Abstract
Low birthweight (LBW) is closely associated with fetal and perinatal mortality and morbidity. We identified the risk factors of LBW and geographical differences in LBW incidence in 30 Chinese provinces in the present study.
This study was a population-based, retrospective cohort study performed in 30 Chinese provinces. We used data from the free National Pre-pregnancy Checkups Project, which is a countrywide population-based retrospective cohort study. To identify regional differences in LBW incidence, we used the Qinling-Huaihe climate line to divide China into northern and southern sections and the Heihe-Tengchong economic line to divide it into eastern and western sections. Multivariate unconditional logistic regression analysis with SAS 9.4 was used for data analysis. P < .05 was considered statistically significant.
LBW incidence was 4.54% in rural China. Southern China had a significantly higher incidence (4.65%) than northern China (4.28%). Our main risk factor for LBW is paternal exposure to radiation (odds ratio = 1.537), which has never been studied before.
This study identifies multiple risk factors of couples giving birth to LBW babies including paternal risk factors.
Keywords: incidence, low birthweight infants, paternal exposure to radiation, risk factors
1. Introduction
Weight is an important indicator of infant health, and the mortality rate in low-weight infants is 40 times that of normal-weight infants.[1] According to the 2011 United Nations International Children's Emergency Fund report, an estimated 20 million low-birthweight (LBW) infants are born annually in developing countries, and LBW remains a significant public health problem in many developing countries. According to a study by Yi Chen et al, the incidence of LBW in mainland China was about 6.1%.[2] LBW infants are likely to have a high risk of infections, hospitalization, and physiological illness.[3] Further, they are more likely to develop atherosclerosis, hypertension, coronary artery disease, and chronic kidney disease later in life.[4–9] To lower the incidence of birth defects and improve the overall health of the population in China, the present study focused on the incidence and risk factors of LBW. Although similar studies of LBW have been performed in China, these studies seldom focus on the incidence of LBW because of the limited scope of population and most of them neglect the effects of paternal factors on LBW. Previous studies found some evidences that prenatal paternal factors can affect the offspring's physical characteristics and cause some diseases. A study of Bailey et al has shown that fathers who underwent more than one abdominal x-rays were more likely to give birth to children with acute lymphoblastic leukemia.[10] Other studies have proved that perceptional paternal exposure to radiation will cause the occurrence of other cancers like renal cancer and chondrosarcoma.[11] With the development of the medical technology, a report of United States indicated that the exposure to radiation has doubled during the past 3 decades, especially the medical radiation which is considered as small doses of radiation[12]; the link between medical radiation and radiation-related hereditary effects remains unclear. So many previous researches have evaluated the health effect of the offspring of atomic bomb survivors and occupational employees exposed to radiation. However, nobody focused on the relationship between parental pregestational exposure to radiation and LBW. We were the first to include the paternal exposure to medical radiation into our database to investigate whether it was related to LBW. Our study has large sample size since we used national data and received government support. In-depth research on LBW in China is still lacking, so our goal of this study was to identify those at risk for having a LBW baby. These families can focus on reducing their risk factors for LBW during prepregnancy and early pregnancy.
2. Methods
2.1. Data acquisition
The Population and Family Planning Commission collaborated with the Ministry of Finance of China to start the first wave of free pre-pregnancy physical examinations in 60% of the pilot counties in China between January 2010 and December 2012. We used data from childbearing-aged couples who delivered babies from January 2010 to December 2013 in the 31 pilot counties of China. The data used in this study came from the database of the free National Pre-pregnancy Checkups Project (NPCP), which is a population-based, retrospective cohort study of free, preconception medical examinations and services for rural reproductive-age couples who are trying to conceive throughout the 30 provinces of China. By the end of 2013, 11.42 million families had participated in this project and they had given birth to a total of 248,501 babies. We included 192,492 records with complete weight information for single live babies in this study (Fig. 1). We have gained ethics approval with the ethics committee of Chinese Academy Medical School and Peking Union Medical College Hospital (the reference number: S-K132). We have also obtained the consent to participate under the “Ethics, consent and permissions" heading and the consent to publish from the participant by signing informed consent forms (Chinese Edition) before they filled in the questionnaire (Supplemental informed consent English Edition). All methods were performed in accordance with the relevant guidelines and regulations.
Figure 1.
