Abstract
Purpose: Video-assisted thoracic surgery (VATS) techniques have been widely used for resection of mediastinal tumors. This study investigated the usefulness of the subxiphoid approach in thoracoscopic thymectomy.
Methods: In all, 36 patients with anterior mediastinal tumor underwent thymectomy using the subxiphoid approach in two Japanese institutions. These patients were retrospectively reviewed and analyzed.
Results: There were 16 females and 20 males with a mean age of 57 years. Five patients underwent partial thymectomy (PT), 27 underwent total or subtotal thymectomy, and 4 underwent thymectomy with combined resection (CR) of the surrounding organs or tissues. The mean maximum tumor diameter, amount of resected tissue, and blood loss were 4.1 cm, 72.5 g, and 20.6 g, respectively. More than half of tumors were diagnosed as thymoma (n = 19). The operation time was prolonged with a greater volume of thymectomy. The duration of chest tube drainage and postoperative stay were 1.7 ± 1.0 days and 5.9 ± 7.6 days, respectively. Four patients suffered intraoperative and postoperative complications, as follows: bleeding of the innominate vein, bleeding of the internal thoracic vein, crisis of myasthenia gravis (MG), pericarditis, and phrenic nerve paralysis. There were no mortalities after surgery.
Conclusion: Subxiphoid thoracoscopic thymectomy might be a safe and useful approach for mediastinal tumors.
Keywords: subxiphoid approach, thymectomy, thoracoscopic surgery, video-assisted thoracic surgery
Introduction
Anterior mediastinal tumors, which include various types of neoplasms, are relatively rare. Thymoma is the most common tumor of the anterior mediastinum. Surgical resection for thymoma has been recommended as the principal treatment, and the completeness of resection has been considered the most important determinant of the long-term survival.1–3) We have recently reported an increased incidence of small-sized anterior mediastinal tumors.4) Such tumors are difficult to diagnose preoperatively. Median sternotomy is generally selected for resection of anterior mediastinal tumors at present, but the usage of video-assisted thoracic surgery (VATS) in mediastinal surgery has begun to spread.5–9) We recently elected to perform thymectomy via the subxiphoid approach.10,11)
In the present retrospective study, 36 cases of mediastinal tumors deemed able to be treated with thymectomy using only the subxiphoid approach were reviewed to determine the safety and usefulness of the subxiphoid approach.
Materials and Methods
From May 2014 to October 2016, 36 operations were performed using the subxiphoid approach at Aichi Medical University Hospital and Nagoya City University Hospital. These patients were retrospectively reviewed and analyzed. This retrospective study was approved by the institutional review boards of both Aichi Medical University and Nagoya City University Graduate School of Medical Sciences. Cases of partial tumor resection for a biopsy were excluded from the analysis. In addition, cases with obvious invasion to the surrounding organs in the preoperative radiological examination were excluded, as complete resection using only the subxiphoid approach was considered difficult in these patients.
Surgical technique
Surgical techniques have been already reported.10,11) For the procedure, the patient was placed in a lithotomy or supine position with their legs spread. A small transverse skin incision was typically made 1–2 cm below the lower edge of the xiphoid. A GelPOINT Mini (Applied Medical, Rancho Santa Margarita, CA, USA) or an EZ access (Hakko Medical, Nagano, Japan) was inserted and fixed. Three or two ports were able to be set through the GelPOINT Mini. Under carbon dioxide (CO2) insufflation with a positive pressure of 8 mmHg, we were able to achieve a working space to resect the thymus. We were able to perform complete thymectomy using only the subxiphoid incision. However, a second or third intercostal skin incision with a thoracic 5-mm port was added to facilitate the operation. The resected specimens were removed through the subxiphoid skin incision, which was enlarged according to the tumor size If massive adhesion was noticed during the operation, open thoracotomy was added.
Classification of thymectomy
Procedure of thymectomy was based on extended thymectomy in cases with malignant tumors and myasthenia gravis (MG). The surgical technique actually performed was retrospectively classified into three categories: partial thymectomy (PT), total or subtotal thymectomy (TT), and total or subtotal thymectomy with combined resection (CR) of the surrounding organs or tissues (CR). PT was defined as resection of the tumor and the surrounding thymus tissues. The thymic arteries and veins were preserved in PT. We used the term of TT as same as extended thymectomy. We sometimes intentionally preserve a part of thymic tissue in thymectomy. We believe thymic tissue is worth to be left. Because we think the problem of the second malignancy following thymectomy has not been dissolved yet. When only a part of the thymus, usually the left upper edge of the thymus, had to be intentionally preserved and most of the thymic tissue was resected, this operation was defined as subtotal thymectomy.12) In subtotal thymectomy, all thymic arteries and veins were dissected.
