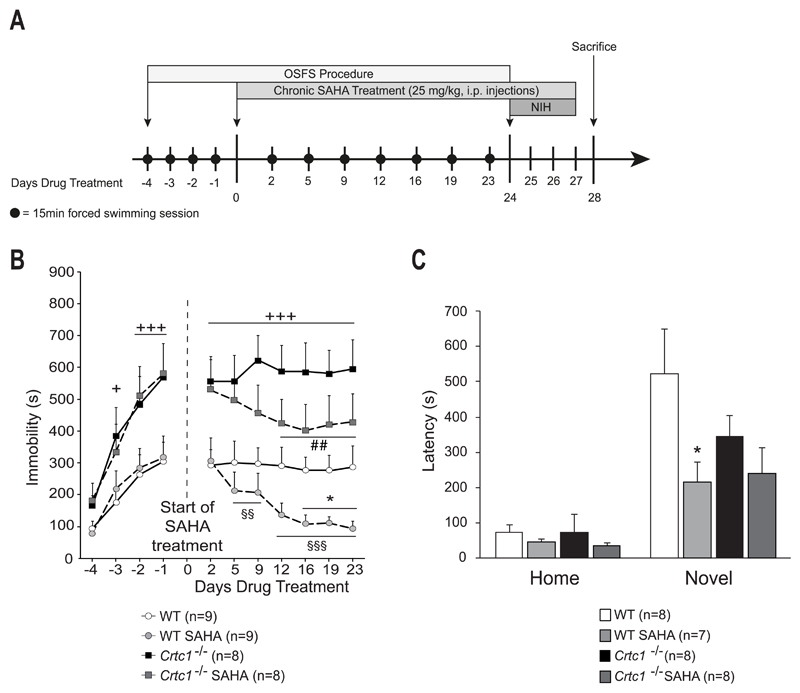
Fig. 4. Behavioral response of Crtc1‒/‒ mice to SAHA.
(A) Experimental design and timeline. The OSFS protocol started when mice reached the age of 8 weeks. Mice underwent forced swimming session during the first four days (day -4 to -1). On day 0, SAHA treatment started and continued until the end of the experiment (last injection on day 27). Swimming session were regularly repeated until day 24. The NIH test was then applied from day 24 until day 27. On day 28, animals were sacrificed. (B) Effects of chronic SAHA in the OSFS model of depression on Crtc1‒/‒ mice and WT littermates. All groups increased their immobility time during the pre-treatment period (Day -4 to day -1). Crtc1‒/‒ mice presented higher immobility time than WT mice starting from day -2 (+p<0.05, +++p<0.001, vs. WT mice). From day 0 until day 23, WT and Crtc1‒/‒ mice were daily injected i.p. with either vehicle (n=9 and n=8 respectively) or 25 mg/kg SAHA (n=9 and n=8 respectively). Vehicle-treated Crtc1‒/‒ mice were significantly more immobile that vehicle-treated WT mice during the whole procedure (+++p<0.001, vs. WT Vehicle). SAHA-treated WT mice significantly decreased their immobility time starting from day 2 of treatment (§§p<0.01, §§§p<0.001, vs. themselves on day 2). Their immobility time was also significantly lower than vehicle-treated WT mice during the last three sessions (*p<0.05, vs. WT Vehicle). SAHA-treated Crtc1‒/‒ mice significantly decreased their immobility time starting from day 12 of treatment (##p<0.01, vs. themselves on day 2). (C) Effects of chronic SAHA on the NIH paradigm. Latencies to drink sweetened condensed milk are shown in the homecage and in the novel environment. Two mice were removed for having latency scores > 2 SD from the mean. One mouse was removed for never having drunk the milk during the habituation and test phases. In the homecage conditions, no effect of SAHA was observed in any groups. In the novel environment, SAHA-treated mice (n=7) presented significant shorter latencies to drink the milk, as compared to vehicle-treated WT mice (n=8) (*p<0.05, vs. WT Vehicle). SAHA-treated Crtc1‒/‒ mice showed a non-significant trend to a shorter latency than vehicle-treated Crtc1‒/‒ mice (n=8 for each group). Data are means ±SEM.