Abstract
Abstract African immigrants living in the United States are disproportionately and uniquely affected by HIV. Evidence shows that stigma may contribute to this inequity. Applying a biopsychosocial model of health, our qualitative study explored HIV-related stigma and its impact on African immigrants living with HIV in a large northwest U.S. metropolitan area. We conducted in-depth, semi-structured interviews with 20 African immigrants living with HIV. In the biological health realm, HIV-related stigma contributed to adverse health care environments, disruptions in care, and poor physical health. In the psychological health realm, it was associated with emotional vulnerability, depressive symptoms, and negative coping. In the social health realm, stigma lead to disclosure challenges, isolation, and poor social support. HIV-related stigma was an extensive and pervasive burden for this population. The biopsychosocial model was a helpful lens through which to explore HIV-related stigma and identify opportunities for future research and intervention.
Keywords: African immigrant, biopsychosocial, HIV, mental health, stigma
In the United States, African immigrants are disproportionately and uniquely affected by HIV. African immigrants have an HIV diagnosis rate estimated at 6 times the incidence in the general U.S. population (Blanas et al., 2013). Compared to other groups of people living with HIV (PLWH) in the United States, African immigrant PLWH have higher rates of diagnosis among women, higher rates of heterosexual transmission, and lower rates of transmission from injection drug use (Johnson, Hu, & Dean, 2010). These trends are similar to trends in sub-Saharan Africa, where heterosexual sex and perinatal transmission are the primary modes of transmission, and women account for 58% of PLWH (Kharsany & Karim, 2016). Furthermore, while immigrants from Africa represent numerous distinct countries, cultures, and communities, they are all vulnerable to immigration-related challenges including discrimination, racism, language barriers, lack of legal documentation, fear of termination from employment, unfamiliarity with the U.S. health care system, and a preference for spiritual or alternative care (American Psychological Association, Presidential Task Force on Immigration, 2012). Previous research has indicated that these factors may reduce the willingness and/or ability of African immigrants to utilize available HIV resources (Othieno, 2007).
HIV-related stigma is another significant issue for PLWH. Stigma has been defined as public perceptions about persons with an undesirable health condition (Scambler, 2009; e.g., HIV, mental illness) or social identity (Goffman, 1963; e.g., immigrant, indigent), resulting in stereotypes, prejudice, and discrimination. Stigma can be social, through overt behaviors of others, or internalized (also known as self-stigma), by incorporating negative stereotypes into one’s sense of self (Van Brakel, 2006). Both forms of stigma have demonstrated negative implications for physical, psychological, and social outcomes (Link & Phelan, 2006). A small, but growing body of research has described HIV-related stigma in African immigrant PLWH in the United States as a unique and culturally-specific barrier to care (Foley, 2005; Koku, 2010; Ojikutu et al., 2013; Othieno, 2007). However, there remains a need for a conceptual framework to comprehensively assess and understand how HIV-related stigma manifests in African immigrant PLWH and the distinct mechanisms by which it impacts overall health and wellbeing.
The biopsychosocial model of health (Engel, 1977) may be a useful framework for understanding the impact of HIV-related stigma on a PLWH’s life. Specifically, the biopsychosocial model underlines the idea that when a disease or disorder is present, a person suffers as a whole, in context, not merely in an isolated organ. This well-established model includes not only the physical health perspective of the biomedical lens, but also incorporates a person’s psychological/emotional experiences, socio-cultural context, and related behaviors into a comprehensive view of health and illness (Havelka, Lučanin, & Lučanin, 2009). Although the biopsychosocial model originated in the field of psychiatry, it has been used extensively in myriad settings, including clinical applications, treatment guidelines, and rehabilitation and disability research, and forms the basis for validated case complexity measures and the World Health Organization’s International Classification of Functioning, Disability, and Health (Wade & Halligan, 2017). It is also a foundational component of patient-centered care (Smith, Fortin, Dwamena, & Frankel, 2013). In terms of HIV research, the biopsychosocial model has been used in studies on disclosure among gay men (Flowers & Davis, 2013) and parents who have HIV (Letteney, Krauss, & Kaplan, 2012), HIV-related chronic pain (Merlin et al., 2014), and aging with HIV (Vance & Robinson, 2004).