Statistical analyses
The analyzed continuous values are presented as the mean ± standard deviation. We used the t-test and a one-way analysis of variance (ANOVA) to compare the continuous values in groups. A post-hoc test was performed using the Bonferroni method. The factors which correlated with the operation time and amount of blood loss were analyzed by Pearson’s correlation coefficient and Spearman’s rank correlation tests. A linear regression analysis of the operation time was performed. Statistical significance was considered to exist at p values <0.05.
Results
Clinical data of all cases
The clinical and pathological data of all 36 cases are listed in Table 1. There were 20 males and 16 females, with a mean age of 57 years (22–83 years). The mean body mass index (BMI) was 23.1 ± 3.7. The mean maximum tumor diameter of the anterior mediastinal tumors was 4.1 ± 2.3 cm (1.2–9.0 cm). The weight of the resected specimens was 72.5 ± 49.6 g (15–212 g). Regarding the type of thymectomy, PT, TT, and CR were performed in 5, 27, and 4 cases, respectively. The combined resected organs and tissues were lung (n = 2), pericardium (n = 1), and left brachiocephalic vein (n = 1). The clinical and pathological diagnoses included thymoma (n = 19) (two cases with MG), simple thymic cyst (n = 4), thymic carcinoma or carcinoid (n = 4), malignant lymphoma (n = 3), multilocular thymic cyst (n = 2), lymphangioma (n = 1), bronchogenic cyst (n = 1), cystic teratoma with myxofibrosarcoma (n = 1), and Castleman disease (n = 1).
Table 1. Clinical data of 36 cases.
| Factors | All cases (n = 36) |
|---|---|
| Age | 57 ± 14 years (22–83 years) |
| Gender | Male (n = 20) |
| Female (n = 16) | |
| BMI | 23.1 ± 3.7 kg/m2 |
| MD | 4.1 ± 2.3 cm (1.2–9.0 cm) |
| <3.0 cm (n = 17) | |
| 3.0 ≤ MD < 5.0 cm (n = 8) | |
| 5.0 ≤ MD < 7.0 cm (n = 8) | |
| ≥7.0 (n = 3) | |
| Weight of resected specimens | 72.5 ± 49.6 g (15–212 g) |
| PT: 27.5 ± 18.1 g | |
| TT: 73.2 ± 44.4 g | |
| CR: 126.0 ± 76.0 g | |
| Operation procedure | PT (n = 5) |
| TT (n = 27) | |
| CR (n = 4) | |
| Operation time | 176.9 ± 62.6 min (94–446 min) |
| PT: 132.4 ± 40.1 min | |
| TT: 173.9 ± 41.1 min | |
| CR: 253 ± 133.0 min | |
| Intraoperative blood loss | 20.6 ± 30.3 g (0–143 g) |
| PT: 40.6 ± 60.2 g | |
| TT: 16.9 ± 23.0 g | |
| CR: 21.0 ± 23.4 g | |
| Number of skin incisions | 1 (n = 11) |
| 2 (n = 19) | |
| ≥3 (n = 6) | |
| WBC on POD 1 | 9708 ± 2307/μL |
| CRP on POD 1 | 2.5 ± 1.8 mg/dL |
| Duration of chest tube drainage | 1.7 ± 1.0 days |
| Postoperative stay | 5.9 ± 7.6 days |
| Pathological diagnoses | Thymoma (n = 20) (with MG: n = 2) |
| Simple thymic cyst (n = 4) | |
| Thymic carcinoma or carcinoid (n = 4) | |
| Malignant lymphoma (n = 3) | |
| Multilocular thymic cyst (n = 2) | |
| Bronchogenic cyst (n = 1) | |
| Lymphangioma (n = 1) | |
| Castleman disease (n = 1) | |
BMI: body mass index; PT: partial thymectomy; TT: total or subtotal thymectomy; CR: total or subtotal thymectomy with combined resection of the surrounding organs or tissues; WBC: the white blood cell count; CRP: C-reactive protein; POD: postoperative day; MG: myasthenia gravis; MD: maximum diameter
More than half of tumors were diagnosed as thymoma. The postoperative World Health Organization (WHO) pathological diagnosis13) revealed the following types and numbers: type A (n = 1), AB (n = 6), B1 (n = 6), B2 (n = 4), B3 (n = 1), and micronodular thymoma (n = 1). These thymomas were classified into the following stages: I (n = 11) and II (n = 8) according to the MasaokaKoga stage classification.1,14)
The most frequent number of skin incision, indicating the number of ports, was 2 (n = 19), and thymectomy was completed using an incision in 11 cases. One case had lateral open thoracotomy added because of massive tumor adhesion with the left lung and the left phrenic nerve. However, there were no cases requiring conversion to sternotomy.
