Abstract
Objectives:
To assess vaccination timeliness, risk factors associated with delays and the reasons for delayed vaccinations among children below the age of 3 years in Jeddah, Kingdom of Saudi Arabia.
Methods:
This is a cross-sectional study conducted in Jeddah, Saudi Arabia during the period of May 2016 to August 2017. Data were obtained from parents of children under the age of 3 years using a structured questionnaire comprised of questions about sociodemographics, physical well-being of the child and the reasons that are used to justify delayed vaccinations. Vaccinations were considered delayed if they occurred more than 30 days after the time designated on the primary vaccination schedule. Logistic regression was used to assess the risk factors for vaccination delays.
Results:
The study included 351 children. Delayed vaccinations were observed in 85/351 (24.2%) of the sample. Delays were noted to occur most frequently for Measles, Mumps, Rubella vaccine (MMR), second dose of meningococcal conjugate quadrivalent vaccine (MCV4), second dose of oral polio vaccine (OPV) and fourth dose of pneumococcal conjugate vaccine (PCV) in 19/125 (15.2%) of the sample. Traveling at the time of vaccination was the most common delay reason and was reported in 31/142 (21.3%) of the sample.
Conclusion:
Adherence to vaccination is fairly common in this part of the country. However, vaccination delays are still present and should be addressed to improve health care.
Infectious diseases are a major cause of morbidity and mortality across age groups worldwide and continue to be major challenges to human survival.1 Vaccination against these diseases is considered a cost-effective method of primary health interventions that improves the well-being of children.2,3 According to the Centers for Disease Control, the morbidity of several vaccine-preventable diseases such as polio, measles and small pox decreased substantially in the United States after the introduction of vaccines during the last century.4 However, adequate vaccination coverage continues to be a major concern despite the progress in the past few decades. In 2007, it was found that 24 million children worldwide did not receive all of their required vaccinations.5 Furthermore, it is estimated that approximately 34 million children are inadequately vaccinated, with the majority of them residing in developing countries.3 Delay in vaccination is variable throughout nations. For example, a study conducted in the United States in 2005 used a national immunization survey on 14,810 children, aged 24 to 35 months, and found around 75% of these children had delays in one or more vaccinations during their first 2 years of life.6 Similarly, a cross-sectional study in Norway in 2015 used the Norwegian immunization registry (SYSVAK) reported that 44.7% of the 63,382 children below the age of 2 years experienced delayed vaccination.7 Inadequate adherence to vaccination schedules was also found in low and middle income countries. In India, a cross-sectional study carried out in 2014 using in-home interviews reported a 94.2% vaccination coverage rate among 224 children aged 12-23 months of age, although only 32% of the children were vaccinated on time.8 Similarly, in The Gambia in 2015, a cross-sectional study conducted in 4 health care centers revealed that of the 1,154 children (aged 12-24 months) examined, 63.3% of them had vaccination delays in one or more vaccines.9 Likewise in Riyadh, Saudi Arabia, out of the 385 children from 5 health centers, 22% experienced vaccination delays.10 Another study in Jeddah in 2001 used parent interviews in a tertiary hospital found that 91% of the 227 children, aged 2-52 months, were current in their vaccination schedules.11 The reasons used to justify the measured delays were variable and many factors were implicated across these studies. For instance, those belonging to minority groups and immigrants were less likely to receive their vaccination on time and vaccination timeliness was worse among those in low socioeconomic categories, those with mothers that had lower educational backgrounds and also children within larger households.8,12-17 In our study, we aim to determine the current rate of delayed vaccinations and also determine the reasons used to justify this practice. This information will be important in improving vaccination timeliness and consequently, the well-being of children in the future.
Methods
Ethical approval
This study was approved by the Biomedical Research ethics committee at the faculty of medicine at King Abdulaziz University in Jeddah, Kingdom of Saudi Arabia.
Study setting
This was an observational, cross-sectional, questionnaire-based study that was conducted between May 2016 and August 2017. Study sites were 5 primary health care centers (Abdulmajeed, Madaien Alfahad, Alfaisalia, Almatar Alqadeem and Albawadi) and 2 tertiary governmental hospitals (National Guard Hospital and King Abdulaziz University). These sites are situated in different locations in Jeddah, Saudi Arabia.
