Abstract
Purpose
Aggressive driving contributes to the high rates of post-deployment motor vehicle-related injury and death observed among veterans, and veterans cite problems with anger, aggressive driving, and road rage as being among their most pressing driving-related concerns. Both posttraumatic stress disorder (PTSD) and traumatic brain injury (TBI) have been associated with driving-related deficits in treatment-seeking samples of veterans, but the relative contribution of each of these conditions to problems with aggressive driving in the broader population of combat veterans is unclear.
Method
Chi-square and logistic regression analyses were used to examine the relative association of PTSD, TBI, and co-occurring PTSD and TBI to self-reported problems with road rage in a sample of 1102 veterans living in the mid-Atlantic region of the United States who had served in Afghanistan or Iraq.
Results
Results indicate that controlling for relevant demographic variables, PTSD without TBI (OR=3.44, p<.001), and PTSD with co-occurring TBI (OR=4.71, p<.001) were associated with increased risk of road rage, but TBI without PTSD was not.
Conclusions
Our findings suggest that PTSD, with or without comorbid TBI, may be associated with increased risk of aggressive driving in veterans. Clinical implications for treating problems with road rage are discussed, including use of interventions targeting hostile interpretation bias and training in emotional and physiological arousal regulation skills.
Keywords: military, aggression, OEF/OIF, road rage
Motor vehicle accidents (MVA) are among the highest post-deployment causes of injury and death in veterans (Krahl, Jankosky, Thomas, & Hooper, 2010; Lew et al., 2011; Woodall, Jacobson, & Crum-Cianflone, 2014). In Gulf War veterans, MVA-related deaths were observed to increase dramatically immediately post-deployment, spiking to over 10 per 100,000 persons within the first full quarter, compared to under 4 per 100,000 persons in non-deployed veterans during that time frame (Lincoln et al., 2006). More recently, insurance records reveal that veterans of the wars in Iraq or Afghanistan have a 13% increase in at-fault motor vehicle accidents from 6 months pre- to 6 months post-deployment (United States Automobile Association, 2012; Woodall et al., 2014). A recent meta-analysis of 51 studies found that driver anger is associated with increased incidence of near misses and accidents (Zhang & Chan, 2016), and one recent study found that more than 30% of recently deployed Operation Enduring Freedom (OEF) and Operation Iraqi Freedom (OIF) veterans reported significantly elevated levels of anger and aggressive driving behaviors as compared to the general population (Hwang, Peyton, Kim, Nakama-Sato, & Noble, 2014). Accidents are not the only adverse consequence of high levels of driving-related anger in combat veterans: In one sample of recently deployed OEF/OIF veterans, over one quarter of respondents reported that they “seek a personal encounter with a bad driver” at a rate of “sometimes”, “often”, or “always” (Hwang et al., 2014). Not surprisingly, veterans in treatment seeking samples cite problems with anger, aggressive driving, and road rage as being among their most pressing driving-related concerns (Hannold, Classen, Winter, Lanford, & Levy, 2013; Lew et al., 2011; Strom et al., 2013).
There are multiple factors that may contribute to aggressive driving in this population. First, military personnel who served in Iraq or Afghanistan were trained to employ aggressive, life-saving “battlemind” driving tactics that include speeding, swerving around road hazards, straddling the center line, and ignoring traffic signs (Amick, Kraft, & McGlinchey, 2013; Hannold et al., 2013; Lew, Amick, Kraft, Stein, & Cifu, 2010). Second, traumatic brain injury (TBI) and posttraumatic stress disorder (PTSD)1 are common among OEF/OIF veterans, and each has been found to be associated with increased incidence of aggressive driving (Ilie et al., 2015; Kuhn, Drescher, Ruzek, & Rosen, 2010; T. Q. Strom et al., 2012). Both conditions are characterized by cognitive functioning deficits (attention lapses, executive functioning, processing speed) and emotion regulation problems (irritability, impulsivity, anxiety) that can make it difficult to override impulsive or aggressive reactions to perceived threat or provocation by other drivers (Amick et al., 2013; Classen et al., 2009; Classen et al., 2011; Contractor, Armour, Forbes, & Elhai, 2016; Lew et al., 2010; Lew et al., 2011; Wickens, Toplak, & Wiesenthal, 2008). The same deficits may also make it particularly challenging to inhibit overlearned combat driving behaviors and readjust to a less aggressive civilian style of driving (Hannold et al., 2013).