Regarding postoperative laboratory data, the white blood cell count (WBC) and the C-reactive protein (CRP) levels before operation and on postoperative day (POD) 1 were 9700 ± 2300/μL and 2.5 ± 1.8 mg/dL, respectively. Preoperative WBC count and CRP levels, for the basis of comparison, were 6500 ± 1900/μL and 0.16 ± 0.52 mg/dL, respectively. The duration of chest tube drainage and postoperative stay were 1.7 ± 1.0 days and 5.9 ± 7.6 days, respectively. Four patients experienced five intraoperative and postoperative complications, as follows: MG crisis (n = 1), bleeding of the innominate vein (n = 1), bleeding of the internal thoracic vein (n = 1), pericarditis (n = 1), and phrenic nerve paralysis (n = 1). There were no postoperative mortalities.
Cases with complications
• Postoperative MG crisis
Case 1: A 34-year-old woman with ptosis was introduced to our hospital. During the diagnosis of MG and thymoma, systemic symptoms appeared. Her Myasthenia Gravis Foundation of America (MGFA) classification was upgraded from I to IIB. Thymectomy was performed prior to immunosuppressive therapy because she had an anterior mediastinal tumor that was likely thymoma. Total thymectomy was performed. The operation time was 184 min, and blood loss was 5 g. Only 12 hrs after the operation, dyspnea appeared postoperatively, and we diagnosed the patient with MG crisis. Tracheal intubation and mechanical ventilation were started, and immunosuppressive therapy began later. A few days later, the respirator was detached. The MG symptoms were well controlled, and she was discharged on POD 46.
• Bleeding from vessels
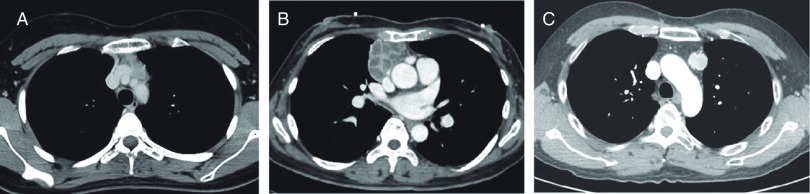
Case 2: A 22-year-old woman with anterior mediastinal tumor was introduced to our hospital. A lobulated tumor showed wide contact with the innominate vein (Fig. 1A). Several thymic veins flowed into the innominate vein from the tumor. When dissecting these vessels, the orifice of the small thymic vein into the innominate vein was torn. The bleeding was well controlled with compression, and a tissue sealing sheet was applied (TachoSil; Takeda Austria GmbH, Linz, Austria). Subsequently, total thymectomy was completed. The operation time was 202 min, and blood loss was 12 g. She was discharged on POD 4.
Fig. 1. Cases with complications or a long operation duration. (A) Case 2. Chest CT revealed a lobulated mass with wide attachment with the innominate vein. (B) Case 3. Chest CT revealed an anterior mediastinal mass 70 mm in diameter enhanced with multiple cystic lesions. (C) Case 4. Chest CT revealed an anterior mediastinal mass with calcification that was located beside the left phrenic artery in the upper portion of the anterior mediastinum. CT: computed tomography.
Case 3: A 48-year-old woman visited our hospital with a chief complaint of chest pain. Chest CT revealed an anterior mediastinal mass 7.0 cm in diameter enhanced with multiple cystic lesions (Fig. 1B). When the left upper edge of the thymus was dissected, bleeding suddenly occurred. The bleeding was well controlled with compression. Thereafter, we recognized a small tear in the orifice of the left internal thoracic vein flowing into the innominate vein. Subsequently, total thymectomy was completed. The operation time was 165 min, and blood loss was 10 g. She was discharged on POD 8.