Study participants
The parents of participants were approached and the purpose of the research was explained. Parents were assured that the disclosed information will be confidential. After giving their verbal consent, parents were asked to complete a 2-page questionnaire and guidance was offered when needed.
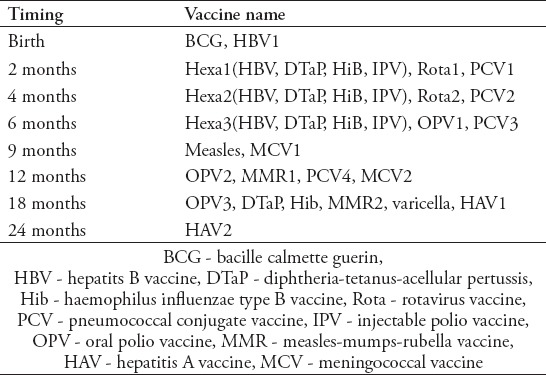
Vaccination schedule
The official vaccination schedule was enacted in 1991 by the Ministry of Health in Saudi Arabia. It includes 24 vaccines for the first 2 years of life comprising one dose of Bacille-Calmette-Guerin (BCG), one dose of Hepatitis B vaccine (HBV), 2 doses of Hepatitis A vaccine (HAV), 4 doses of hexavalent vaccine (containing Diphteria-Tetanus-Pertussis (DTaP), Hepatitis B vaccine (HBV), injectable polio (IPV) and Haemophilus influenzae type B (Hib) vaccines), 3 doses each of oral polio (OPV), 2 doses of rotavirus vaccines and 3 doses of pneumococcal conjugate vaccine (PCV). Other vaccines are one dose each of measles and varicella vaccines, 2 doses each of meningococcal (MCV) and measles-mumps-rubella (MMR) vaccines.18 The last modification to the schedule was in 2013, as they added 3 new vaccines, which included a third dose of the following vaccines: rotavirus vaccine, MCV, and MMR vaccine.19 The current vaccination schedule is provided by the Ministry of Health to all families with children and vaccines are offered free of charge at all levels of health care. These vaccinations are summarized in Table 1.
Table 1.
Primary vaccination schedule in Saudi Arabia as provided by the ministry of health.
Study questionnaire
The study used a semi-structured 28-item questionnaire. Questions were worded at a simple reading level in both Arabic and English. The study instrument was comprised of 5 sections. The first examined the child’s personal information such as date of birth, gender and nationality. The second was regarding the bio-data of the parents and inquired about their financial status, educational background and health status. The third section assessed the caretaker’s perspective on vaccinations and whether they presumed that they have vaccination delays using the Likert scale. The fourth section concentrated on the child’s physical well-being that could affect his/her vaccination status. The last section focused on possible reasons for vaccine delays. Also, a blank space was provided for the caretaker to give additional reasons.
Assessment of delay
Vaccinations were considered delayed if they were received 30 days after the designated time, based on the schedule. This definition is similar to that used in other studies.6,7 Only the vaccinations of the first year of life were assessed in this study. The vaccination cards were assessed objectively by the data collectors and parents were asked directly about the reasons behind each existing vaccine delay. Each vaccine was evaluated separately while making sure that the child was old enough to receive it.
Analysis of data
Logistic regression was used to assess risk factors associated with vaccination delay. P-values less than 0.05 were considered significant. All analyses were done using the Statistical Package for the Social Sciences (SPSS) Version 25 (IBM Corp., Armonk, NY, USA).
Results
Demographics of the participants
In total, 450 children were approached and 99 were excluded because of incomplete data on their vaccination card, missing answers in the questionnaires and/or not fulfilling the inclusion criteria in this study.