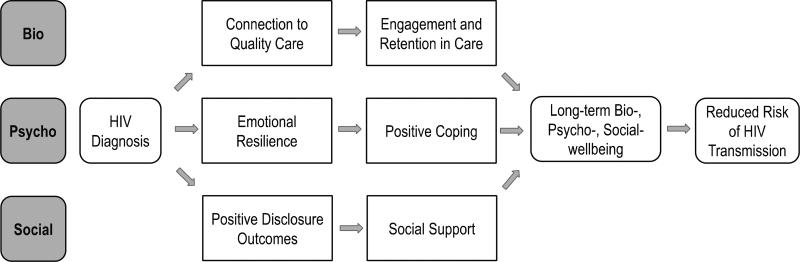
Figure 1 represents an ideal scenario for someone receiving an HIV diagnosis. Under the biopsychosocial model, this individual would (a) be connected to competent and compassionate clinical care (bio); (b) possess the resilience and coping skills to manage the emotional effects of receiving an HIV diagnosis (psycho); and (c) have supportive friends and family with whom to share the diagnosis (social). These positive biopsychosocial resources would then lead to long-term well-being, including a reduced risk of disease transmission.
Figure 1.
Biopsychosocial model of HIV Care
In this study, we explore how African immigrant PLWH in a large northwest U.S. metropolitan area experience HIV-related stigma, and the subsequent effects on their biopsychosocial health.
Methods
Study Design and Sample
For this exploratory qualitative study, we conducted semi-structured individual interviews with African immigrant PLWH in 2013–2014. We recruited participants from a public hospital-based clinic and a local peer-led community-based organization (CBO) that provided psychosocial support services (case management and support groups) to PLWH in a large northwest U.S. metropolitan area. Eligible participants were English-speaking immigrants from any African country, ages 18 years or older, receiving outpatient HIV treatment services, and able to give informed consent. At the clinic, a nurse with access to a research registry contacted eligible patients who had pre-consented to participate in studies. At the CBO, a peer counselor contacted eligible clients in person and via telephone. Respondents who were interested then met with a research coordinator who obtained informed consent and conducted in-person interviews. Based on prior research experience with this population, we determined that 20 interviews would be sufficient to achieve thematic saturation. All study procedures were approved by the University of Washington Institutional Review Board.
Data Collection
We collected socio-demographic information including sex, age, country of origin, education level, religion, marital status, living arrangements, number of years in the United States, and number of years living with HIV. A semi-structured interview guide of general questions and probes was used to explore related stigma, stress/mood (more neutral terminology we used to assess depression), engagement in care, and health-related behaviors.
Each participant took part in an individual interview that lasted approximately 1 hour and was held at a time and private location convenient to the participant. All but one participant consented to audio-recordings of their interviews. Detailed field notes were taken to document that participant’s responses.
Data Analysis
Audio data were transcribed verbatim by an independent third-party service. Using thematic analysis, such that themes related to the research question emerged from the data and were not determined a priori (Braun & Clarke, 2006), an experienced, masters level researcher (who was not an interviewer) initiated and coordinated data analysis using the qualitative coding software program, ATLAS.ti (Muhr, 1991). She reviewed the transcripts and inductively open-coded for key recurring concepts and themes, and organized the data into a codebook using matrices to assist with theme identification (Miles & Huberman, 1994). The secondary analyst (who was also the primary interviewer) then used that codebook to independently and deductively code the transcripts. The two analysts met several times to refine code definitions based on interrelationships between themes and discrepancies. Emerging themes were then overlaid onto the biopsychosocial model to organize and illustrate our findings.
Results
We interviewed 20 (8 from the clinic, 12 from the CBO) African immigrant PLWH who were receiving care in a large northwest U.S. metropolitan area. Participant socio-demographic information can be found in Table 1. The mean age of the group was 42.5 years (range = 25–58 years), and the majority (80%) reported having education beyond high school. Participants represented nine countries of origin from West, North, and East Africa, with a majority from East African countries. The median lengths of time living in the United States and since HIV diagnosis were 11.9 and 11 years, respectively.
Table 1.
