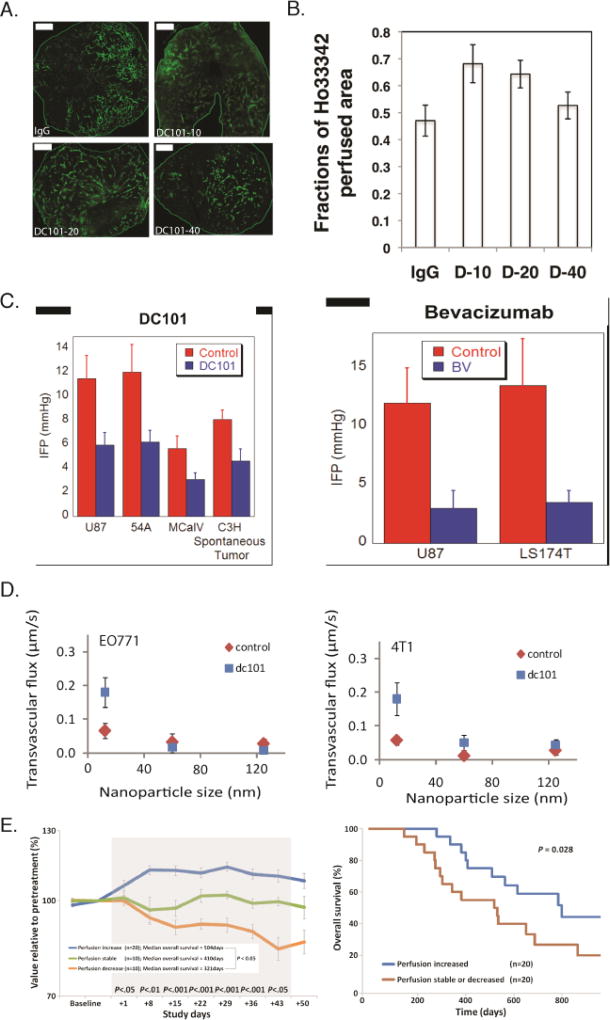
Figure 7. Vascular normalization strategy.
Normalization of tumor vessels using the monoclonal antibody DC101 improves tumor perfusion in a dose-dependent manner. (A) Perfusion images of whole-tumor tissue taken by confocal microscopy. Animals were treated with IgG (control) and 10, 20, or 40 mg/kg of DC101 (green: Sytox staining). Scale bar: 1 mm. (B) Quantification of fractions of Hoechst 33342–positive area in the whole-tumor area presents perfused regions of the tumors shown in panel A for the control (IgG) and the three DC101 doses (D-10, D-20, and D-40). (Reproduced with permission from [133]). (C) Vascular normalization with DC101 or bevacizumab reduces IFP in murine tumor models (reproduced with permission from Ref. [86]). (D) Vascular normalization of murine mammary adenocarcinomas E0771 and 4T1 improves the transvascular transport of nanoparticles in a size-dependent manner (reproduced with permission from [109]). (E) Clinical data of glioblastoma patients who received anti-angiogenic treatment and chemoradiation. Perfusion increased in 20 patients, decreased in 10 patients, and remained stable in 10 patients during combination therapy (left). Kaplan-Meier overall survival data showing that patients whose perfusion was increased exhibited an increased overall survival of ∼ 9 months (Reproduced with permission from [153]).