TBI and PTSD are highly comorbid in combat veterans, and there is evidence that the persistent “postconcussive” symptoms associated with TBI may be largely mediated by PTSD in those with both conditions (Hoge et al., 2008; Schneiderman, Braver, & Kang, 2008). Driving simulation studies have found that combat veterans perform more poorly than controls on a number of driving-related indices (Amick et al., 2013; Classen et al., 2011), and that PTSD may be associated with increases in driving errors (Amick et al., 2013). In one study of Iraq/Afghanistan era veterans seen in a VA outpatient polytrauma clinic where 93% of patients endorsed difficulties with driving in at least one domain (e.g. general driving difficulties, receipt of a warning or traffic citation, accidents, near misses, problems with anger or impatience, or becoming lost or disoriented), patients with PTSD (with or without TBI) reported the most significant driving impairments, while veterans with TBI alone did not differ from veterans without either diagnosis in the types of driving problems they experienced. Problems with anger or impatience, specifically, was endorsed by over 80% of veterans with PTSD, regardless of the presence of TBI (Lew et al., 2011).
The majority of research examining difficulties with aggressive driving or road rage among OEF/OIF veterans has been conducted in veterans who obtain healthcare through the Department of Veterans Affairs (VA) (Hannold et al., 2013; James, Strom, & Leskela, 2014; Kuhn et al., 2010; T. Strom et al., 2013; T. Q. Strom et al., 2012), a subset of the veteran population with the greatest and most complex mental health needs (CMS Alliance to Modernize Healthcare, 2015). In this study we sought to examine the association between combat exposure, TBI, PTSD, and perceived need to reduce aggressive driving or road rage in a large sample of OEF/OIF veterans that included both VA users and non-users. We hypothesized that (1) veterans using VA healthcare services would be more likely to report difficulties with road rage and (2) that PTSD would be associated with perceived need to cut down on aggressive driving in this population, regardless of the presence of TBI.
Method
Participants and Procedure
Approvals for the parent project for this study were obtained from the [edited out for blind review] Institutional Review Board and the U.S. Office of Management and Budget. Details of study methods have been published previously [edited out for blind review] and will be reviewed only briefly here. Measures for this study were completed as part of the OEF/OIF Veterans Health and Needs Study. This study surveyed a random sample of 5000 veterans who deployed in support of the wars in Iraq and Afghanistan, were eligible for VA care, and who had a last known residence within the Veterans Integrated Service Network 6 (VISN 6) catchment area (North Carolina, most of Virginia, and the southeastern corner of West Virginia). Potentially eligible participants were identified in collaboration with the Defense Manpower Data Center. A modified Dillman procedure was used, in which all participants received a 60-item survey package including an informed consent form. If needed, a follow-up letter and duplicate survey were sent. Of the 5000 veterans identified, 72 (1.4%) were determined to be ineligible (e.g., deceased or deployed) and 924 (18.5%) surveys were undeliverable (returned to sender). Of the 4004 surveys that were delivered, 1161 surveys were completed and returned, resulting in a cooperation rate of 29.0% (response rate of 23.6%).
Measures
Survey items assessed demographic characteristics and military history, including age, sex, race, marital status, employment status, military component and rank. “Road rage” was assessed via the following dichotomously scored item: “In the past year, have you felt you wanted or needed to cut down on aggressive driving or ‘road rage?’” Use of VA services for health care was assessed via the following item: “Since your last deployment, which, if any, have you used? Mark all that apply: used VA for health care services; used non-VA for health care services; have not used any health care services.” The Combat Experiences Scale (Hoge et al., 2004) was used to assess exposure to combat-related trauma. Participants indicated whether they had experienced 17 different combat situations during their deployment(s) such as “Handling or uncovering human remains”, “Participating in demeaning operations”, or “Had a buddy shot or hit who was near you.” Items endorsed were summed to index the total number of types of combat trauma experienced, ranging from 0–17.
PTSD symptom severity in the month prior to completing the survey was assessed using the 17-item PTSD Checklist (PCL) (Blanchard, Jones-Alexander, Buckley, & Forneris, 1996). Items on the PCL correspond to the diagnostic criteria for PTSD in the Diagnostic and Statistical Manual of Mental Disorders, 4th Edition, Text Revision. Total score is the sum of all items and can range from 17–85. Consistent with previous research, scores of 50 and above on the PCL were considered to reflect “probable PTSD” (Crawford et al., 2015; Forbes, Creamer, & Biddle, 2001; Hoge et al., 2008; Schry et al., 2015).
Potential TBI was coded as present if a participant indicated that he or she met both of the following criteria: 1) sustained an injury during deployment such as fragment wound, bullet wound, vehicle accident (tank, boat, plan, etc.), fall, blast/explosion (IED, RPG, land mine, grenade, etc.), physical training/sports, or other; and 2) the injury resulted in loss of consciousness as evidenced by “being dazed, confused, or seeing stars”; loss of consciousness for “less than 1 minute”, “1 to 20 minutes”, or “longer than 20 minutes”; or “not remembering the injury”. If both of these criteria were not met, the participant was coded as not having sustained a head injury.