• Phrenic nerve paralysis
Case 4: A 47-year-old man with an anterior mediastinal tumor was introduced to our hospital. With a clinical diagnosis of thymoma, the operation was performed. The tumor was located on the aorta (Fig. 1C). The left phrenic nerve was running on the edge of the tumor. Although the location of the left phrenic nerve was confirmed using the lateral view from the left side, postoperative paralysis of the left phrenic nerve occurred. The operation time was 162 min, and blood loss was 14 g. He was discharged on POD 7.
Prognosis
The mean observation period was 10.1 months (range: 0.5–26.0 months after operation). There were no mortalities in this period. In all, 26 malignant lesions were included in this study. One case with malignant lymphoma experienced recurrence, and additional treatment is in progress. In the other cases with 25 malignant lesions, no recurrences were observed.
Factors correlated with the operation time and blood loss
We analyzed the factors correlated with the operation time and blood loss as indicators to evaluate the difficulties of the operation (Table 2). Both the operation time (94–446 min) and blood loss (0–143 g) widely varied. Given that the operation time and blood loss depend on the extent of thymectomy, these values were analyzed among three thymectomy groups of PT (n = 5), TT (n = 27), and CR (n = 4). The operation time was 132 ± 41 min in PT, 174 ± 41 min in TT, and 253 ± 133 min in CR, with significant differences between the groups (Fig. 2A, p = 0.010). The operation time in CR was significantly longer than in PT and TT (p = 0.0089 and 0.038, respectively). The blood loss was 17 ± 23 g in PT, 21 ± 23 g in TT, and 41 ± 60 g in CR, with no significant differences between the groups (Fig. 2B, p = 0.283). The number of skin incisions, referring to the number of ports, also influenced the operation time (Fig. 2C, p = 0.022). The operation time in two-port surgery was significantly shorter than that for three-port surgery (p = 0.02).
Table 2. Factors correlated with the operation time and blood loss.
| Factors | Operation time (min) | Blood loss (g) | |
|---|---|---|---|
| Institutions | A | 176 ± 41 | 32 ± 35 |
| B | 178 ± 86 p = 0.93 | 5 ± 9 p = 0.0060 | |
| Gender | Female | 155 ± 34 | 20 ± 28 |
| Male | 194 ± 75 p = 0.063 | 21 ± 33 p = 0.94 | |
| Numbers of skin incision | 1 | 183 ± 49 | 26 ± 27 |
| 2 | 156 ± 38 | 14 ± 21 | |
| 3* | 234 ± 108 p = 0.022 | 31 ± 56 p = 0.42 | |
| (2 vs. 3; p = 0.02) | |||
| Thymectomy | CR | 253 ± 133 | 21 ± 23 |
| TT | 174 ± 41 | 17 ± 23 | |
| PT | 132 ± 41 p = 0.010 | 41 ± 60 p = 0.28 | |
| (CR vs. TT; p = 0.038) | |||
| (CR vs. PT; p = 0.0089) | |||
| BMI | p = 0.24 | p = 0.19 | |
| Max diameter | p = 0.023 (r = 0.377) | p = 0.20 | |
| Weight of resected sample | p = 2.0 × 10−5 (r = 0.670) | p = 0.55 | |
| Blood loss | p = 0.13 | - | |
| Age | p = 0.76 | p = 0.15 | |
*including a case with thoracotomy. PT: partial thymectomy; TT: total or subtotal thymectomy; CR: total or subtotal thymectomy with combined resection of the surrounding organs or tissues; BMI: body mass index
Fig. 2. Operation time (A) and blood loss (B) for different thymectomy procedures and operation time according to the number of ports (C).
Among the factors with continuous values, the weight of the resected specimens (p = 2.0 × 10−5, r = 0.670, Fig. 3A) and maximum tumor diameter (p = 0.023, r = 0.377, Fig. 3B) were correlated with the operation time. In addition, we plotted the data from the patients who underwent TT or CR using a single port in red. The blue circle indicates only the patients who underwent PT for a thymic cyst using a single port. In most patients who underwent TT or CR using a single port, the operation time was longer than the estimated operation time, which is estimated based on the maximum tumor diameter.
Fig. 3. Correlation of the operation time and the weight of the resected specimens (A) and maximum tumor diameter (B). The gray colored circles indicate patients with TT or CR who underwent surgery using a single port. The closed circle indicates patients with PT who underwent surgery using a single port. PT: partial thymectomy; TT: total or subtotal thymectomy; CR: total or subtotal thymectomy with combined resection of the surrounding organs or tissues.