Demographic Characteristics of African Immigrant Participants (N = 20)
| Characteristic (Categorical) | Frequency (%) |
|---|---|
| Gender | |
| • Male | 7 (35) |
| • Female | 13 (65) |
| Education Level | |
| • Less than 12th grade | 2 (10) |
| • 12th grade or equivalent | 2 (10) |
| • Some college | 7 (35) |
| • College graduate | 9 (45) |
| Marital Status | |
| • Legally married | 8 (40) |
| • Cohabiting | 1 (5) |
| • Unmarried/single | 3 (15) |
| • Separated/divorced | 5 (25) |
| • Widowed | 3 (15) |
| Living Arrangement | |
| • Alone | 2 (10) |
| • With other adults; no dependents | 9 (45) |
| • With other adults and dependents | 5 (25) |
| • With dependants only | 4 (20) |
| Religion | |
| • Christian | 16 (80) |
| • Muslim | 3 (15) |
| • Other | 1 (5) |
| Characteristic (Continuous) | Mean (range) |
| • Age | 42.5 (25–58) |
| Median (range) | |
| • Number of years living with HIV | 11 (1–19) |
| • Number of years living in the United Statesa | 11.9 (0.08–27.61) |
Data only available for 15 participants
Qualitative Themes
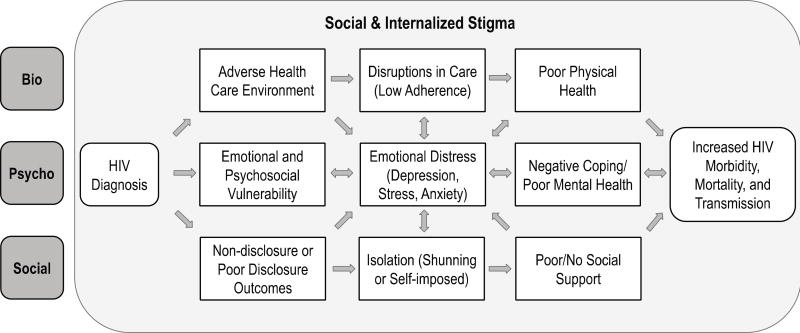
Figure 2 displays the biopsychosocial model adapted to illustrate our thematic findings and visually demonstrate the complex ways stigma operates to interrupt optimal health across the biological, psychological, and social realms.
Figure 2.
Biopsychosocial model of HIV Care within the context of stigma
Social and Internalized Stigma
HIV-related stigma was identified as a significant issue by all participants. Descriptions of experiences with stigma were extensive and diverse, with social stigma appearing as a predominant theme. Participants shared personal experiences of being shamed, ignored, or shunned from the community. Furthermore, there was consensus among participants that HIV-related stigma was distinct in tight-knit African immigrant communities. Many attributed this to “African culture,” as exemplified by this participant who described the challenge of living with HIV in her community: “Our family, they don’t accept us; our society, they don’t accept us.”
Among the small number of participants who reported no personal experiences with social stigma, all described witnessing stigma in the community or in their families. One woman quoted her father’s response to her sister’s HIV diagnosis: “She brought this on her own, so let her just die.”
A majority of participants also related to the concept of internalized stigma. They reported feelings of self-blame, shame, and guilt. They also worried about sharing personal items or interacting with loved ones. One mother explained stigma’s impact on her relationship with her child: “I don’t want to be so close to this baby, so that I don’t get too attached… So apart from even people stigmatizing me, I stigmatize myself.”
Biopsychosocial Realm I: Biological Health
Adverse health care environment
In the biological health realm, many participants expressed how stigma made them uneasy in the health care environment and many reported discriminatory interactions with health care providers. One participant described receiving his diagnosis: “When he told me my [HIV] results, he just said, ‘Well, you have about 15 years to live, and you need to find another doctor because I don’t deal with HIV.’”
Participants also expressed concern about being seen in an HIV-specific clinical setting by others from the community. For many, knowing someone who worked in, or received treatment from, the same HIV primary care clinic had resulted in unconsented disclosure: “Someone [from my community] was working in the medical field… and they told my brother’s girlfriend that they saw my name and that I was HIV positive.”