Analyses
Participants were excluded iteratively from analysis if they were missing data necessary to calculate presence/absence of road rage (n=34 excluded), gender data (n=5 excluded), or more than 3 items on the PCL (n=20 excluded), reducing the total sample size for these analyses from 1161 to 1102. For participants missing 3 or fewer items on the PCL, the mean item rating for the symptom cluster of the missing item was imputed. For the remaining demographic and military variables included as covariates, multiple imputation with 10 iterations was used to impute missing data. Results from the pooled data are reported in this article.
Chi-square analyses were used to examine the differences on endorsement of road rage among the four possible TBI/PTSD participant groups: neither TBI nor PTSD; TBI without PTSD; PTSD without TBI; both TBI and PTSD. To test the hypothesis that veterans using VA healthcare services would be more likely to report difficulties with road rage, a logistic regression was used to model the univariate association between use of VA services and self-reported road rage. To evaluate the hypothesis that PTSD would be associated with self-reported road rage, regardless of the presence of TBI, a multivariate logistic regression modeled the presence of road rage as a factor of age, minority status (white vs. non-white), gender, martial status (married vs. unmarried), rank structure (officer vs. enlisted), number of types of combat traumas experience (0-17), and PTSD/TBI status (TBI only, PTSD only, or both TBI and PTSD; referent category=neither TBI nor PTSD).
Results
Demographic and clinical characteristics are reported in Table 1. A chi-square test of all four groups revealed a significant overall effect of group on likelihood of endorsing road rage (χ2=109.62, p<.0001). Post-hoc chi-square comparisons among the groups indicated that both groups with PTSD (regardless of TBI status) reported significantly (i.e. p<.05) higher rates of road rage when compared to the group with neither PTSD nor TBI, and when compared to the group with TBI only. The group with TBI only did not endorse significantly higher rates of road rage than the group with neither PTSD nor TBI (See Figure 1).
Table 1.
Demographic and Clinical Characteristics
| Variable | Mean (SD) or n (%) |
|---|---|
| Age (n=1099) a | 38.8 (9.8) |
| Male | 907 (82.5%) |
| Race | |
| African-American | 184 (16.7%) |
| White | 783 (71.3%) |
| Other race | 132 (12.0%) |
| Married (n=1090)a | 774 (71.0%) |
| Employment status (n=1101) a | |
| Active duty military or full time civilian | 725 (65.9%) |
| Part time civilian or student | 90 (8.2%) |
| Other | 286 (26.0%) |
| Military component (n=1071) a | |
| Active duty | 668 (62.4%) |
| Reserves/National Guard | 403 (37.6%) |
| Enlisted (vs. Officer) (n=1090) a | 808 (74.1%) |
| Used VA for health care since deployment (n=1062) a | 388 (36.5%) |
| Income < $30,000 per year (n=1085) a | 188 (17.3%) |
| # types combat trauma | 4.01 (4.03) |
| PTSD/TBI status | |
| neither | 877 (79.8%) |
| TBI, no PTSD | 69 (6.3%) |
| PTSD, no TBI | 96 (8.7%) |
| TBI and PTSD | 57 (5.2%) |
| Problem with road rage | 305 (27.8%) |
These variables had missing data and were imputed to create a full dataset for regression analyses. All other variables N = 1102.
Figure.
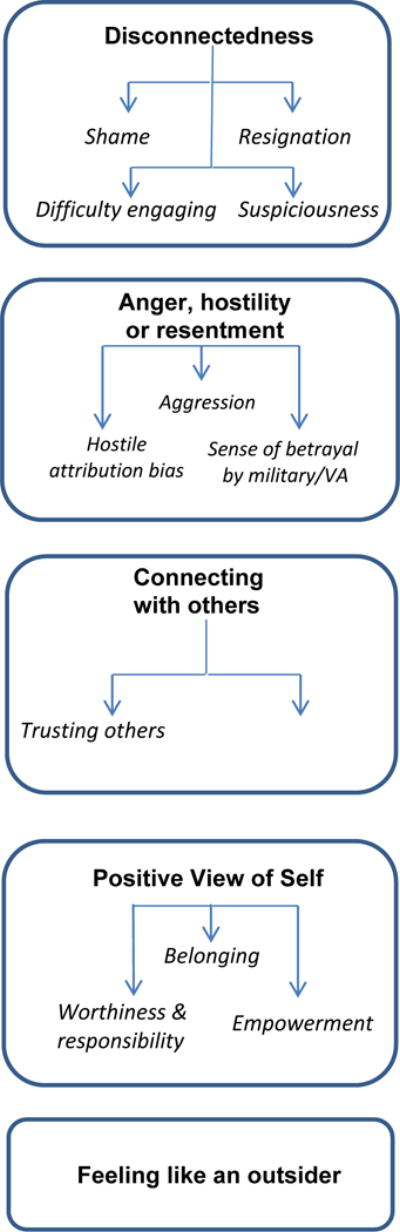
Themes and Subthemes
In the logistic regression modeling road rage as a factor of VA use only, veterans who reported using VA services since their last deployment were significantly more likely to report problems with self-reported aggressive driving or road rage (odds ratio [OR]=1.87, p<.0001) than veterans who did not report using VA services. In the multivariate logistic regression model, age (OR=0.98, p<.05), officer status (OR=0.57, p<.01), combat trauma (OR=1.09, p<.0001), PTSD without TBI (OR=3.63, p<.0001), and PTSD comorbid with TBI (OR=5.01, p<.0001) were significantly associated with road rage, whereas TBI without PTSD was not. Notably, use of VA services was no longer associated with road rage in the multivariate model (see Table 2). To examine whether the PCL cutoff score used to determine the presence of probable PTSD influenced the results of the regression, we re-ran the model with the threshold for PTSD at PCL≥40 and PCL≥60. The results were not changed substantially in either model.
