bergstrom J. Smoking and vertical bone defects in a Saudi Arabian population. Oral Health Prev Dent. 2005;3(3):173–182. [PubMed] [Google Scholar]
- Bedwani R, el-Khwsky F, Renganathan E, Braga C, Abu Seif HH, Abul Azm T, Zaki A, Franceschi S, Boffetta P, La Vecchia C. Epidemiology of bladder cancer in Alexandria, Egypt: tobacco smoking. Int J Cancer. 1997;73(1):64–67. doi: 10.1002/(sici)1097-0215(19970926)73:1<64::aid-ijc11>3.0.co;2-5. [DOI] [PubMed] [Google Scholar]
- Ben Saad H, Babba M, Boukamcha R, Ghannouchi I, Latiri I, Mezghenni S, Zedini C, Rouatbi S. Investigation of exclusive narghile smokers: deficiency and incapacity measured by spirometry and 6-minute walk test. Respir Care. 2014;59(11):1696–1709. doi: 10.4187/respcare.03058. [DOI] [PubMed] [Google Scholar]
- Ben Saad H, Khemiss M, Nhari S, Ben Essghaier M, Rouatbi S. Pulmonary functions of narghile smokers compared to cigarette smokers: a case-control study. Libyan J Med. 2013;8:22650. doi: 10.3402/ljm.v8i0.22650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bharateesh JV, Kokila G. Association of root caries with oral habits in older individuals attending a rural health centre of a dental hospital in India. J Clin Diagn Res. 2014;8(11):Zc80–82. doi: 10.7860/JCDR/2014/8771.5165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borgan SM, Jassim G, Marhoon ZA, Almuqamam MA, Ebrahim MA, Soliman PA. Prevalence of tobacco smoking among health-care physicians in Bahrain. BMC Public Health. 2014;14:931. doi: 10.1186/1471-2458-14-931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buro-Auriemma LJ, Salit J, Hackett NR, Walters MS, Strulovici-Barel Y, Staudt MR, Fuller J, Mahmoud M, Stevenson CS, Hilton H, Ho MW, Crystal RG. Cigarette smoking induces small airway epithelial epigenetic changes with corresponding modulation of gene expression. Hum Mol Genet. 2013;22(23):4726–4738. doi: 10.1093/hmg/ddt326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chaouachi K, Sajid KM. A critique of recent hypotheses on oral (and lung) cancer induced by water pipe (hookah, shisha, narghile) tobacco smoking. Med Hypotheses. 2010;74(5):843–846. doi: 10.1016/j.mehy.2009.11.036. [DOI] [PubMed] [Google Scholar]
- Charab MA, Abouzeinab NS, Moustafa ME. The Protective Effect of Selenium on Oxidative Stress Induced by Waterpipe (Narghile) Smoke in Lungs and Liver of Mice. Biol Trace Elem Res. 2016;174(2):392–401. doi: 10.1007/s12011-016-0737-9. [DOI] [PubMed] [Google Scholar]
- Chher T, Hak S, Kallarakkal TG, Durward C, Ramanathan A, Ghani WM, Razak IA, Harun MH, Ashar NA, Rajandram RK, Prak P, Hussaini HM, Zain RB. Prevalence of oral cancer, oral potentially malignant disorders and other oral mucosal lesions in Cambodia. Ethn Health. 2016 doi: 10.1080/13557858.2016.1246431:1-15. [DOI] [PubMed] [Google Scholar]
- Christensen LB, Bardow A, Ekstrand K, Fiehn NE, Heitmann BL, Qvist V, Twetman S. Root caries, root surface restorations and lifestyle factors in adult Danes. Acta Odontol Scand. 2015;73(6):467–473. doi: 10.3109/00016357.2014.986753. [DOI] [PubMed] [Google Scholar]