The amount of blood loss was only correlated with the difference in the institutions. There were no other factors that correlated with the amount of blood loss.
Using a multiple regression analysis, the continuous variables were evaluated to determine their correlations with the operation time and blood loss. The operation time was regressed to the weight of the resected specimens (p = 1.84 × 10−5) and blood loss (p = 0.03). The operation time (Y) was estimated with the weight of the resected specimens (X1) and blood loss (X2), as shown below.
Discussion
The findings in the present study suggest the usefulness of thymectomy via the subxiphoid approach for anterior mediastinal tumors. Although we have experienced the cases with postoperative complications or a long operation duration as introduced above, we believe the safety and usefulness of the subxiphoid approach.
Thus far, the lateral approach has been considered the standard procedure of VATS thymectomy.5–9,15) However, while the lateral approach is useful for PT of tumors that are obviously deviated to the right or left thoracic cavity, performing total thymectomy using the lateral approach can be difficult, even with thoracic ports placed on both sides of the thoracic wall, and a cervical incision is occasionally required.11,15) As three ports are set on each side with the lateral approach, six or seven incisions may be necessary to perform total thymectomy using this approach.11,15) Reducing the number of thoracic ports led to a reduction in pain due to damage of the intercostal nerves. Therefore, we recently changed our main approach for thymectomy to the subxiphoid approach.10,11) In addition to achieving pain relief, the performance of thymectomy is easier using the subxiphoid approach than the lateral approach. In the lateral approach, the view is limited to the lateral direction. Although the lateral view is indeed very important for confirming the running of the phrenic nerve, we noticed that the vertical view from the subxiphoid port was also important for dissecting thymic arteries and veins safely. Furthermore, with the subxiphoid approach, a lateral view was easily obtained by the addition of the thoracic ports.
Some previous studies with VATS thymectomy using the lateral approach have described the weight of the resected samples (thymic tumors and thymus), with values ranging from 59.6 g to 72.5 g.16,17) Given that the mean amount of resected tissue in the present study was 72.5 g, the subxiphoid approach does not seem to be inferior to the lateral approach with respect to the weight of the resected specimens.
We also analyzed the operation time and amount of blood loss in thymectomy. The amount of blood loss only correlated with differences in institutions. Such differences may depend on the various methods used to measure the amount of the blood loss or the difference of the surgical skill. The operation time was correlated with differences in the extent of thymectomy, the number of ports, the maximum tumor diameter, and the weight of the resected specimens. These correlations are reasonable. Difficult operations, such as the CR of the surrounding organs or resection of a large tumor, require more time and an increased number of ports. Toker et al. reported a correlation between the operation time and BMI; however, we did not detect any such correlation in the present study.18)
We also performed single-port thymectomy, which was previously reported by Suda et al.19) Not setting a thoracic port seemed attractive to us, as this would likely reduce the postoperative pain although two-port thymectomy would have likely reduced the postoperative pain compared with the lateral approach. Unfortunately, we did not obtain any data regarding the postoperative pain on a numerical rating scale in the present study. However, single-port thymectomy is not an easy technique to learn. For institutions newly introducing thymectomy using the subxiphoid approach, we recommend using two or three ports initially. Increasing the number of the ports can help obtain a multidirectional view, which may be directly correlated with the safety of the procedure. Following the training of two- or three-port thymectomy, single-port thymectomy should be started. Based on our findings, we newly propose an indication for single-port thymectomy using the subxiphoid approach: it should be limited to cases with small tumors, for example, maximum tumor diameter ≤4 cm (Fig. 3B).
Although our study has several limitations, including the small sample size, short follow-up, and retrospective nature, we described our initial experiences regarding thoracoscopic resection of mediastinal tumors and the thymus via the minimally invasive subxiphoid approach. Future investigations with more patients and a longer follow-up will be required to confirm the oncological outcomes of this new procedure.
In conclusion, thoracoscopic thymectomy via the subxiphoid approach might be a safe and useful approach for treating anterior mediastinal tumors.
Disclosure Statement
All authors declare no conflicts of interest in the present study. None of the contributors had interests to disclose with regard to commercial support.