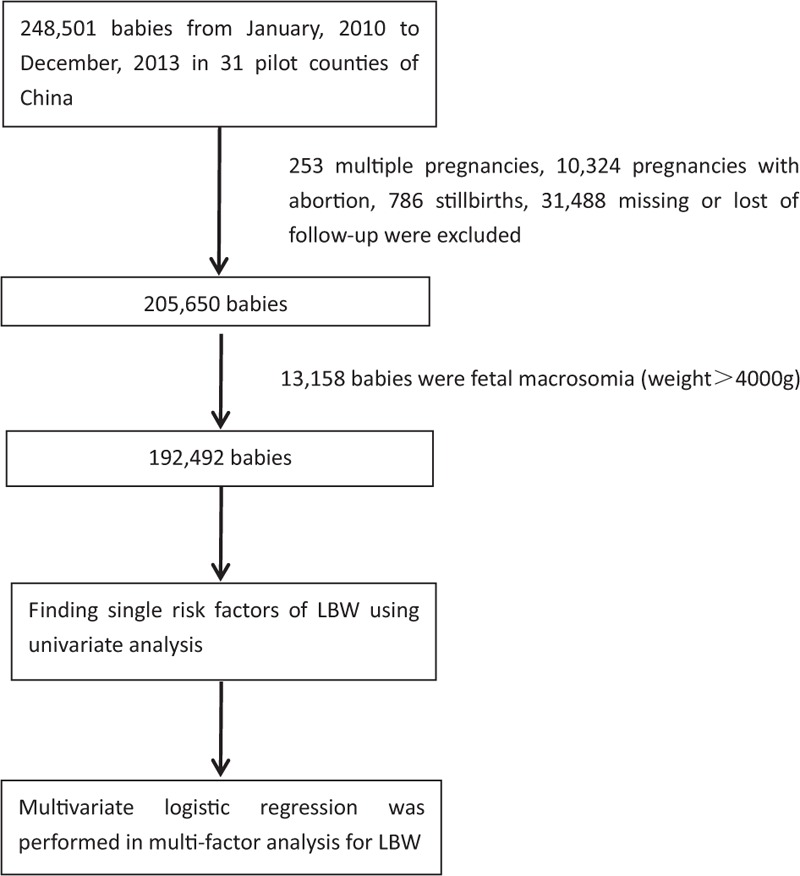
Study profile. A total of 192,492 pregnancies were analyzed after the missing or lost follow-up data, abortions, stillbirths, fetal macrosomia were excluded.
The clinical data were collected by professional medical staff and an application developer (somebody who programs apps for collecting information) during the preconception medical examination. After the examination, interviewers asked the couple questions which were planned in our study questionnaire. Newborn information was collected by a trained interviewer.
2.2. Data processing
2.2.1. Diagnosis and assignment to the LBW group
According to a manual published by the World Health Organization, LBW means a birthweight <2500 g9. As a result, infants’ weights were divided into 2 groups: a LBW (<2500 g) and a normal weight (2500–4000 g) group.
2.2.2. Variable grouping, assignment and definitions of variables
The data of exposure to radiation in the residence before pregnancy, which may indicate the exposure of x-ray, computed tomography (CT), positron emission tomography-computed tomography(PET-CT) or other radionuclide imaging before pregnancy, were obtained by a “yes or no” question, namely “If any x-ray, CT, PET-CT or other radionuclide imaging was underwent in your residence or workplace within 6 months before you got pregnant?” All the mothers/fathers whose answers to this question were “yes“ would be grouped as “exposed”, and the rest ones were defined as “non-exposed.” Oral contraception use means that mothers have used it within 6 months