- Cobb CO, Shihadeh A, Weaver MF, Eissenberg T. Waterpipe tobacco smoking and cigarette smoking: a direct comparison of toxicant exposure and subjective effects. Nicotine Tob Res. 2010;13(2):78–87. doi: 10.1093/ntr/ntq212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cobb CO, Shihadeh A, Weaver MF, Eissenberg T. Waterpipe tobacco smoking and cigarette smoking: a direct comparison of toxicant exposure and subjective effects. Nicotine Tob Res. 2011;13(2):78–87. doi: 10.1093/ntr/ntq212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cornacchione J, Wagoner KG, Wiseman KD, Kelley D, Noar SM, Smith MH, Sutfin EL. Adolescent and Young Adult Perceptions of Hookah and Little Cigars/Cigarillos: Implications for Risk Messages. J Health Commun. 2016;21(7):818–25. doi: 10.1080/10810730.2016.1177141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corey CG, Ambrose BK, Apelberg BJ, King BA. Flavored Tobacco Product Use Among Middle and High School Students--United States, 2014. MMWR Morb Mortal Wkly Rep. 2015;64(38):1066–1070. doi: 10.15585/mmwr.mm6438a2. [DOI] [PubMed] [Google Scholar]
- Daher N, Saleh R, Jaroudi E, Sheheitli H, Badr T, Sepetdjian E, Al Rashidi M, Saliba N, Shihadeh A. Comparison of carcinogen, carbon monoxide, and ultrafine particle emissions from narghile waterpipe and cigarette smoking: Sidestream smoke measurements and assessment of second-hand smoke emission factors. Atmos Environ (1994) 2010;44(1):8–14. doi: 10.1016/j.atmosenv.2009.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dangi J, Kinnunen TH, Zavras AI. Challenges in global improvement of oral cancer outcomes: findings from rural Northern India. Tob Induc Dis. 2012;10:5. doi: 10.1186/1617-9625-10-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dar-Odeh NS, Abu-Hammad OA. Narghile smoking and its adverse health consequences: a literature review. Br Dent J. 2009;206(11):571–573. doi: 10.1038/sj.bdj.2009.475. [DOI] [PubMed] [Google Scholar]
- Dar NA, Bhat GA, Shah IA, Iqbal B, Makhdoomi MA, Nisar I, Rafiq R, Iqbal ST, Bhat AB, Nabi S, Shah SA, Shafi R, Masood A, Lone MM, Zargar SA, Najar MS, Islami F, Boffetta P. Hookah smoking, nass chewing, and oesophageal squamous cell carcinoma in Kashmir, India. Br J Cancer. 2012;107(9):1618–1623. doi: 10.1038/bjc.2012.449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edman K, Ohrn K, Nordstrom B, Holmlund A. Prevalence of dental caries and influencing factors, time trends over a 30-year period in an adult population. Epidemiological studies between 1983 and 2013 in the county of Dalarna, Sweden. Acta Odontol Scand. 2016;74(5):385–392. doi: 10.3109/00016357.2016.1163733. [DOI] [PubMed] [Google Scholar]
- Eissenberg T, Shihadeh A. Waterpipe tobacco and cigarette smoking: direct comparison of toxicant exposure. Am J Prev Med. 2009;37(6):518–523. doi: 10.1016/j.amepre.2009.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- El-Hakim IE, Uthman MA. Squamous cell carcinoma and keratoacanthoma of the lower lip associated with “Goza” and “Shisha” smoking. Int J Dermatol. 1999;38(2):108–110. doi: 10.1046/j.1365-4362.1999.00448.x. [DOI] [PubMed] [Google Scholar]
- Feng BJ, Khyatti M, Ben-Ayoub W, Dahmoul S, Ayad M, Maachi F, Bedadra W, Abdoun M, Mesli S, Bakkali H, Jalbout M, Hamdi-Cherif M, Boualga K, Bouaouina N, Chouchane L, Benider A, Ben-Ayed F, Goldgar DE, Corbex M. Cannabis, tobacco and domestic fumes intake are associated with nasopharyngeal carcinoma in North Africa. Br J Cancer. 2009;101(7):1207–1212. doi: 10.1038/sj.bjc.6605281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gunaid AA, Sumairi AA, Shidrawi RG, al-Hanaki A, al-Haimi M, al-Absi S, al-Hureibi MA, Qirbi AA, al-Awlagi S, el-Guneid AM. Oesophageal and gastric carcinoma in the Republic of Yemen. Br J Cancer. 