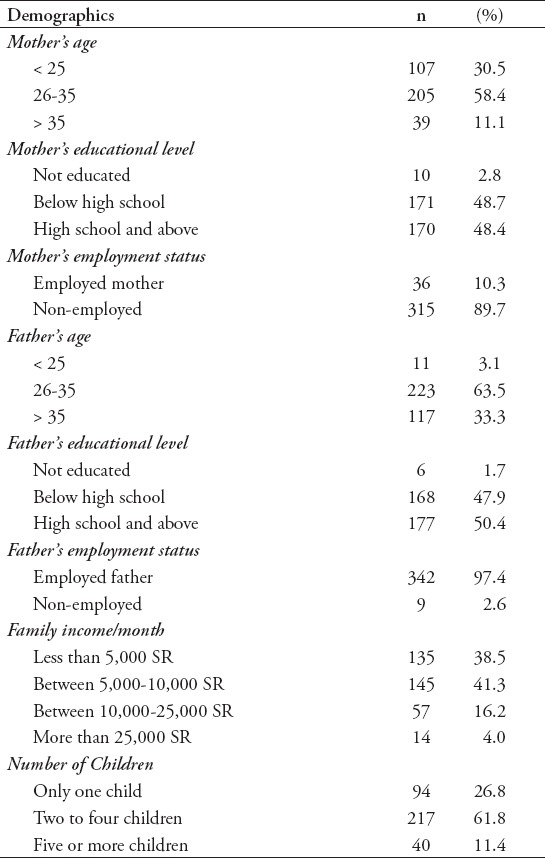
A total of 351 children were included in the analysis. Overall, the participants’ sample ages ranged between 1-35 months (mean 10.0, standard deviation 7.3), with nearly equal distributions in sex. Majority of fathers had some level of education (345\351; 98.3%) and (36\351; 10.6%) of mothers were employed. Other socio-demographic information about the participants and their parents are in Tables 2 and 3.
Table 2.
Socio-demographic characteristics of participants (N= 351).
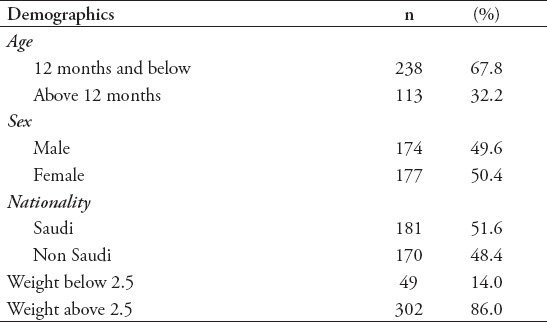
Table 3.
Socio-demographic characteristics of participants (N=351).
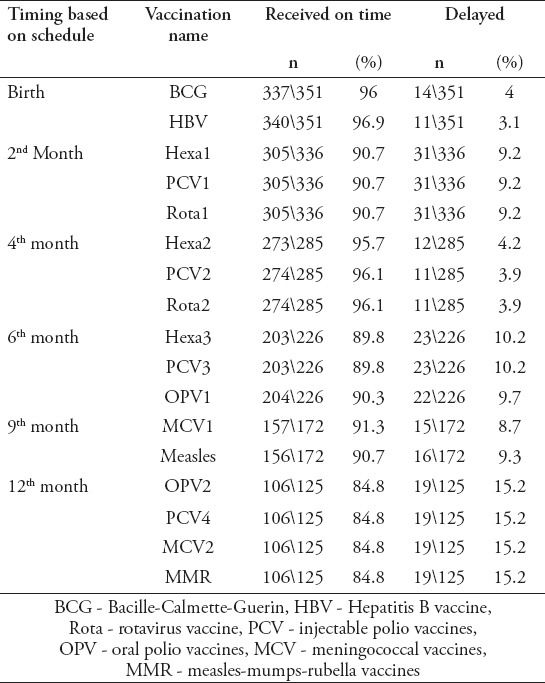
Presence of delayed vaccinations
Overall, delayed vaccinations were observed in (85\351; 24.2%) of the sample. Most had only one vaccination delay (59\85; 69.4%), while (26\85; 30.5%) had delayed vaccination on multiple occasions. Delays were assessed using the children’s vaccination card and were found to occur most frequently for MMR, 4th dose of PCV, 2nd dose of MCV, and the 2nd dose of OPV in (19\125; 15.2%), followed by the third dose of Hexa, third dose of PCV in (203\226; 10.2%). Further details are present in Table 4.
Table 4.
Details of vaccinations timeliness based on the vaccinations cards.