before pregnancy as well. We also asked the mothers to answer whether they take folic acid regularly within 1 month before pregnancy and during the previous 3 months, “Irregular” refers “No” in their answers. Stress statues and gum bleeding were recorded by their answers to “Do you feel stressed?” “Do you usually have gum bleeding?” on questionnaire as well, “Yes” means “Having stress” and “Having gum bleeding”, “No" means “Not having stress” and “No gum bleeding.” Table 2 shows how the variables were assigned to groups. In the table, “♂” means father of the baby and “♀” means mother. Chinese body mass index (BMI) classification standards were used in this study to classify different BMI groups.[13]
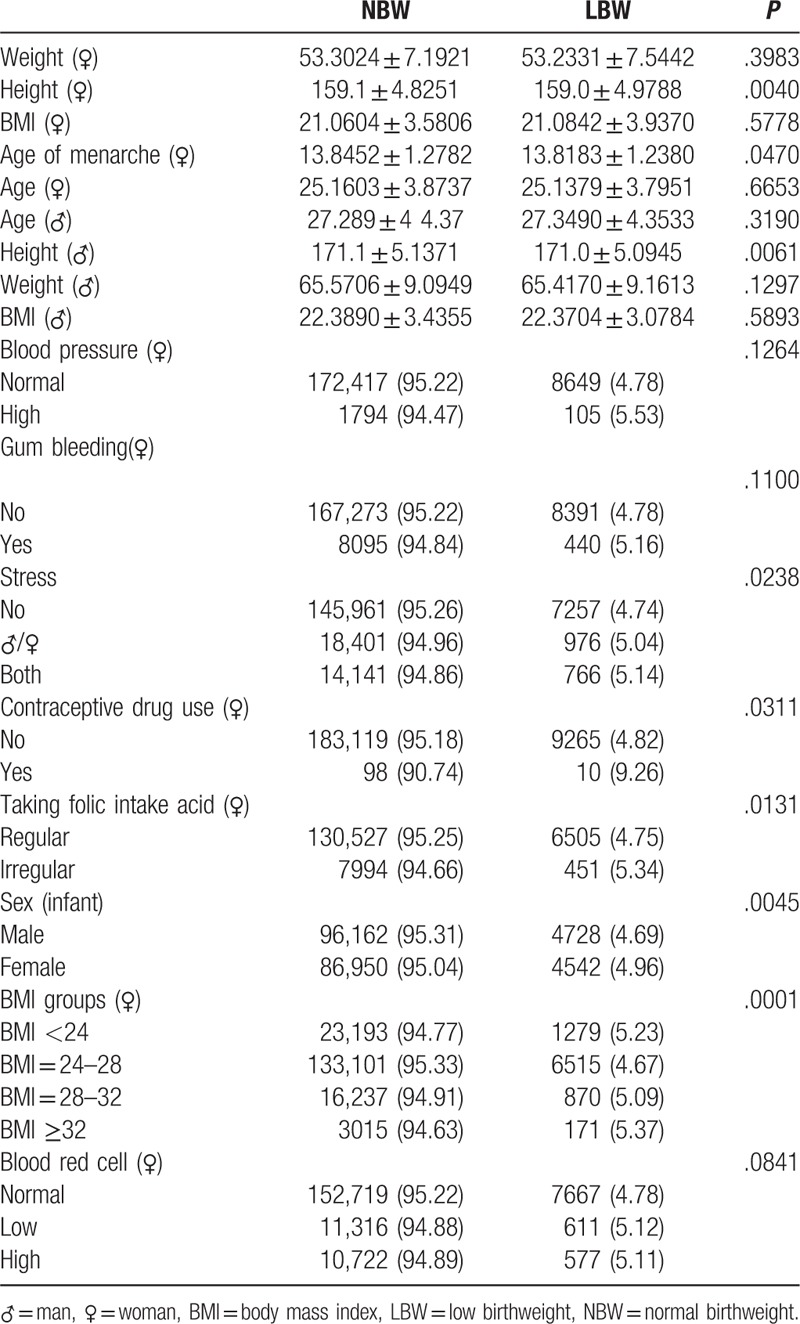
Table 2.
Factors found significant by univariate analysis.
2.2.3. Description of region designation
The 30 provinces included in the study were: Beijing, Hebei, Jiangsu, Anhui, Jilin, Zhejiang, Fujian, Jiangxi, Henan, Hubei, Guangdong, Sichuan, Chongqing, Yunnan, Shanxi, Tianjin, Shanghai, Guangxi, Hunan, Shandong, Hainan, Heilongjiang, Qinghai, Tibet, Inner Mongolia, Shanxi, Liaoning, Ningxia, Guizhou, and Gansu. In this study, we divided China geographically into 4 regions with the Qinling-Huaihe line, which bisects China into North and South regions based on climate and the Heihe-Tengchong line, which divides China into east and west regions based on economic development. Eastern China is more economically developed than western China as most of its cities are coastal cities (Fig. 2).
Figure 2.