References
- 1).Masaoka A, Monden Y, Nakahara K, et al. Follow-up study of thymomas with special reference to their clinical stages. Cancer 1981; 48: 2485-92. [DOI] [PubMed] [Google Scholar]
- 2).Blumberg D, Port JL, Weksler B, et al. Thymoma: a multivariate analysis of factors predicting survival. Ann Thorac Surg 1995; 60: 908-13; discussion 914. [DOI] [PubMed] [Google Scholar]
- 3).Kondo K, Monden Y. Therapy for thymic epithelial tumors: a clinical study of 1,320 patients from Japan. Ann Thorac Surg 2003; 76: 878-84; discussion 884-5. [DOI] [PubMed] [Google Scholar]
- 4).Yano M, Sasaki H, Moriyama S, et al. Clinicopathological analysis of small-sized anterior mediastinal tumors. Surg Today 2014; 44: 1817-22. [DOI] [PubMed] [Google Scholar]
- 5).Yim AP, Kay RL, Ho JK. Video-assisted thoracoscopic thymectomy for myasthenia gravis. Chest 1995; 108: 1440-3. [DOI] [PubMed] [Google Scholar]
- 6).Demling L. Surgical endoscopy. Med Welt 1973; 24: 1253-5. [PubMed] [Google Scholar]
- 7).Landreneau RJ, Dowling RD, Castillo WM, et al. Thoracoscopic resection of an anterior mediastinal tumor. Ann Thorac Surg 1992; 54: 142-4. [DOI] [PubMed] [Google Scholar]
- 8).Mack MJ, Landreneau RJ, Yim AP, et al. Results of video-assisted thymectomy in patients with myasthenia gravis. J Thorac Cardiovasc Surg 1996; 112: 1352-9; discussion 1359-60. [DOI] [PubMed] [Google Scholar]
- 9).Nakagiri T, Inoue M, Shintani Y, et al. Improved procedures and comparative results for video-assisted thoracoscopic extended thymectomy for myasthenia gravis. Surg Endosc 2015; 29: 2859-65. [DOI] [PubMed] [Google Scholar]
- 10).Yano M, Moriyama S, Haneda H, et al. Thymectomy using the subxiphoid approach. J Thorac Cardiovasc Surg 2016; 152: 278-9. [DOI] [PubMed] [Google Scholar]
- 11).Yano M, Moriyama S, Haneda H, et al. The subxiphoid approach leads to less invasive thoracoscopic thymectomy than the lateral approach. World J Surg 2017; 41: 763-70. [DOI] [PubMed] [Google Scholar]
- 12).Yano M, Fujii Y, Yoshida J, et al. A Phase II study of partial and subtotal thymectomy for thymoma (JART02). World J Surg 2017; 41: 2033-8. [DOI] [PubMed] [Google Scholar]
- 13).Travis WD, Brambilla E, Burke AP, et al. WHO classification of tumours of the lung, pleura, thymus and heart. Lyon: International agency for research on cancer (IARC) press, 2015; pp 184-5. [Google Scholar]
- 14).Koga K, Matsuno Y, Noguchi M, et al. A review of 79 thymomas: modification of staging system and reappraisal of conventional division into invasive and non-invasive thymoma. Pathol Int 1994; 44: 359-67. [DOI] [PubMed] [Google Scholar]
- 15).Shigemura N, Shiono H, Inoue M, et al. Inclusion of the transcervical approach in video-assisted thoracoscopic extended thymectomy (VATET) for myasthenia gravis: a prospective trial. Surg Endosc 2006; 20: 1614-8. [DOI] [PubMed] [Google Scholar]
- 16).Lee CY, Kim DJ, Lee JG, et al. Bilateral video-assisted thoracoscopic thymectomy has a surgical extent similar to that of transsternal extended thymectomy with more favorable early surgical outcomes for myasthenia gravis patients. Surg Endosc 2011; 25: 849-54. [DOI] [PubMed] [Google Scholar]
- 17).Rückert JC, Walter M, Müller JM. Pulmonary function after thoracoscopic thymectomy versus median sternotomy for myasthenia gravis. Ann Thorac Surg 2000; 70: 1656-61. [DOI] [PubMed] [Google Scholar]
- 18).Toker A, Tanju S, Ziyade S, et al. Learning curve in videothoracoscopic thymectomy: how many operations and in which situations? Eur J Cardiothorac Surg 2008; 34: 155-8. [DOI] [PubMed] [Google Scholar]
- 19).Suda T, Sugimura H, Tochii D, et al. Single-port thymectomy through an infrasternal approach. Ann Thorac Surg 2012; 93: 334-6. [DOI] [PubMed] [Google Scholar]