Factors associated with delay
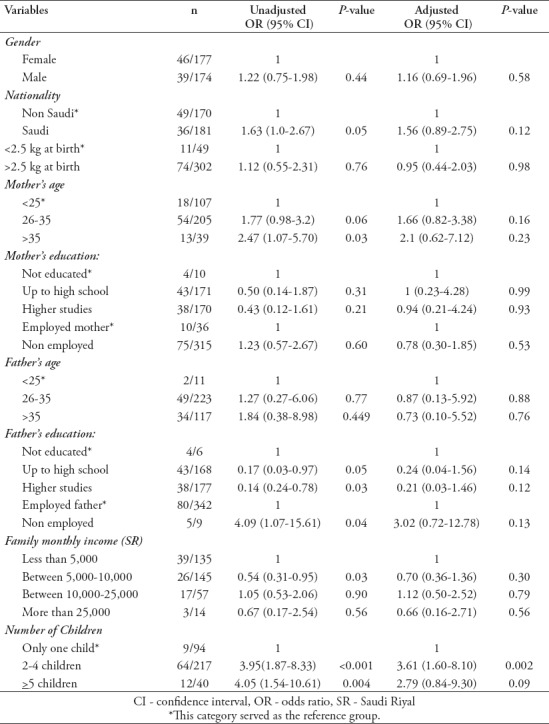
Factors associated with delayed vaccination were fathers’ employment status, fathers’ educational level, mothers age, low family income and household size. In the multivariate analysis, increasing number of children was found to be independently associated with delayed vaccinations. (Table 5)
Table 5.
Factors associated with delayed vaccination of any vaccine.
Reported reasons for vaccinations delay
Reported reasons by the parents to justify the delays are summarized in Figure 1. It demonstrates that traveling at the time of vaccination was the most common reason for delay (31\142; 21.3%), followed by the unavailability of the vaccine in the health care facility (22\142; 15.5%) and transportation issues (20\142;14.1%). Further details are presented in Figure 1.
Figure 1.
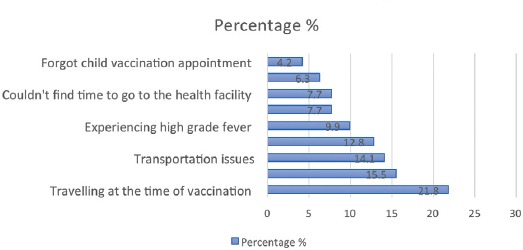
Reasons given by parents for vaccination delay.
Discussion
Our study was conducted to assess the vaccination delay rate in Jeddah, Saudi Arabia and to evaluate the factors and reasons contributing to vaccination delay among children younger than 3 years.
The vaccination delay rate observed in this study was 24.2%. Higher delay rates have been reported in international studies.6-9 A study done in India on 25,517 children below the age of 5 revealed that over 50% of them had delays.20 Yu Hu et al21 had conducted cluster surveys on 2,772 children between 24-35 months in China and discovered that age-appropriate vaccinations ranged between 25.4% for BCG to 91% for OPV1. A possible explanation for the larger difference is that both of the previous studies were either records-based or conducted through home visits, therefore, they were more likely to discover patients with delays. Also, our sample size is relatively smaller and that could have resulted in an underestimation of the problem.
However, on the national level, a similar study conducted in Riyadh, Saudi Arabia in 1992 on 383 children demonstrated a close vaccine delay rate of 22%.10 On the other hand, a previous study done in Jeddah during 2001 had a delay rate of 9%.11 The difference in delay rates compared to our study may be explained by the observation that the mean age of their participants was 3.4 months, which suggests that children in their sample had less opportunity to miss their vaccines. Also, the number of required vaccines per visit has increased since 2001, which could lead to more incidents of unavailable vaccines at the health care facilities at scheduled time of vaccinations or increases in the number or intensity of adverse events experienced by participants following vaccination.