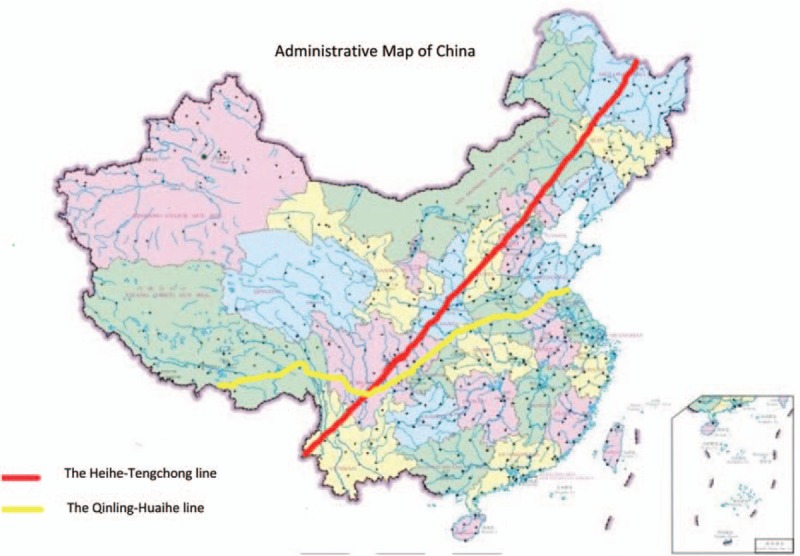
The map was created by Photoshop CS6 (URL: adobeid-na1.services.adobe.com) made by author CS, which is permitted to publis under an Open Access license by its copyright owner (Permission Document). The Heihe-Tengchong line and the Qinling-Huaihe line. The Heihe-Tengchong line is a line from Heihe in Heilongjiang province to Tengchong in Yunnan province. China was divided into south and north by the Heihe-Tengchong line. It was raised by geographer Weiyong Hu in 1935. The east has a more developed economy and degree of civilization than west. The Qinling-Huaihe line is along the Qinling Mountains.The Qinling Mountains are the barrier and boundary separating the climates of both northern and southern China; they are the highest mountains in central-western China. Natural conditions, agricultural production mode, geographical features and people's life styles greatly differ between the south and north of the Qinling-Huaihe line.
2.2.4. Statistical analyses
In our study, LBW was a dependent variable. In single-factor analysis, the χ2 test was used to analyze qualitative data, the independent sample t test and 1-way analysis of variance were used for quantitative data analysis. We also calculated the Spearman rank correlation coefficient for correlation analyses. Stepwise multivariate logistic regression was performed in multifactor analysis. Odds ratios (ORs) and 95% confidence intervals (CIs) were estimated by use of both univariate and multivariate analyses. P < .05 was considered statistically significant. SAS 9.4 statistical packages were used for data analysis.
3. Results
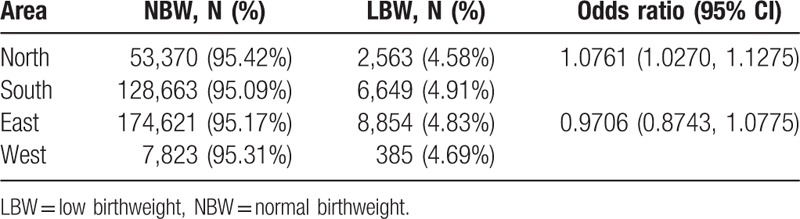
Of the 192,492 infants in our study, 9,275 of them were LBW with a mean weight of 2088.8 ± 407.4 g. There were 183,217 infants with a normal birthweight (NBW) and the mean NBW was 3311.3 ± 340.2 g (P < .001). Our results indicate that the incidence of LBW in mainland rural area of China was 4.54% with south China having a higher incidence of LBW (4.65%) compared with north China (4.28%, P < .001). There were little differences between the distribution of LBW incidences in eastern (4.55%) and western China (4.42%, P = .848) (Table 1).
Table 1.
The distribution of LBW in different regions of China.