Table 2.
Logistic regression Predicting “Road Rage” as a Factor of TBI/PTSD Status
| Variable | OR | 95% CI |
|---|---|---|
| Intercept | 0.44* | [0.22, 0.89] |
| Age | 0.98* | [0.96, 0.99] |
| Minority status (white=1, non-white=0) |
1.20 | [0.85, 1.71] |
| Gender (male=1, female=0) |
0.89 | [0.60, 1.32] |
| Marital status (married=1, not married=2) |
1.11 | [0.80, 1.54] |
| Officer | 0.57** | [0.39, 0.83] |
| Use of VA health care services (0=no use since last deployment, 1=use since last deployment) |
1.24 | [0.91, 1.68] |
| # types combat trauma | 1.09*** | [1.05, 1.13] |
| TBI, no PTSD | 1.22 | [0.70, 2.13] |
| PTSD, no TBI | 3.44*** | [2.14, 5.52] |
| TBI & PTSD | 4.71*** | [2.46, 9.00] |
Note: index is “no TBI”
p < .05
p < .01
p < .001
Discussion
In this sample of both VA and non-VA service-using veterans, we found that 56% of veterans with PTSD, and 70% of veterans with both PTSD and TBI, endorsed a recognized need to cut down on aggressive driving. In bivariate analyses, use of VA services was significantly associated with self-reported difficulty controlling aggressive driving or “road rage”; however, this association was no longer significant in the multivariate model, suggesting that observed differences in problems with aggressive driving between users and non-users of VA services were largely accounted for by demographic and clinical factors.
Veterans with PTSD, regardless of TBI status, reported road rage at significantly higher rates compared to veterans with TBI only, and compared to veterans with neither TBI nor PTSD. Veterans with TBI only did not differ from those with neither diagnosis in self-reported problems with road rage. From a clinical standpoint, this suggests that treatment of PTSD could benefit from assessment of aggressive driving and the inclusion of aggressive driving as an outcome in treatment plans. Interventions for road rage in veterans with PTSD (regardless of TBI status) might be strengthened by components that focus on motivational enhancement, target hostile interpretation biases (e.g. Hawkins & Cougle, 2013), or enhance emotional and physiological arousal regulation skills. A previous study of this cohort documented that 57% of veterans with probable PTSD reported at least one mental health contact in the prior 12-months, and 68% of those reporting any mental health contact indicated that services were obtained at a VA or Vet Center (Crawford et al., 2015). Outreach to the more than 40% of Veterans with probable PTSD is needed, as is additional research on whether PTSD treatment lowers risk of road rage/aggressive driving.
Apart from PTSD, TBI and exposure to combat trauma, officer status emerged as a significant (negative) predictor of aggressive driving in the multivariate model. Officer status has been found to be protective against both PTSD (Ramchand, Rudavsky, Grant, Tanielian, & Jaycox, 2015) and aggression (Gallaway, Fink, Millikan, & Bell, 2012) in previous work, with hypothesized mechanisms including older age, higher education, and lower combat exposure. Bivariate analyses in the current sample indicated that officer status was positively associated with age, but was not related to number of combat-related traumas. Enlisted status and exposure to combat trauma were significantly associated with increased odds of aggressive driving. This is consistent with previous findings that enlisted status and higher rates of deployment-related traumatic events are associated with higher levels of risky driving behavior and greater risk of involvement in motor vehicle accidents (Hoggatt et al., 2015; Woodall et al., 2014). As such, post-deployment education aimed at helping military personnel transition from battlemind-style aggressive driving behaviors to the more defensive approach appropriate to civilian settings may be warranted.