1995;71(2):409–410. doi: 10.1038/bjc.1995.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haddad L, Kelly DL, Weglicki LS, Barnett TE, Ferrell AV, Ghadban R. A Systematic Review of Effects of Waterpipe Smoking on Cardiovascular and Respiratory Health Outcomes. Tob Use Insights. 2016;9:13–28. doi: 10.4137/TUI.S39873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamadeh RR, Ansari AA, Jahrami H, Offi AA. Cigarette and waterpipe smoking among adult patients with severe and persistent mental illness in Bahrain: a comparison with the National Non-communicable Diseases Risk Factors Survey. BMC Res Notes. 2016;9:77. doi: 10.1186/s13104-016-1894-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hammal F, Wild TC, Nykiforuk C, Abdullahi K, Mussie D, Finegan BA. Waterpipe (Hookah) Smoking Among Youth and Women in Canada is New, not Traditional. Nicotine Tob Res. 2016;18(5):757–762. doi: 10.1093/ntr/ntv152. [DOI] [PubMed] [Google Scholar]
- Jacob P, 3rd, Abu Raddaha AH, Dempsey D, Havel C, Peng M, Yu L, Benowitz NL. Comparison of nicotine and carcinogen exposure with water pipe and cigarette smoking. Cancer Epidemiol Biomarkers Prev. 2013;22(5):765–772. doi: 10.1158/1055-9965.EPI-12-1422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jaghbir M, Shreif S, Ahram M. Pattern of cigarette and waterpipe smoking in the adult population of Jordan. East Mediterr Health J. 2014;20(9):529–537. [PubMed] [Google Scholar]
- Javed F, Al-Kheraif AA, Rahman I, Millan-Luongo LT, Feng C, Yunker M, Malmstrom H, Romanos GE. Comparison of Clinical and Radiographic Periodontal Status Between Habitual Water-Pipe Smokers and Cigarette Smokers. J Periodontol. 2016a;87(2):142–147. doi: 10.1902/jop.2015.150235. [DOI] [PubMed] [Google Scholar]
- Javed F, Feng C, Kopycka-Kedzierawski DT. Incidence of early childhood caries: A systematic review and meta-analysis. J Investig Clin Dent. 2016b doi: 10.1111/jicd.12238. [DOI] [PubMed] [Google Scholar]
- Javed F, Nasstrom K, Benchimol D, Altamash M, Klinge B, Engstrom PE. Comparison of periodontal and socioeconomic status between subjects with type 2 diabetes mellitus and non-diabetic controls. J Periodontol. 2007;78(11):2112–2119. doi: 10.1902/jop.2007.070186. [DOI] [PubMed] [Google Scholar]
- Jawad M, Millett C. Impact of EU flavoured tobacco ban on waterpipe smoking. BMJ. 2014 Apr 14;348:g2698. doi: 10.1136/bmj.g2698. [DOI] [PubMed] [Google Scholar]
- Jensen PD, Cortes R, Engholm G, Kremers S, Gislum M. Waterpipe use predicts progression to regular cigarette smoking among Danish youth. Subst Use Misuse. 2010;45(7–8):1245–1261. doi: 10.3109/10826081003682909. [DOI] [PubMed] [Google Scholar]
- Joseph S, Pascale S, Georges K, Mirna W. Cigarette and waterpipe smoking decrease respiratory quality of life in adults: results from a national cross-sectional study. Pulm Med. 2012;2012:868294. doi: 10.1155/2012/868294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jukema JB, Bagnasco DE, Jukema RA. Waterpipe smoking: not necessarily less hazardous than cigarette smoking : Possible consequences for (cardiovascular) disease. Neth Heart J. 2014;22(3):91–99. doi: 10.1007/s12471-013-0501-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kassim S, Al-Bakri A, Al’Absi M, Croucher R. Waterpipe tobacco dependence in U.K. male adult residents: a cross-sectional study. Nicotine Tob Res. 2014;16(3):316–325. doi: 10.1093/ntr/ntt148. [DOI] [PubMed] [Google Scholar]