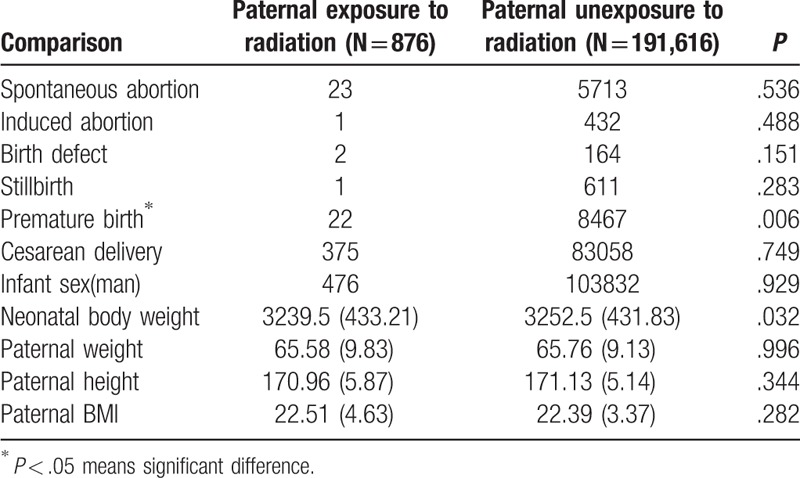
Several factors were found significant by univariate analysis. These factors included: weight (♂, ♀), height (♂, ♀), age of menarche (♀), age (♀), BMI (♀), exposure to poisonous materials and radiation (♀), blood pressure (♂), gum bleeding (♂), stress, use of a contraceptive drugs (♂), folic acid intake (♂), uterine activity, infant's sex, BMI(♀), and red blood cell count (♂) (“♂" means man, “♀" means woman) (Table 2). Factors found significant by multivariate analysis which were adjusted for age, occupation, education, sex of baby, parity were: hypertension (odds ratio [OR] = 2.326, [1.349,4.013], paternal exposure to radiation (OR = 1.537, [1.083,2.181]), contraceptive drug use (OR = 2.318, [1.059,5.074]), both parents with stress (OR = 1.146, [1.047,1.255]), irregular use of folic acid (OR = 1.121, [1.001,1.255]), maternal BMI <24 (OR = 1.113, [1.030,1.202]) (Fig. 3). Table 3 showed the comparison of both paternal and neonatal characteristics between fathers exposed to radiation and unexposed to radiation. The average infant birthweight in the group of fathers exposed to radiation was 3239.5 g, whereas it was 3252.5 g in the population who wa not exposed to radiation (P = .032). Additionally, fathers who were exposed to radiation were likely to give birth to premature infants (P = .006).
Figure 3.
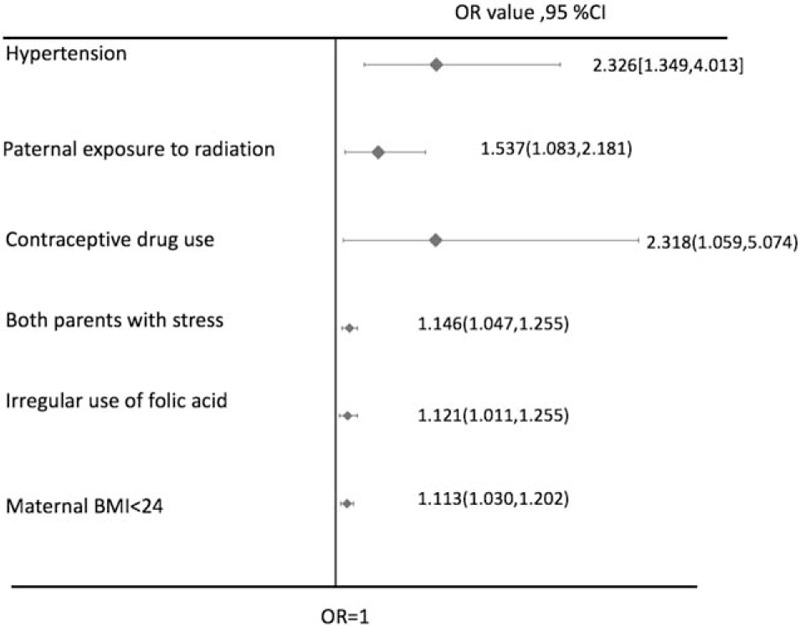
Risk factors found significant by multivariate analysis. These risk factors were adjusted for age, occupation, education, sex of baby, and parity.
Table 3.
The comparison of both paternal and neonatal characteristics between fathers exposed to radiation and unexposed to radiation.
4. Discussion
LBW is common worldwide, especially in developing countries. The percent of LBW in developing countries is far higher than in developed countries.[14,15]Therefore, it is especially important to find as many as risk factors of LBW. The data for this study came from the free NPCP. Our study had a large number of samples and this kind of large sample research has not happened in previous studies. Our data indicated that the incidence of LBW in rural areas of China was 4.54%. Southern China had a higher incidence of LBW (P < .05). There were no significant differences in LBW between eastern and western China. Climate and eating habits may play a critical role in the reason for the regional differences and similarities. People in the north are generally taller and heavier than those in the south, and the winter is much colder in the north than in the south. Therefore, people living in the north have diet that is high in calories; it may be the reason for the lower incidence of LBW in north.