Furthermore, it was observed that vaccines received at the age of 12 months (MMR, 4th dose of PCV, 2nd dose of both MCV and OPV) were the most delayed vaccinations. This is similar to an Iranian study done in 2011 on 2,460 children, which revealed that most delays occurred for the 12th month vaccine (MMR)(9%).22 Similarly, a systematic review done assessing timeliness of vaccinations in 31 low and middle income countries showed that only 38% of children received timely vaccination with the third dose of polio vaccine.23 This could be because final doses of vaccinations are more likely to be received with delays, also, as discovered in other studies, the more side effects children experience as a result of previous vaccines (such as swelling at the site of injection, fever and pain), the more likely for caregivers to consider skipping the upcoming vaccinations.9 In this study, about 10% of parents stated that their children experiencing post-vaccination fever was the reason for encountering vaccination delay.
The only factor that was independently significant in relation to the presence of delay was the household size. These results were also reported in studies done in Greece and Argentina.15,24 This could be because the more members in the family, the more responsibilities for the caregiver. In this study, about 8% of parents admitted that they could not find time to allocate for their childrens’ vaccinations appointments. Furthermore, it is worth noting that the financial status had no significant effect on delays in vaccinations. This could be because this sample was collected from primary health care centers and governmental hospitals, which offer vaccinations for free. These findings are opposite to what was found in other studies done in Ethiopia, Pakistan and Gabon.25-27 Moreover, no difference was found in the adequacy of vaccination between Saudi and non-Saudi children, which contradicts studies done in Pakistan and Greece that reported significant differences between citizens and foreigners.14,15 The positive observation in our study could be because the Ministry of Health in Saudi Arabia offers free-of-charge vaccinations to everyone regardless of their nationality or immigration status.
This study found that travelling at the time of vaccination is the most common reason used to justify vaccination delay. This reason was not significant in any other studies. For example, difficulties with appointment booking and non-febrile upper respiratory tract illness were the 2 common reasons for delay in the research done in Jeddah in 2001, while studies done in Karachi, Bangladesh and Burkina Faso revealed that the most common reason for delay is lack of time or knowledge among parents.11,14,28,29 It was also found that unavailability of some vaccinations was a major reason for delay in our sample, which is consistent with other studies conducted in Gambia, Greece, China and Mozambique.9,15,17,27
Study limitations
This study only included children who had their vaccination cards at the time of conducting the surveys. This may result in an underestimation of the vaccination delay in the sample. Furthermore, it was noticed that some of the vaccination cards contained inaccurate information that contradicted the caregiver knowledge, leading to an exclusion of many patients from the study. In addition, the sample size in this study is relatively small, therefore, a large-population based study may yield more accurate results. Lastly, the perception and knowledge of the caregivers were not assessed, which may play an important role in the presence of delayed vaccinations among their children. Finally, health care workers were not interviewed in this study. A study targeting their perception could explain the role of vaccination availability and appointments distribution to the presence of vaccine delay.
In conclusion, the most obvious finding to emerge from this study is a vaccination delay rate of 24.2%, which represents an alarming increase in the incidence of delayed vaccines.
One of the modifiable risk factors found is the unavailability of vaccines at the time of appointments, therefore, we recommend modifications in the supply chain and readiness of vaccines by the Ministry of Health to decrease the rate of delay. Also, more awareness programs are recommended for parents regarding the importance of vaccinating their children on time in addition to the consequences of vaccination delay.
Acknowledgment
The authors would like to thank Maram Mohammed Al-Johani, Weaam Sami Al-harbi, Shatha Meteab Al-Jamhoor and Silwan bakr Bin Sadiq Al-Bakri for their help in data collection.
Footnotes
Withdrawal policy.
By submission, the author grants the journal right of first publication. Therefore, the journal discourages unethical withdrawal of manuscripts from the publication process after peer review. The corresponding author should send a formal request signed by all co-authors stating the reason for withdrawing the manuscript. Withdrawal of a manuscript is only considered valid when the editor accepts, or approves the reason to withdraw the manuscript from publication. Subsequently, the author must receive a confirmation from the editorial office. Only at that stage, are the authors free to submit the manuscript elsewhere.
No response from the authors to all journal communication after review and acceptance is also considered unethical withdrawal. Withdrawn manuscripts noted to have already been submitted or published in another journal will be subjected to sanctions in accordance with the journal policy. The journal will take disciplinary measures for unacceptable withdrawal of manuscripts. An embargo of 5 years will be enforced for the author and their co-authors, and their institute will be notified of this action.