Disruptions in care
In many cases, such adverse experiences contributed to disruptions in care and treatment adherence. Specifically, because of fears of discrimination and lack of confidentiality, participants were reluctant to speak honestly with health care providers, return to clinic appointments, or pick up medications: “The clinicians that are there, some of them come from the same village I come from…. Sometimes when I go to take my HIV medication… I miss my appointment that day because I don’t want them to see me.”
Poor physical health
Finally, a few participants noted that disruptions in care and adherence due to fear of negative experiences in the health setting could result in serious repercussions for health and life expectancy: “People are dying because of discrimination because they’re scared of that. They don’t want to get treated.”
Biopsychosocial Realm II: Psychological Health
Emotional vulnerability
In the psychological realm, participants reflected on ways in which stigma increased emotional vulnerability:
I’m fearful of people coming near me. I’m fearful they will find my medication. People know I’m fearful of something but they don’t know what… I’m always watching my back… You are always hiding. It’s the worst way to live.
Depression, stress, anxiety
The emotional distress described by participants primarily fell into the categories of depression, stress, and anxiety. References to depressive symptoms were the most prevalent, with many participants describing feeling “worthless” and not “want[ing] to live anymore.” Furthermore, the burden of these depressive symptoms was exacerbated by stigma related to mental illness. Participants commonly noted that, “depression is not very talked about in the African community.”
Many participants made direct links between depressive symptoms and disruptions in HIV care: “Depression can waste your health and make [a] difference for your HIV treatment. I missed my medication. I called out on my appointments so many times. That's part of depression right there.”
Heightened levels of stress and anxiety, especially related to health concerns, were also frequently reported: “So any small thing, oh, I think it’s HIV-related. I think I’m going; I’m dying. Any small thing that you didn’t even worry about [before] now is worrying you.”
Negative coping
Participants noted that limited support, low levels of emotional resilience, and/or lack of positive coping skills could reduce the ability to manage distress. Some described resorting to unhealthy behaviors such as denial or seeking escape: “Things that make me unhappy are the things that make me feel good. Smoking cigarettes. When I'm smoking I feel good about it. I'm drinking, I feel good. When I'm done and think about it, I feel bad again.”
Biopsychosocial Realm III: Social Health
Non-disclosure or poor disclosure outcomes
In the social realm, participants articulated significant concerns about disclosing their HIV status. Several participants described experiencing or witnessing painful, negative responses to disclosure. As a result, many participants reported not disclosing to anyone aside from their health care providers. One participant connected the reluctance to disclose to perceptions of HIV in the African immigrant community: “That’s why, even my family, I don’t tell them, because back home in Africa, if I told them I’m HIV [positive], they’re going to think I’m dead already.”
Isolation
Participants also described how they or people they knew had been shunned or “cut off” by friends and family due to stigma related to their disease:
I had my auntie who was HIV [positive], and when the family knew about it, everybody just kind of left her alone. She would come in, and people would walk out. If she would drink in a cup, then that cup would be thrown away. So, it was that kind of isolation that I don’t want to experience on myself.
Poor social support
Related to isolation, many participants acknowledged that not telling anyone about their disease left them unsupported with their worries, sadness, and distress. “There’s very few people you can talk to” was a common sentiment among participants. The desire to keep their HIV status a secret resulted in several participants avoiding social interaction, thus limiting the ability to develop a support network. “This is the fourth year I’ve not socialized with other people really, especially from the community,” explained one participant. Others explained that after the HIV diagnosis, they no longer sought romantic partners: “I don’t date. I never dated. The day I knew is the day I quit.”
Increased HIV Morbidity, Mortality, and Transmission
Responses from participants indicated that the biopsychosocial effects of HIV-related stigma resulted in poor disease outcomes. Many participants expressed a form of fatalism leading to low treatment adherence: “If you have HIV, you think you’re dying tomorrow, that’s it. [You] don’t even think about medication as useful.” Additionally, some participants described failing to take precaution to prevent transmission, expressing sentiments of, “Well, I already have [HIV], so why use a condom? …. You just want to feel good about yourself, you forget about the other person.” Another participant explained how non-disclosure and isolation had deleterious health impacts:
I think if I don’t tell anybody and if I don’t deal with it, then nobody will know. But most people I know who have done that have died, because then they don’t get the medication they need, and they end up with irreversible infections.