- Khabour OF, Alzoubi KH, Bani-Ahmad M, Dodin A, Eissenberg T, Shihadeh A. Acute exposure to waterpipe tobacco smoke induces changes in the oxidative and inflammatory markers in mouse lung. Inhal Toxicol. 2012;24(10):667–675. doi: 10.3109/08958378.2012.710918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khan NA, Teli MA, Mohib-Ul Haq M, Bhat GM, Lone MM, Afroz F. A survey of risk factors in carcinoma esophagus in the valley of Kashmir, Northern India. J Cancer Res Ther. 2011;7(1):15–18. doi: 10.4103/0973-1482.80431. [DOI] [PubMed] [Google Scholar]
- Khemiss M, Ben Khelifa M, Ben Rejeb M, Ben Saad H. Periodontal bone height of exclusive narghile smokers compared with exclusive cigarette smokers. Libyan J Med. 2016;11:31689. doi: 10.3402/ljm.v11.31689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khlifi R, Olmedo P, Gil F, Feki-Tounsi M, Chakroun A, Rebai A, Hamza-Chaffai A. Blood nickel and chromium levels in association with smoking and occupational exposure among head and neck cancer patients in Tunisia. Environ Sci Pollut Res Int. 2013;20(11):8282–8294. doi: 10.1007/s11356-013-1466-7. [DOI] [PubMed] [Google Scholar]
- Kowitt SD, Meernik C, Baker HM, Osman A, Huang LL, Goldstein AO. Perceptions and Experiences with Flavored Non-Menthol Tobacco Products: A Systematic Review of Qualitative Studies. Int J Environ Res Public Health. 2017;14(4) doi: 10.3390/ijerph14040338. pii: E338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Layoun N, Saleh N, Barbour B, Awada S, Rachidi S, Al-Hajje A, Bawab W, Waked M, Salameh P. Waterpipe effects on pulmonary function and cardiovascular indices: a comparison to cigarette smoking in real life situation. Inhal Toxicol. 2014;26(10):620–627. doi: 10.3109/08958378.2014.945106. [DOI] [PubMed] [Google Scholar]
- Letasiova S, Medve’ova A, Sovcikova A, Dusinska M, Volkovova K, Mosoiu C, Bartonova A. Bladder cancer, a review of the environmental risk factors. Environ Health. 2012;11(Suppl 1):S11. doi: 10.1186/1476-069X-11-S1-S11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Llewellyn CD, Johnson NW, Warnakulasuriya KA. Risk factors for oral cancer in newly diagnosed patients aged 45 years and younger: a case-control study in Southern England. J Oral Pathol Med. 2004;33(9):525–532. doi: 10.1111/j.1600-0714.2004.00222.x. [DOI] [PubMed] [Google Scholar]
- Lo AC, Soliman AS, El-Ghawalby N, Abdel-Wahab M, Fathy O, Khaled HM, Omar S, Hamilton SR, Greenson JK, Abbruzzese JL. Lifestyle, occupational, and reproductive factors in relation to pancreatic cancer risk. Pancreas. 2007;35(2):120–129. doi: 10.1097/mpa.0b013e318053e7d3. [DOI] [PubMed] [Google Scholar]
- Majeed BA, Sterling KL, Weaver SR, Pechacek TF, Eriksen MP. Prevalence and harm perceptions of hookah smoking among U.S. adults, 2014–2015. Addict Behav. 2017;69:78–86. doi: 10.1016/j.addbeh.2017.01.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maziak W, Rastam S, Ibrahim I, Ward KD, Shihadeh A, Eissenberg T. CO exposure, puff topography, and subjective effects in waterpipe tobacco smokers. Nicotine Tob Res. 2009;11(7):806–811. doi: 10.1093/ntr/ntp066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malik MA, Upadhyay R, Mittal RD, Zargar SA, Mittal B. Association of xenobiotic metabolizing enzymes genetic polymorphisms with esophageal cancer in Kashmir Valley and influence of environmental factors. Nutr Cancer. 2010;62(6):734–742. doi: 10.1080/01635581003605904. [DOI] [PubMed] [Google Scholar]