References
- 1.Morens DM, Folkers GK, Fauci AS. The challenge of emerging and re-emerging infectious diseases. Nature. 2010;463:122–122. doi: 10.1038/nature02759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ramalingaswami V. Importance of vaccines in child survival. Rev Infect Dis. 1989;11:S498–502. doi: 10.1093/clinids/11.supplement_3.s498. [DOI] [PubMed] [Google Scholar]
- 3.Frenkel LD, Nielsen K. Immunization issues for the 21st century. Ann Allergy Asthma Immunol. 2003;90:45–52. doi: 10.1016/s1081-1206(10)61660-2. [DOI] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention. Achievements in public health, 1900-1999 Impact of vaccines universally recommended for children -- United States, 1990-1998. MMWR Morb Mortal Wkly Rep. 1999;48:243–248. [PubMed] [Google Scholar]
- 5.Riedmann EM. Report: State of the world`s vaccines and immunization. Hum Vaccin. 2010;6:157–163. [Google Scholar]
- 6.Luman ET, Barker LE, Shaw KM, McCauley MM, Buehler JW, Pickering LK. Timeliness of childhood vaccinations in the united states: Days undervaccinated and number of vaccines delayed. JAMA. 2005;293:1204–1211. doi: 10.1001/jama.293.10.1204. [DOI] [PubMed] [Google Scholar]
- 7.Riise ØR, Laake I, Bergsaker MAR, Nøkleby H, Haugen IL, Storsæter J. Monitoring of timely and delayed vaccinations: a nation-wide registry-based study of Norwegian children aged. BMC Pediatr. 2015;15:180. doi: 10.1186/s12887-015-0487-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sood RK, Sood A, Bharti OK, Ramachandran V. High immunization coverage but delayed immunization reflects gaps in health management information system (HMIS) in district Kangra , Himachal Pradesh , India - an immunization evaluation. World J Vaccine. 2015;5:69–78. [Google Scholar]
- 9.Odutola A, Afolabi MO, Ogundare EO, Lowe-Jallow YN, Worwui A, Okebe J, et al. Risk factors for delay in age-appropriate vaccinations among gambian children. BMC Health Serv Res. 2015;15:346. doi: 10.1186/s12913-015-1015-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Al-Shehri SN, Al-Shammari SA, Khoja TA. Missed Opportunities for Immunization: A Saudi Arabia survey. Can Fam Physician. 1992;38:1087–1091. [PMC free article] [PubMed] [Google Scholar]
- 11.Hasanain FH, Jan MM. Delays in primary vaccination of infanths living in Western Saudi Arabia. Saudi Med J. 2002;23:1087–1089. [PubMed] [Google Scholar]
- 12.Danis K, Georgakopoulou T, Stavrou T, Laggas D, Panagiotopoulos T. Predictors of childhood vaccination uptake: a cross-sectional study in Greece. Procedia in Vaccinology. 2010;2:86–91. doi: 10.1016/j.vaccine.2009.11.078. [DOI] [PubMed] [Google Scholar]
- 13.Abdulraheem S, Onajole T, Jimoh G, Oladipo R. Reasons for incomplete vaccination and factors for missed opportunities among rural Nigerian children. J Public Heal Epidemiol. 2011;3:194–203. [Google Scholar]
- 14.Sheikh A, Iqbal B, Ehtamam A, Rahim M, Shaikh HA, Usmani HA, et al. Reasons for non-vaccination in pediatric patients visiting tertiary care centers in a polio-prone country. Arch Public Heal. 2013;71:19. doi: 10.1186/0778-7367-71-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pavlopoulou ID, Michail KA, Samoli E, Tsiftis G, Tsoumakas K. Immunization coverage and predictive factors for complete and age-appropriate vaccination among preschoolers in Athens, Greece: a cross- sectional study. BMC Public Health. 2013;13:908. doi: 10.1186/1471-2458-13-908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Barman MP, Nath K, Hazarika J. Factors affecting timeliness of immunization coverage among children of Assam, India: A cross-sectional study. J Health Manag. 2015;17:274–284. [Google Scholar]
- 17.Hu Y, Chen Y, Guo J, Tang X, Shen L. Completeness and timeliness of vaccination and determinants for low and late uptake among young children in eastern China. Hum Vaccin Immunother. 2014;10:1408–1415. doi: 10.4161/hv.28054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tufenkeji H, Rattan H. Childhood immunization in the Kingdom of Saudi Arabia. Ann Saudi Med. 1994;14:91–93. doi: 10.5144/0256-4947.1994.91. [DOI] [PubMed] [Google Scholar]
- 19.Ministry of Health. Ministry News - MOH: “New Vaccines Added to the National Immunization Schedule.”. 2013. Jan, pp. 1–2. Available from: https://www.moh.gov.sa/en/ministry/mediacenter/news/pages/news-2013-07-24-002.aspx .