These findings extend previous work in at least two ways. First, the majority of prior research on aggressive driving in OEF/OIF veterans has been in users of VA healthcare (see Hwang et al., 2014, for an exception), a subset of veterans with the greatest and most complex mental health needs (CMS Alliance to Modernize Healthcare, 2015). Our sample extends these findings to include veterans who are not actively seeking healthcare through the VA, allowing us to demonstrate that while VA use is associated with increased road rage in bivariate analysis, this association does not hold when other relevant demographic and clinical factors are taken into consideration.
This study also adds to the literature on post-deployment driving problems by demonstrating that PTSD, regardless of TBI status, is associated specifically with aggressive driving. This may be important because aggressive driving appears to be unique among driving-related challenges in combat veterans. For example, Hannold et al (2013) found that OEF/OIF veterans sought to implement specific strategies to mitigate most of their driving-related difficulties, with the notable exception of aggressive driving. Individuals with PTSD have been found to be more likely to perceive threat and to attribute hostile intentions to perceived provocation by others (Dodge, Bates, & Pettit, 1990; Taft et al., 2015), and PTSD-related aggression has been found to be largely impulsive in nature (Heinz, Makin-Byrd, Blonigen, Reilly, & Timko, 2015; Miles, Menefee, Wanner, Teten Tharp, & Kent, 2015; Teten et al., 2010) and associated with symptoms of hyperarousal (Kachadourian et al., 2013; Pavic et al., 2003). In the context of driving, then, veterans with PTSD may be more likely to perceive threat and to attribute hostile intent to other drivers, diminishing their motivation to inhibit impulsive aggressive responses for which they are already physiologically primed.
Study Limitations & Conclusion
The present study has several limitations that should be considered when interpreting these findings. The primary limitation is that the outcome variable of road rage was assessed with a single self-report item: “In the past year, have you felt you wanted or needed to cut down on aggressive driving or ‘road rage?’” While the definition of aggressive driving or road rage may be somewhat intuitive, a more clearly operationalized definition of the construct would help improve confidence that what is being measured is a specific set of behaviors, rather than a mixture of behavior and insight. Kuhn et al (2010), for example, specified angry hand gestures, tailgating, cutting off other drivers, chasing other drivers, or intentionally driving into another object as aggressive driving. As the research in this area evolves, more clearly operationalized definitions of aggressive driving and road rage will become increasingly necessary.
Self-report checklists were also used to evaluate for the presence of PTSD and TBI. The limitation of our checklist for TBI may have particularly important implications for the interpretation of our findings because the items did not allow us to make any determination about severity or frequency head injuries. We also did not assess length of time since the most recent head injury, a potentially important data point given that the majority of post-concussive symptoms remit in mild TBI after about three months at least for non-repetitive head injuries (Karr, Areshenkoff, & Garcia-Barrera, 2014). An additional limitation concerns the cross-sectional design of the study, which does not allow us to determine whether problems with aggressive driving existed prior to deployment or the onset of PTSD and/or TBI. Keeping these limitations in mind, the present findings suggest that PTSD increases returning veterans’ risk of aggressive driving, regardless of TBI status. These data add to the growing literature indicating that PTSD may be a critical factor in the increased risk for MVA-related injury and death faced by combat veterans when they return home from service in a war zone.
Impact.
The findings of this study suggest that PTSD increases returning veterans’ risk of aggressive driving, regardless of TBI status. These data add to the growing literature indicating that PTSD may be a critical factor in the increased risk for MVA-related injury and death faced by combat veterans when they return home from service in a war zone.
From a clinical standpoint, this suggests that treatment of PTSD in combat veterans could benefit from assessment of aggressive driving, and the inclusion of aggressive driving as an outcome in treatment plans.
Our findings may also suggest that post-deployment education aimed at helping military personnel transition from combat-style aggressive driving behaviors to the more defensive approach appropriate to civilian settings may be warranted.
Acknowledgments
This project was supported in part by the Department of Veterans Affairs’ (VA) Mid-Atlantic Mental Illness Research, Education and Clinical Center (MIRECC) of the VA Office of Mental Health Services, the VA VISN 6 Mid-Atlantic Healthcare Network, and the Research and Development and Mental Health Services of the Durham VA Medical Center. Dr. Van Voorhees was supported by Career Development Awards #5IK2RX001298 from the Rehabilitation Research and Development (RR&D) of the VA Office of Research and Development (ORD). Drs. Kimbrel and Dedert were supported by Career Development Awards #IK2CX000525 and #IK2CX000718, respectively, from the Clinical Science Research and Development (CSR&D) Service of the VA Office of Research and Development (ORD). VA CSR&D and RR&D played no role in study design, data collection, data analysis, manuscript preparation, or the decision to submit this article for publication. We would like to thank the anonymous peer reviewers of our work for their insights and suggestions on the initial draft; we believe their comments improved the presentation of our findings enormously. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the VA or the United States government.