Discussion
Our findings highlight the pervasive and extensive burden of HIV-related stigma on African immigrant PLWH in a large northwest U.S. metropolitan area. HIV-related stigma is a known barrier to treatment adherence among PLWH (Katz et al., 2013), but the unique context in which this population experiences stigma necessitates a comprehensive approach to understanding how it influences all facets of health. In a recent article about women living with HIV in India, Short and Vissandjée (2017) assert that Engel’s biopsychosocial model was well-positioned to assess HIV-related stigma because stigma was manifest in all aspects of one’s life. Our findings support this assertion. Our adaptation of the biopsychosocial model of health in the context of HIV-related stigma, as depicted in Figure 2, provides a holistic approach for examining the diverse and culturally-contextualized threats that stigma poses to African immigrant PLWH’s physical, emotional, and social health.
In the biological health realm, our findings demonstrated how HIV-related stigma could create adverse health care environments that contributed to disruptions in care and subsequent poor physical health. Similar to a study of African immigrant women living with HIV in Philadelphia (Foley, 2005), our participants expended a substantial amount of time and energy attempting to keep their HIV status hidden and to avoid unintentional disclosure in the health care setting. Indeed, experiencing a negative encounter with health care personnel or fear of inadvertent disclosure deterred some participants from returning to the health care setting at all. Research has shown that stigma in the clinical setting is a threat to engagement in care (Valdiserri, 2002); however, as alluded to by certain participants, this threat may be magnified in smaller, tight-knit African immigrant communities. As such, health care settings that serve this population may benefit from targeted stigma interventions to increase and sustain clinical engagement. A number of stigma reduction strategies and tools are available for implementation at individual, environmental, and policy levels (Nyblade, Stangl, Weiss, & Ashburn, 2009).
In the psychological health realm, descriptions of stress, fear, anxiety, and depression were prevalent throughout the interviews. Our findings were consistent with previous research associating HIV-related stigma to depressive symptoms (Mitzel et al., 2015). In addition to depressive symptoms, our participants described negative coping, including substance use. Depression and substance abuse are the two most common psychiatric disorders in PLWH (Rabkin, 2008). Many participants noted that mental illness was also stigmatized in African immigrant communities. Correspondingly, research has shown that immigrant women suffering from depression were less likely to access mental health services than U.S.-born White women with depressive symptoms (Nadeem et al., 2007). The dual burden of mental illness and HIV-related stigma is concerning and represents an important focus for interventions targeted at African immigrant PLWH. Primary care and mental health providers in HIV clinics could explore creative and culturally aligned ways to integrate depression treatment when indicated. Practical cognitive behavioral interventions have demonstrated a cross-cultural application to address depression and may be a promising option (American Psychological Association, Presidential Task Force on Immigration, 2013).
Finally, in the social heath realm, similar to other research with African immigrant PLWH (Stutterheim et al., 2012), our study found that poor disclosure outcomes, isolation, and inadequate social support were common in this population. In our study, avoiding disclosure contributed to isolation and poor social support, both of which have been linked to lower engagement in care (Remien et al., 2015). As we saw in the biological realm, efforts to conceal one’s HIV status could also decrease engagement in care, adherence to treatment, and prevention of new infections (Mugavero et al., 2012). Such efforts at secrecy were not only isolating, but also exhausting, distressing, and shame inducing. As one participant said, “It’s the worst way to live.” Disclosure of seropositive status has been linked to benefits such as obtaining disease-specific social support (Kalichman, DiMarco, Austin, Luke, & DiFonzo, 2003), better mental health outcomes (Onwumere, Holttum, & Hirst, 2002), and improved treatment adherence (Kankou et al., 2017). However, with few exceptions, the majority of our study participants described negative consequences of disclosure. As such, further research may be needed before definitive recommendations can be made regarding disclosure by African immigrant PLWH.