- Maziak W, Taleb ZB, Bahelah R, Islam F, Jaber R, Auf R, Salloum RG. The global epidemiology of waterpipe smoking. Tob Control. 2015a;24(Suppl 1):i3–i12. doi: 10.1136/tobaccocontrol-2014-051903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maziak W, Taleb ZB, Bahelah R, Islam F, Jaber R, Auf R, Salloum RG. The global epidemiology of waterpipe smoking. Tob Control. 2015b;24(Suppl 1):i3–i12. doi: 10.1136/tobaccocontrol-2014-051903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maziak W, Ward KD, Eissenberg T. Factors related to frequency of narghile (waterpipe) use: the first insights on tobacco dependence in narghile users. Drug Alcohol Depend. 2004;76(1):101–106. doi: 10.1016/j.drugalcdep.2004.04.007. [DOI] [PubMed] [Google Scholar]
- Moh’d Al-Mulla A, Abdou Helmy S, Al-Lawati J, Al Nasser S, Ali Abdel Rahman S, Almutawa A, Abi Saab B, Al-Bedah AM, Al-Rabeah AM, Ali Bahaj A, El-Awa F, Warren CW, Jones NR, Asma S. Prevalence of tobacco use among students aged 13–15 years in Health Ministers’ Council/Gulf Cooperation Council Member States, 2001–2004. J Sch Health. 2008;78(6):337–343. doi: 10.1111/j.1746-1561.2008.00311.x. [DOI] [PubMed] [Google Scholar]
- Mohammad Y, Shaaban R, Hassan M, Yassine F, Mohammad S, Tessier JF, Ellwood P. Respiratory effects in children from passive smoking of cigarettes and narghile: ISAAC Phase Three in Syria. Int J Tuberc Lung Dis. 2014;18(11):1279–1284. doi: 10.5588/ijtld.13.0912. [DOI] [PubMed] [Google Scholar]
- Montazeri Z, Nyiraneza C, El-Katerji H, Little J. Waterpipe smoking and cancer: systematic review and meta-analysis. Tob Control. 2017;26(1):92–97. doi: 10.1136/tobaccocontrol-2015-052758. [DOI] [PubMed] [Google Scholar]
- Nasrollahzadeh D, Kamangar F, Aghcheli K, Sotoudeh M, Islami F, Abnet CC, Shakeri R, Pourshams A, Marjani HA, Nouraie M, Khatibian M, Semnani S, Ye W, Boffetta P, Dawsey SM, Malekzadeh R. Opium, tobacco, and alcohol use in relation to oesophageal squamous cell carcinoma in a high-risk area of Iran. Br J Cancer. 2008;98(11):1857–1863. doi: 10.1038/sj.bjc.6604369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Natto S, Baljoon M, Bergstrom J. Tobacco smoking and periodontal health in a Saudi Arabian population. J Periodontol. 2005;76(11):1919–1926. doi: 10.1902/jop.2005.76.11.1919. [DOI] [PubMed] [Google Scholar]
- Natto SB. Tobacco smoking and periodontal health in a Saudi Arabian population. Swed Dent J Suppl. 2005;176:8–52. [PubMed] [Google Scholar]
- Nayak S, Chandra S, Mehrotra D, Kumar S, Agrawal SP, Kumar S, Goel MM. Effect of tobacco, alcohol, and smoking habits in oral precancer with histological proven epithelial dysplasia. J Oral Biol Craniofac Res. 2012;2(3):159–162. doi: 10.1016/j.jobcr.2012.