- 20.Yadav K, Srivastava R, Kumar R, Chinnakal P, Rai SK, Krishnan A. Significant vaccination delay can occur even in a community with very high vaccination coverage: Evidence from Ballabgarh, India. J Trop Pediatr. 2012;58:133–138. doi: 10.1093/tropej/fmr059. [DOI] [PubMed] [Google Scholar]
- 21.Hu Y, Li Q, Chen Y. Timeliness of childhood primary immunization and risk factors related with delays: evidence from the 2014 Zhejiang provincial vaccination coverage survey. Int J Environ Res Public Health. 2017;14:1086. doi: 10.3390/ijerph14091086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Poorolajal J, Khazaei S, Kousehlou Z, Bathaei SJ, Zahiri A. Delayed vaccination and related predictors among infants. Iran J Public Health. 2012;41:65–71. [PMC free article] [PubMed] [Google Scholar]
- 23.Akmatov MK, Mikolajczyk RT. Timeliness of childhood vaccinations in 31 low and middle-income countries. J Epidemiol Community Health. 2012;66:e14. doi: 10.1136/jech.2010.124651. [DOI] [PubMed] [Google Scholar]
- 24.Dayan GH, Shaw KM, Baughman AL, Orellana LC, Forlenza R, Ellis A, et al. Assessment of delay in age-appropriate vaccination using survival analysis. Am J Epidemiol. 2006;163:561–570. doi: 10.1093/aje/kwj074. [DOI] [PubMed] [Google Scholar]
- 25.Bugvi AS, Rahat R, Zakar R, Zakar MZ, Fischer F, Nasrullah M, et al. Factors associated with non-utilization of child immunization in Pakistan: evidence from the Demographic and Health Survey 2006-07. BMC Public Health. 2014;14:232. doi: 10.1186/1471-2458-14-232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lakew Y, Bekele A, Biadgilign S. Factors influencing full immunization coverage among 12-23 months of age children in Ethiopia: evidence from the national demographic and health survey in 2011. BMC Public Health. 2015;15:728. doi: 10.1186/s12889-015-2078-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ategbo S, Ngoungou EB, Koko J, Vierin Y, Zang Ndong CE. Moussavou Mouyama a. Immunization coverage of children aged 0 to 5 years in Libreville (Gabon) Sante. 2010;20:215–219. doi: 10.1684/san.2010.0204. [DOI] [PubMed] [Google Scholar]
- 28.Salam MM, Uddin MS, Khan MFA, Mazumdar PK, Huq ME, Yousuf R, et al. Maternal awareness on under-5 child immunization in a rural community of Bangladesh. Int Med J. 2013;20:681–684. [Google Scholar]
- 29.Sanou A, Simboro S, Kouyaté B, Dugas M, Graham J, Bibeau G. Assessment of factors associated with complete immunization coverage in children aged 12-23 months: a cross-sectional study in Nouna district, Burkina Faso. BMC Int Health Hum Rights. 2009;9:S10. doi: 10.1186/1472-698X-9-S1-S10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Jani JV, De Schacht C, Jani IV, Bjune G. Risk factors for incomplete vaccination and missed opportunity for immunization in rural Mozambique. BMC Public Health. 2008;8:161. doi: 10.1186/1471-2458-8-161. [DOI] [PMC free article] [PubMed] [Google Scholar]