Footnotes
Rates of TBI, for example, have been reported to be as high as 15% in veterans of the Iraq War (Hoge et al., 2008), and rates of PTSD have been found to be close to 16% of veterans who were deployed to Iraq or Afghanistan (Dursa, Reinhard, Barth, & Schneiderman, 2014).
References
- Amick MM, Kraft M, McGlinchey R. Driving simulator performance of veterans from the Iraq and Afghanistan wars. Journal of Rehabilitation Research and Development. 2013;50(4):463–470. doi: 10.1682/jrrd.2012.06.0108. [DOI] [PubMed] [Google Scholar]
- Blanchard EB, Jones-Alexander J, Buckley TC, Forneris CA. Psychometric properties of the PTSD Checklist (PCL) Behaviour Research and Therapy. 1996;34(8):669–673. doi: 10.1016/0005-7967(96)00033-2. doi:0005-7967(96)00033-2. [DOI] [PubMed] [Google Scholar]
- Classen S, Levy C, McCarthy D, Mann WC, Lanford DN, Waid-Ebbs JK. Traumatic Brain Injury and Driving Assessment: An Evidence-Based Literature Review. American Journal of Occupational Therapy. 2009;63(5):580–591. doi: 10.5014/ajot.63.5.580. [DOI] [PubMed] [Google Scholar]
- Classen S, Levy C, Meyer DL, Bewernitz M, Lanford DN, Mann WC. Simulated driving performance of combat veterans with mild tramatic brain injury and posttraumatic stress disorder: a pilot study. American Journal of Occupational Therapy. 2011;65(4):419–427. doi: 10.5014/ajot.2011.000893. [DOI] [PubMed] [Google Scholar]
- CMS Alliance to Modernize Health Care. Independent Assessment of the Health Care Delivery Systems and Management Processes of the Department of Veterans Affairs. Integrated Report 2015;1 [Google Scholar]
- Contractor AA, Armour C, Forbes D, Elhai JD. Posttraumatic Stress Disorder’s Underlying Dimensions and Their Relation With Impulsivity Facets. Journal of Nervous and Mental Disease. 2016;204(1):20–25. doi: 10.1097/NMD.0000000000000417. [DOI] [PubMed] [Google Scholar]
- Crawford EF, Elbogen EB, Wagner HR, Kudler H, Calhoun PS, Brancu M, Straits-Troster KA. Surveying treatment preferences in U.S. Iraq-Afghanistan Veterans with PTSD symptoms: a step toward veteran-centered care. Journal of Traumatic Stress. 2015;28(2):118–126. doi: 10.1002/jts.21993. [DOI] [PubMed] [Google Scholar]
- Dodge KA, Bates JE, Pettit GS. Mechanisms in the cycle of violence. Science. 1990;250(4988):1678–1683. doi: 10.1126/science.2270481. [DOI] [PubMed] [Google Scholar]
- Dursa EK, Reinhard MJ, Barth SK, Schneiderman AI. Prevalence of a positive screen for PTSD among OEF/OIF and OEF/OIF-era veterans in a large population-based cohort. Journal of Traumatic Stress. 2014;27(5):542–549. doi: 10.1002/jts.21956. [DOI] [PubMed] [Google Scholar]
- Forbes D, Creamer M, Biddle D. The validity of the PTSD checklist as a measure of symptomatic change in combat-related PTSD. Behaviour Research and Therapy. 2001;39(8):977–986. doi: 10.1016/s0005-7967(00)00084-x. http://dx.doi.org/10.1016/S0005-7967(00)00084-X. [DOI] [PubMed] [Google Scholar]
- Gallaway MS, Fink DS, Millikan AM, Bell MR. Factors associated with physical aggression among US Army soldiers. Aggress Behav. 2012;38(5):357–367. doi: 10.1002/ab.21436. [DOI] [PubMed] [Google Scholar]
- Hannold EM, Classen S, Winter S, Lanford DN, Levy CE. Exploratory pilot study of driving perceptions among OIF/OEF Veterans with mTBI and PTSD. Journal of Rehabilitation Research and Development. 2013;50(10):1315–1330. doi: 10.1682/jrrd.2013.04.0084. [DOI] [PubMed] [Google Scholar]
- Hawkins KA, Cougle JR. Effects of interpretation training on hostile attribution bias and reactivity to interpersonal insult. Behavior Therapy. 2013;44(3):479–488. doi: 10.1016/j.beth.2013.04.005. [DOI] [PubMed] [Google Scholar]
