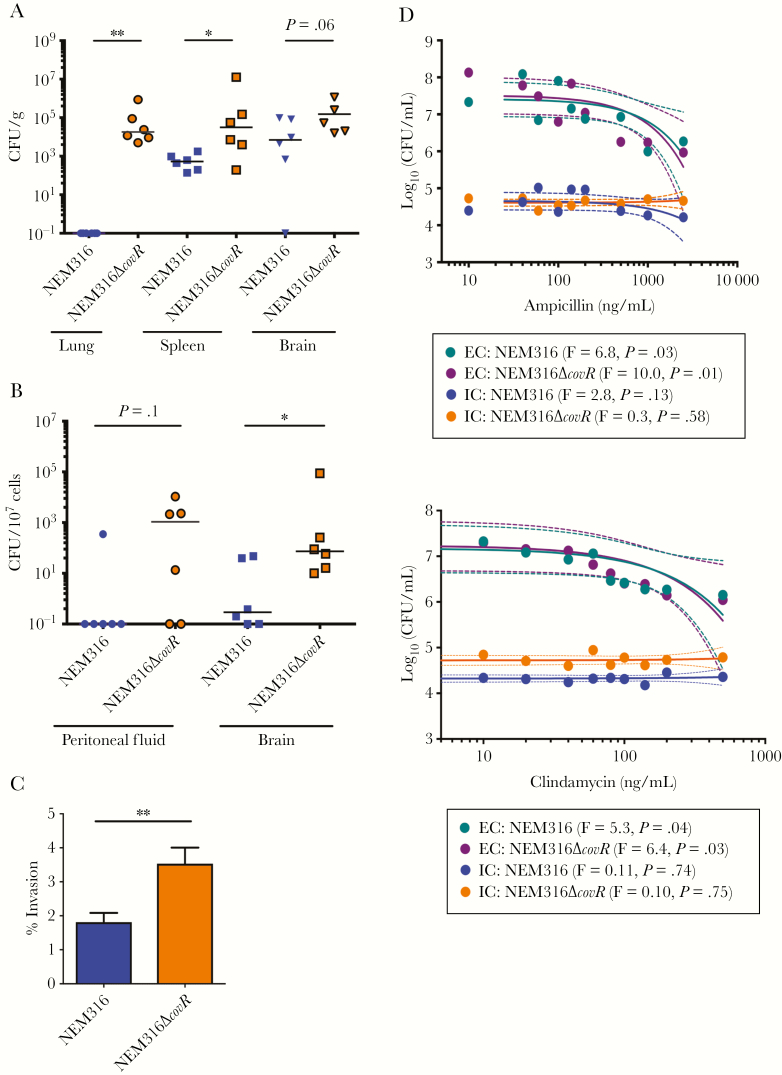
Figure 6.
Hyperhemolytic group B streptococci (GBS) with decreased capsule also exhibit increased dissemination, intracellular persistence, and antibiotic evasion. A, Wild-type (WT) C57BL6/J mice (n = 6/group) were infected intravenously with NEM316 (WT) or NEM316ΔcovR in bone marrow derived macrophages (BMDM). At 48 hours postinfection, total (A) and intracellular (B) bacterial burden was estimated. Mann–Whitney test was used to compare differences between the 2 groups. A, *P = .04, **P = .002. B, *P = .02. C, Percent invasion of GBS NEM316 and NEM316ΔcovR. Data shown is the mean of 3 independent experiments. **P = .007, Student t test, error bars ± standard error of the mean. D, Bone marrow–derived macrophages (BMDMs) containing intracellular GBS NEM316 and NEM316ΔcovR were exposed to increasing concentrations of ampicillin (top panel) or clindamycin (bottom panel) for 2 hours. Infected BMDMs were lysed to determine bactericidal effects of the antibiotics to intracellular GBS. As controls, extracellular GBS were also exposed to increasing concentrations of these antibiotics and colony-forming units (CFU) were enumerated after 2 hours. Linear regression was used to evaluate the relationship between antibiotic concentration and bacterial CFU (colored line represents regression and dashed line represents 95% confidence intervals). The F-test for each regression comparing antibiotic concentration and bacterial CFU was significant (P < .05) for extracellular bacteria (EC) and nonsignificant (P > .05) for intracellular bacteria (IC).