Our study had several limitations. Namely, the findings may not be generalizable due to the specificity of the population. Our study sample included only English-speaking participants, thus excluding a number of African immigrants, particularly recent arrivals. Additionally, the majority of those who agreed to join the study had been living with HIV for many years (median = 11 years), potentially indicating a reluctance of newly diagnosed immigrants to participate. Individuals who were comfortable participating in a research study and discussing HIV-related experiences may be more likely to have developed positive coping strategies and to have reached a point of healthy acceptance of the disease and related stigma. Finally, including subjects from a number of disparate African countries, communities, and cultures may not sufficiently account for differences in experiences with HIV and its associated stigma. Despite these limitations, our study findings demonstrate important opportunities for future intervention and research.
Conclusion
HIV-related stigma is an extensive and pervasive challenge for African immigrant PLWH in a large northwest U.S. metropolitan area. The adapted biopsychosocial model is one way to conceptualize how HIV-related stigma manifests and how it ultimately impacts HIV morbidity, mortality, and transmission. Moreover, this conceptual framework can help guide targeted interventions to reduce the burden of HIV-related stigma in this population. Further research is needed to better understand the nuances of HIV-related stigma in individual African immigrant communities, particularly as it is related to disclosure of HIV diagnosis.
Key Considerations.
HIV-related stigma is an extensive and pervasive challenge for African immigrant PLWH in the United States.
The adapted biopsychosocial model is a useful tool for conceptualizing and comprehensively assessing how HIV-related stigma manifests in PLWH, affects their overall health and wellbeing, and impacts HIV morbidity, mortality, and trasnsmission.
In the biological health realm, HIV-related stigma contributes to adverse health care environments, disruptions in HIV care, and poor physical health.
In the psychological health realm, HIV-related stigma is associated with emotional vulnerability, depressive symptoms, and negative coping.
In the social health realm, HIV-related stigma leads to disclosure challenges, isolation, and poor social support.
Acknowledgments
Research reported in this manuscript was supported by NIAID, NCI, NIMH, NIDA, NICHD, NHLBI, NIA, NIGMS, NIDDK of the National Institutes of Health under award number AI027757 (PI Baeten).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosures
The authors report no real or perceived vested interests that relate to this article that could be construed as a conflict of interest.
Contributor Information
Paul E. Nevin, University of Washington School of Public Health, Seattle, Washington, USA.
Sarah Frey, University of Washington School of Public Health, Seattle, Washington, USA.
Lauren Lipira, University of Washington School of Public Health, Seattle, Washington, USA.
Meheret Endeshaw, University of Washington School of Public Health, Seattle, Washington, USA.
Lisa Niemann, University of Washington School of Public Health, Seattle, Washington, USA.
Roxanne P. Kerani, University of Washington School of Medicine, Seattle, Washington, USA.
Deepa Rao, University of Washington School of Public Health, Seattle, Washington, USA.
References
- American Psychological Association, Presidential Task Force on Immigration. Crossroads: The psychology of immigration in the new century. 2012 Retrieved from http://www.apa.org/topics/immigration/report.aspx.
- American Psychological Association, Presidential Task Force on Immigration. Crossroads: The psychology of immigration in the new century: Working with immigrant-origin clients: An update for mental health professionals. 2013 Retrieved from http://www.apa.org/topics/immigration/immigration-report-professionals.pdf.