- Heinz AJ, Makin-Byrd K, Blonigen DM, Reilly P, Timko C. Aggressive behavior among military veterans in substance use disorder treatment: the roles of posttraumatic stress and impulsivity. Journal of Substance Abuse Treatment. 2015;50:59–66. doi: 10.1016/j.jsat.2014.10.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoge CW, Castro CA, Messer SC, McGurk D, Cotting DI, Koffman RL. Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. New England Journal of Medicine. 2004;351(1):13–22. doi: 10.1056/NEJMoa040603. [DOI] [PubMed] [Google Scholar]
- Hoge CW, McGurk D, Thomas JL, Cox AL, Engel CC, Castro CA. Mild traumatic brain injury in U.S. Soldiers returning from Iraq. New England Journal of Medicine. 2008;358(5):453–463. doi: 10.1056/NEJMoa072972. doi:NEJMoa072972. [DOI] [PubMed] [Google Scholar]
- Hoggatt KJ, Prescott MR, Goldmann E, Tamburrino M, Calabrese JR, Liberzon I, Galea S. The prevalence and correlates of risky driving behavior among National Guard soldiers. Traffic Inj Prev. 2015;16(1):17–23. doi: 10.1080/15389588.2014.896994. [DOI] [PubMed] [Google Scholar]
- Hwang EJ, Peyton CG, Kim DK, Nakama-Sato KK, Noble AE. Postdeployment Driving Stress and Related Occupational Limitations Among Veterans of Operation Iraqi Freedom and Operation Enduring Freedom. American Journal of Occupational Therapy. 2014;68(4):386–394. doi: 10.5014/ajot.2014.011668. [DOI] [PubMed] [Google Scholar]
- Ilie G, Mann RE, Ialomiteanu A, Adlaf EM, Hamilton H, Wickens CM, Cusimano MD. Traumatic brain injury, driver aggression and motor vehicle collisions in Canadian adults. Accident Analysis and Prevention. 2015;81:1–7. doi: 10.1016/j.aap.2015.04.021. http://dx.doi.org/10.1016/j.aap.2015.04.021. [DOI] [PubMed] [Google Scholar]
- James LM, Strom TQ, Leskela J. Risk-taking behaviors and impulsivity among veterans with and without PTSD and mild TBI. Military Medicine. 2014;179(4):357–363. doi: 10.7205/MILMED-D-13-00241. [DOI] [PubMed] [Google Scholar]
- Kachadourian LK, Taft CT, Holowka DW, Woodward H, Marx BP, Burns A. Maladaptive dependency schemas, posttraumatic stress hyperarousal symptoms, and intimate partner aggression perpetration. Journal of Traumatic Stress. 2013;26(5):580–587. doi: 10.1002/jts.21850. [DOI] [PubMed] [Google Scholar]
- Karr JE, Areshenkoff CN, Garcia-Barrera MA. The neuropsychological outcomes of concussion: a systematic review of meta-analyses on the cognitive sequelae of mild traumatic brain injury. Neuropsychology. 2014;28(3):321–336. doi: 10.1037/neu0000037. [DOI] [PubMed] [Google Scholar]
- Krahl PL, Jankosky CJ, Thomas RJ, Hooper TI. Systematic review of military motor vehicle crash-related injuries. American Journal of Preventive Medicine. 2010;38(1 Suppl):S189–196. doi: 10.1016/j.amepre.2009.10.024. [DOI] [PubMed] [Google Scholar]
- Kuhn E, Drescher K, Ruzek J, Rosen C. Aggressive and unsafe driving in male veterans receiving residential treatment for PTSD. Journal of Traumatic Stress. 2010;23(3):399–402. doi: 10.1002/jts.20536. [DOI] [PubMed] [Google Scholar]
- Lew HL, Amick MM, Kraft M, Stein MB, Cifu DX. Potential driving issues in combat returnees. NeuroRehabilitation. 2010;26(3):271–278. doi: 10.3233/NRE-2010-0562. [DOI] [PubMed] [Google Scholar]
- Lew HL, Kraft M, Pogoda TK, Amick MM, Woods P, Cifu DX. Prevalence and characteristics of driving difficulties in Operation Iraqi Freedom/Operation Enduring Freedom combat returnees. Journal of Rehabilitation Research and Development. 2011;48(8):913–925. doi: 10.1682/jrrd.2010.08.0140. [DOI] [PubMed] [Google Scholar]
- Lincoln AE, Hooper TI, Kang HK, Debakey SF, Cowan DN, Gackstetter GD. Motor vehicle fatalities among Gulf War era veterans: characteristics, mechanisms, and circumstances. Traffic Inj Prev. 2006;7(1):31–37. doi: 10.1080/15389580500412028. [DOI] [PubMed] [Google Scholar]