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neergaard J, Singh P, Job J, Montgomery S. Waterpipe smoking and nicotine exposure: a review of the current evidence. Nicotine Tob Res. 2007;9(10):987–994. doi: 10.1080/14622200701591591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Primack BA, Carroll MV, Weiss PM, Shihadeh AL, Shensa A, Farley ST, Fine MJ, Eissenberg T, Nayak S. Systematic Review and Meta-Analysis of Inhaled Toxicants from Waterpipe and Cigarette Smoking. Public Health Rep. 2016;131(1):76–85. doi: 10.1177/003335491613100114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radwan G, Hecht SS, Carmella SG, Loffredo CA. Tobacco-specific nitrosamine exposures in smokers and nonsmokers exposed to cigarette or waterpipe tobacco smoke. Nicotine Tob Res. 2013;15(1):130–138. doi: 10.1093/ntr/nts099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rahman I, Biswas SK. Non-invasive biomarkers of oxidative stress: reproducibility and methodological issues. Redox Rep. 2004;9(3):125–143. doi: 10.1179/135100004225005219. [DOI] [PubMed] [Google Scholar]
- Rahman I, Morrison D, Donaldson K, MacNee W. Systemic oxidative stress in asthma, COPD, and smokers. Am J Respir Crit Care Med. 1996;154(4 Pt 1):1055–1060. doi: 10.1164/ajrccm.154.4.8887607. [DOI] [PubMed] [Google Scholar]
- Rahman I, van Schadewijk AA, Crowther AJ, Hiemstra PS, Stolk J, MacNee W, De Boer WI. 4-Hydroxy-2-nonenal, a specific lipid peroxidation product, is elevated in lungs of patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2002;166(4):490–495. doi: 10.1164/rccm.2110101. [DOI] [PubMed] [Google Scholar]
- Ramji R, Arnetz J, Nilsson M, Jamil H, Norstrom F, Maziak W, Wiklund Y, Arnetz B. Determinants of waterpipe use amongst adolescents in Northern Sweden: a survey of use pattern, risk perception, and environmental factors. BMC Res Notes. 2015;8:441. doi: 10.1186/s13104-015-1413-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rammah M, Dandachi F, Salman R, Shihadeh A, El-Sabban M. In vitro cytotoxicity and mutagenicity of mainstream waterpipe smoke and its functional consequences on alveolar type II derived cells. Toxicol Lett. 2012;211(3):220–231. doi: 10.1016/j.toxlet.2012.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramoa CP, Eissenberg T, Sahingur SE. Increasing popularity of waterpipe tobacco smoking and electronic cigarette use: Implications for oral healthcare. J Periodontal Res. 2017 doi: 10.1111/jre.12458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rastam S, Eissenberg T, Ibrahim I, Ward KD, Khalil R, Maziak W. Comparative analysis of waterpipe and cigarette suppression of abstinence and craving symptoms. Addict Behav. 2011;36(5):555–559. doi: 10.1016/j.addbeh.2011.01.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salloum RG, Thrasher JF, Getz KR, Barnett TE, Asfar T, Maziak W. Patterns of Waterpipe Tobacco Smoking Among U.S. Young Adults, 2013–2014. Am J Prev Med. 2017;52(4):507–512. doi: 10.1016/j.amepre.2016.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schubert J, Luch A, Schulz TG. Waterpipe smoking: analysis of the aroma profile of flavored waterpipe tobaccos. Talanta. 2013;115:665–674. doi: 10.1016/j.talanta.2013.06.022. [DOI] [PubMed] [Google Scholar]
- Shakeri R, Kamangar F, Nasrollahzadeh D, Nouraie M, Khademi H, Etemadi A, Islami F, Marjani H, Fahimi S, Sepehr A, Rahmati A, Abnet CC, Dawsey SM, Brennan P, Boffetta P, Malekzadeh R, Majdzadeh R. Is opium a real risk factor for esophageal cancer or just a methodological artifact? Hospital and neighborhood controls in case-control studies. PLoS One. 2012;7(3):e32711. doi: 10.1371/journal.pone.0032711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shihadeh A. Investigation of mainstream smoke aerosol of the argileh water pipe. Food Chem Toxicol. 2003;41(1):143–152. doi: 10.1016/s0278-6915(02)00220-x. [DOI] [PubMed] [Google Scholar]