- Blanas DA, Nichols K, Bekele M, Lugg A, Kerani RP, Horowitz CR. HIV/AIDS among African-born residents in the United States. Journal of Immigrant and Minority Health. 2013;15(4):718–24. doi: 10.1007/s10903-012-9691-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braun V, Clarke V. Using thematic analysis in psychology. Qualitative Research in Psychology. 2006;3(2):77–101. doi: 10.1191/1478088706qp063oa. [DOI] [Google Scholar]
- Engel GL. The need for a new medical model: A challenge for biomedicine. Science. 1977;196(4286):129–136. doi: 10.1126/science.847460. [DOI] [PubMed] [Google Scholar]
- Foley E. HIV/AIDS and African immigrant women in Philadelphia: Structural and cultural barriers to care. AIDS Care. 2005;17(8):1030–1043. doi: 10.1080/09540120500100890. [DOI] [PubMed] [Google Scholar]
- Flowers P, Davis M. Understanding the biopsychosocial aspects of HIV disclosure among HIV-positive gay men in Scotland. Journal of Health Psychology. 2013;18(5):711–724. doi: 10.1177/1359105312454037. [DOI] [PubMed] [Google Scholar]
- Goffman E. Stigma; notes on the management of spoiled identity. Englewood Cliffs, N.J: Prentice-Hall; 1963. [Google Scholar]
- Havelka M, Lučanin JD, Lučanin D. Biopsychosocial model–the integrated approach to health and disease. Collegium Antropologicum. 2009;33(1):303–310. [PubMed] [Google Scholar]
- Johnson AS, Hu X, Dean HD. Epidemiologic differences between native-born and foreign-born Black people diagnosed with HIV infection in 33 U.S. states, 2001–2007. Public Health Reports. 2010;125(Suppl. 4):61–69. doi: 10.1177/00333549101250S410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalichman S, DiMarco C, Austin M, Luke J, DiFonzo W. Stress, social support, and HIV-status disclosure to family and friends among HIV-positive men and women. Journal of Behavioral Medicine. 2003;26(4):315–332. doi: 10.1023/a:1024252926930. [DOI] [PubMed] [Google Scholar]
- Kankou J, Bouchaud M, Lele O, Bourgeois N, Spire D, Carrieri B, Abgrall P. Factors associated with HIV status disclosure in HIV-infected sub-Saharan migrants living in France and successfully treated with antiretroviral therapy: Results from the ANRS-VIHVO study. Journal of Immigrant and Minority Health. 2017;19(4):843–850. doi: 10.1007/s10903-016-0423-1. [DOI] [PubMed] [Google Scholar]
- Katz IT, Ryu AE, Onuegbu AG, Psaros C, Weiser SD, Bangsberg DR, Tsai AC. Impact of HIV-related stigma on treatment adherence: Systematic review and meta-synthesis. Journal of the International AIDS Society. 2013;16(3Suppl 2):18640. doi: 10.7448/IAS.16.3.18640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kharsany ABM, Karim QA. HIV infection and AIDS in sub-Saharan Africa: Current status, challenges and opportunities. The Open AIDS Journal. 2016;10:34–48. doi: 10.2174/1874613601610010034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koku EF. HIV-related stigma among African immigrants living with HIV/AIDS in USA. Sociological Research Online. 2010;15(3):5. doi: 10.5153/sro.2170. [DOI] [Google Scholar]
- Letteney S, Krauss B, Kaplan R. Examining HIV-positive parents' disclosure to their children: A biopsychosocial approach. Social Work in Public Health. 2012;27(4):345–360. doi: 10.1080/19371918.2010.500881. [DOI] [PubMed] [Google Scholar]
- Link BG, Phelan JC. Stigma and its public health implications. Lancet. 2006;367(9509):528–529. doi: 10.1016/s0140-6736(06)68184-1. [DOI] [PubMed] [Google Scholar]
- Merlin J, Zinski A, Norton W, Ritchie C, Saag M, Mugavero M, Hooten W. A conceptual framework for understanding chronic pain in patients with HIV. Pain Practice. 2014;14(3):207–216. doi: 10.1111/papr.12052. [DOI] [PubMed] [Google Scholar]
- Miles M, Huberman AM. Qualitative data analysis: An expanded sourcebook. 2. Thousand Oaks, CA: Sage Publications; 1994. [Google Scholar]
- Mitzel L, Vanable P, Brown J, Bostwick R, Sweeney S, Carey M. Depressive symptoms mediate the effect of HIV-related stigmatization on medication adherence among HIV-infected men who have sex with men. AIDS and Behavior. 2015;19(8):1454–1459. doi: 10.1007/s10461-015-1038-6. [DOI] [PubMed] [Google Scholar]