- Miles SR, Menefee DS, Wanner J, Teten Tharp A, Kent TA. The Relationship Between Emotion Dysregulation and Impulsive Aggression in Veterans With Posttraumatic Stress Disorder Symptoms. J Interpers Violence. 2015 doi: 10.1177/0886260515570746. [DOI] [PubMed] [Google Scholar]
- Pavic L, Gregurek R, Petrovic R, Petrovic D, Varda R, Vukusic H, Crnkovic-Markovic S. Alterations in brain activation in posttraumatic stress disorder patients with severe hyperarousal symptoms and impulsive aggressiveness. European Archives of Psychiatry and Clinical Neuroscience. 2003;253(2):80–83. doi: 10.1007/s00406-003-0411-z. [DOI] [PubMed] [Google Scholar]
- Ramchand R, Rudavsky R, Grant S, Tanielian T, Jaycox L. Prevalence of, risk factors for, and consequences of posttraumatic stress disorder and other mental health problems in military populations deployed to Iraq and Afghanistan. Curr Psychiatry Rep. 2015;17(5):37. doi: 10.1007/s11920-015-0575-z. [DOI] [PubMed] [Google Scholar]
- Schneiderman A, Braver E, Kang H. Understanding sequelae of injury mechanisms and mild traumatic brain injury incurred during the conflicts in Iraq and Afghanistan: persistent postconcussive symptoms and posttraumatic stress disorder. American Journal of Epidemiology. 2008;167(12):1446–1452. doi: 10.1093/aje/kwn068. doi:kwn068. [DOI] [PubMed] [Google Scholar]
- Schry AR, Rissling MB, Gentes EL, Beckham JC, Kudler HS, Straits-Tröster K, Calhoun PS. The Relationship Between Posttraumatic Stress Symptoms and Physical Health in a Survey of U.S. Veterans of the Iraq and Afghanistan Era. Psychosomatics. 2015;56(6):674–684. doi: 10.1016/j.psym.2015.07.010. http://dx.doi.org/10.1016/j.psym.2015.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strom T, Leskela J, Possis E, Thuras P, Leuty ME, Doane BM, Rosenzweig L. Cognitive-behavioral group treatment for driving-related anger, aggression, and risky driving in combat veterans: a pilot study. Journal of Traumatic Stress. 2013;26(3):405–408. doi: 10.1002/jts.21808. [DOI] [PubMed] [Google Scholar]
- Strom TQ, Leskela J, James LM, Thuras PD, Voller E, Weigel R, Holz KB. An exploratory examination of risk-taking behavior and PTSD symptom severity in a veteran sample. Military Medicine. 2012;177(4):390–396. doi: 10.7205/milmed-d-11-00133. [DOI] [PubMed] [Google Scholar]
- Taft CT, Weatherill RP, Scott JP, Thomas SA, Kang HK, Eckhardt CI. Social Information Processing in Anger Expression and Partner Violence in Returning U.S. Veterans. Journal of Traumatic Stress. 2015;28(4):314–321. doi: 10.1002/jts.22017. [DOI] [PubMed] [Google Scholar]
- Teten AL, Schumacher JA, Taft CT, Stanley MA, Kent TA, Bailey SD, White DL. Intimate partner aggression perpetrated and sustained by male Afghanistan, Iraq, and Vietnam veterans with and without posttraumatic stress disorder. J Interpers Violence. 2010;25(9):1612–1630. doi: 10.1177/0886260509354583. doi:0886260509354583. [DOI] [PubMed] [Google Scholar]
- United States Automobile Association. Returning warriors drivingsafety report 2012. 2012 Retrieved from https://content.usaa.com/mcontent/static_assets/Media/Returning_Warriors_report_summary.pdf.
- Wickens CM, Toplak ME, Wiesenthal DL. Cognitive failures as predictors of driving errors, lapses, and violations. Accident Analysis and Prevention. 2008;40(3):1223–1233. doi: 10.1016/j.aap.2008.01.006. http://dx.doi.org/10.1016/j.aap.2008.01.006. [DOI] [PubMed] [Google Scholar]
- Woodall KA, Jacobson IG, Crum-Cianflone NF. Deployment experiences and motor vehicle crashes among U.S. service members. American Journal of Preventive Medicine. 2014;46(4):350–358. doi: 10.1016/j.amepre.2013.11.015. [DOI] [PubMed] [Google Scholar]
- Zhang T, Chan AH. The association between driving anger and driving outcomes: A meta-analysis of evidence from the past twenty years. Accident Analysis and Prevention. 2016;90:50–62. doi: 10.1016/j.aap.2016.02.009. [DOI] [PubMed] [Google Scholar]