- Shihadeh A, Saleh R. Polycyclic aromatic hydrocarbons, carbon monoxide, “tar”, and nicotine in the mainstream smoke aerosol of the narghile water pipe. Food Chem Toxicol. 2005;43(5):655–661. doi: 10.1016/j.fct.2004.12.013. [DOI] [PubMed] [Google Scholar]
- Shihadeh A, Salman R, Jaroudi E, Saliba N, Sepetdjian E, Blank MD, Cobb CO, Eissenberg T. Does switching to a tobacco-free waterpipe product reduce toxicant intake? A crossover study comparing CO, NO, PAH, volatile aldehydes, “tar” and nicotine yields. Food Chem Toxicol. 2012;50(5):1494–1498. doi: 10.1016/j.fct.2012.02.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shihadeh A, Eissenberg T, Rammah M, Salman R, Jaroudi E, El-Sabban M. Comparison of tobacco-containing and tobacco-free waterpipe products: effects on human alveolar cells. Nicotine Tob Res. 2014;16(4):496–499. doi: 10.1093/ntr/ntt193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shihadeh A, Schubert J, Klaiany J, El Sabban M, Luch A, Saliba NA. Toxicant content, physical properties and biological activity of waterpipe tobacco smoke and its tobacco-free alternatives. Tob Control. 2015;24(Suppl 1):i22–i30. doi: 10.1136/tobaccocontrol-2014-051907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sidani JE, Shensa A, Shiffman S, Switzer GE, Primack BA. Public health implications of waterpipe tobacco use in the United States warrant initial steps towards assessing dependence. Addiction. 2016;111(5):937–938. doi: 10.1111/add.13316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strulovici-Barel Y, Shaykhiev R, Salit J, Deeb RS, Krause A, Kaner RJ, Vincent TL, Agosto-Perez F, Wang G, Hollmann C, Shanmugam V, Almulla AM, Sattar H, Mahmoud M, Mezey JG, Gross SS, Staudt MR, Walters MS, Crystal RG. Pulmonary Abnormalities in Young, Light-Use Waterpipe (Hookah) Smokers. Am J Respir Crit Care Med. 2016;194(5):587–595. doi: 10.1164/rccm.201512-2470OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sugihara N, Maki Y, Okawa Y, Hosaka M, Matsukubo T, Takaesu Y. Factors associated with root surface caries in elderly. Bull Tokyo Dent Coll. 2010;51(1):23–30. doi: 10.2209/tdcpublication.51.23. [DOI] [PubMed] [Google Scholar]
- Villanti AC, Johnson AL, Ambrose BK, Cummings KM, Stanton CA, Rose SW, Feirman SP, Tworek C, Glasser AM, Pearson JL, Cohn AM, Conway KP, Niaura RS, Bansal-Travers M, Hyland A. Flavored Tobacco Product Use in Youth and Adults: Findings From the First Wave of the PATH Study (2013–2014) Am J Prev Med. 2017 doi: 10.1016/j.amepre.2017.01.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walters MS, Salit J, Ju JH, Staudt MR, Kaner RJ, Rogalski AM, Sodeinde TB, Rahim R, Strulovici-Barel Y, Mezey JG, Almulla AM, Sattar H, Mahmoud M, Crystal RG. Waterpipe smoking induces epigenetic changes in the small airway epithelium. PLoS One. 2017;12(3):e0171112. doi: 10.1371/journal.pone.0171112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waziry R, Jawad M, Ballout RA, Al Akel M, Akl EA. The effects of waterpipe tobacco smoking on health outcomes: an updated systematic review and meta-analysis. Int J Epidemiol. 2016 doi: 10.1093/ije/dyw021. [DOI] [PubMed] [Google Scholar]
- Wolfram RM, Chehne F, Oguogho A, Sinzinger H. Narghile (water pipe) smoking influences platelet function and (iso-)eicosanoids. Life Sci. 2003;74(1):47–53. doi: 10.1016/j.lfs.2003.06.020. [DOI] [PubMed] [Google Scholar]