- Mugavero MJ, Amico KR, Westfall AO, Crane HM, Zinski A, Willig JH, Saag MS. Early retention in HIV care and viral load suppression: Implications for a test and treat approach to HIV prevention. Journal of Acquired Immune Deficiency Syndromes. 2012;59(1):86–93. doi: 10.1097/QAI.0b013e318236f7d2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muhr T. ATLAS/ ti: A prototype for the support of text interpretation. Qualitative Sociology. 1991;14(4):349–371. doi: 10.1007/BF00989645. [DOI] [Google Scholar]
- Nadeem E, Lange J, Edge D, Fongwa M, Belin T, Miranda J. Does stigma keep poor young immigrant and U.S.-born Black and Latina women fom seeking mental health care? Psychiatric Services. 2007;58(12):1547–1554. doi: 10.1176/ps.2007.58.12.1547. [DOI] [PubMed] [Google Scholar]
- Nyblade L, Stangl A, Weiss E, Ashburn K. Combating HIV stigma in health care settings: What works? Journal of the International AIDS Society. 2009;12(1):1–7. doi: 10.1186/1758-2652-12-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ojikutu B, Nnaji C, Sithole J, Schneider KL, Higgins-Biddle M, Cranston K, Earls F. All Black people are not alike: Differences in HIV testing patterns, knowledge, and experience of stigma between U.S.-born and non–U.S.-born Blacks in Massachusetts. AIDS Patient Care and STDs. 2013;27(1):45–54. doi: 10.1089/apc.2012.0312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Onwumere J, Holttum S, Hirst F. Determinants of quality of life in Black African women with HIV living in London. Psychology, Health and Medicine. 2002;7(1):61–74. doi: 10.1080/13548500120101568. [DOI] [Google Scholar]
- Othieno J. Understanding how contextual realities affect African born immigrants and refugees living with HIV in accessing care in the Twin Cities. Journal of Health Care for the Poor and Underserved. 2007;18(3):170–188. doi: 10.1353/hpu.2007.0085. [DOI] [PubMed] [Google Scholar]
- Rabkin JG. HIV and depression: 2008 review and update. Current HIV/AIDS Reports. 2008;5(4):163–171. doi: 10.1007/s11904-008-0025-1. [DOI] [PubMed] [Google Scholar]
- Remien R, Bauman L, Mantell J, Tsoi B, Lopez-Rios J, Chhabra R, Warne P. Barriers and facilitators to engagement of vulnerable populations in HIV primary care in New York City. Journal of Acquired Immune Deficiency Syndromes. 2015;69(Suppl. 1):S16–S24. doi: 10.1097/QAI.0000000000000577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scambler G. Health-related stigma. Sociology of Health & Illness. 2009;31(3):441–455. doi: 10.1111/j.1467-9566.2009.01161.x. [DOI] [PubMed] [Google Scholar]
- Short W, Vissandjée B. Women living with HIV in India: Looking up from a place of stigma, identifying nexus sites for change. Diversity and Equality in Health and Care. 2017;14(3):159. [Google Scholar]
- Smith RC, Fortin AH, Dwamena F, Frankel RM. An evidence-based patient-centered method makes the biopsychosocial model scientific. Patient Education and Counseling. 2013;91(3):265–270. doi: 10.1016/j.pec.2012.12.010. [DOI] [PubMed] [Google Scholar]
- Stutterheim S, Bos A, Shiripinda I, De Bruin M, Pryor J, Schaalma H. HIV-related stigma in African and Afro-Caribbean communities in the Netherlands: Manifestations, consequences and coping. Psychology & Health. 2012;27(4):395–411. doi: 10.1080/08870446.2011.585426. [DOI] [PubMed] [Google Scholar]
- Valdiserri RO. HIV/AIDS stigma: An impediment to public health. American Journal of Public Health. 2002;92(3):341–342. doi: 10.2105/AJPH.92.3.341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Brakel WH. Measuring health-related stigma--A literature review. Psychology, Health & Medicine. 2006;11(3):307–334. doi: 10.1080/13548500600595160. [DOI] [PubMed] [Google Scholar]
- Vance DE, Robinson FP. Reconciling successful aging with HIV: A biopsychosocial overview. Journal of HIV/AIDS & Social Services. 2004;3(1):59–78. doi: 10.1300/J187v03n01_06. [DOI] [Google Scholar]
- Wade DT, Halligan PW. The biopsychosocial model of illness: A model whose time has come. Clinical Rehabilitation. 2017;31(8):995–1004. doi: 10.1177/0269215517709890. [DOI] [PubMed] [Google Scholar]