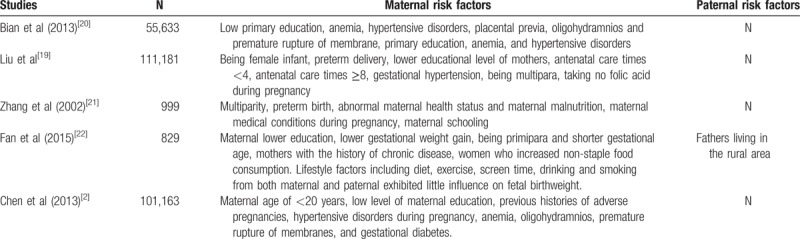
Among the studies of LBW worldwide, the significant maternal risk factors for LBW contained abnormal weight gain during pregnancy, low family functioning, stressful events, cigarette smoking, a previous preterm or LBW baby, anemia, and having a female baby.[16–18] Significant paternal factors related to LBW including paternal age, height, weight, birthweight, occupation, education, parental smoking, and alcohol use. In China, several similar researches have been concerned about the risk factors of LBW, but their samples and variables were limited and most of them focused on the maternal factors without including paternal risk factors. So we reviewed all studies covering the mainland China for the risk factors of LBW in China. Their studies covered the population between 869 and 111187. Only one of them contained the paternal risk factors of LBW (Table 4).
Table 4.
Studies covering the mainland China for the risk factors of LBW.
In our study, we found the following to be significant risk factors for LBW (using multivariate analysis): paternal exposure to radiation, hypertension, use of contraceptive drugs, presence of pressure in both parents, irregular use of folic acid, and maternal BMI <24 kg/m2.
It is generally known that maternal exposure to radiation before pregnancy can increase the possibility of fetal malformations including LBW. However, our results indicated that paternal history of exposing to radiation (OR = 1.329) was related to LBW and nobody has reported a relationship between paternal radiation exposure and LBW. Human studies showed that fathers who were exposed to the nuclear plant or medical radiation were prone to give birth to children with leukemia or defect. Recent studies proved that paternal exposure to radiation could cause gene instability, especially for those cancer-related genes. Many such genes suppressed or overexpressed in the next generations of irradiated mice 23. Another animal experiment showed that paternal irradiation would disturb the expression of circadian genes in offspring. They found that gene involved in rhythmic process overpresented in irradiated male mice 24. Besides, transgenerational instability of the next generation was observed in Mughal et al’ study[22] because of a threshold dose of acute paternal irradiation. But the reasons why paternal exposure to radiation was associated with LBW still needs further study. We hypothesize that the similar mechanism may act during the process of LBW formation. Several studies have been carried out on the gene etiology of LBW. Among them, Buschdorf et al's study found that gene expressed on hippocampal participated in the fetal development since 4% of genes expression of their study co-varied with DNA methylation levels in the tissue of nonhuman during this process 25. Recent research conducted by Rumbajan et al compared the placental DNA methylation levels between LBW and NBW; they finally detected low level of methylation in the promotor area of HUSB gene, which changed the placental gene expression, and thus may play a role in the pathogenesis of LBW 26. More investigations need to be done to establish this question.
Other risk factors including prepregnancy BMI, hypertension, oral contraceptive exposure, parental stress, and taking folic acid or used it irregularly were found to be significantly associated with LBW babies in other researches as well.[20–24]They are associated with maternal nutritional status, blood circulation, and the placental blood supply, which are related to many perinatal complications that may contribute to LBW incidence. Similar to Chen et al, our study also indicated an association between and LBW. We speculate that progesterone and E3 play a central role in pregnancy physiology, and maternal hormones are strongly correlated with birthweight and placental weight.
This study is the first to demonstrate that paternal exposure to radiation influences LBW incidence. These paternal risk factors need to be taken into consideration during conception and pregnancy. A limitation of this study is that some risk factors were only identified by questionnaires with a “Yes” or “No” question. A lot of variables were only qualitative indicators such as those variables that reflect the parents’ social and mental state and we were unable to provide correct and quantifiable outcomes. In addition, we are not able to build an effective risk prediction model to show a relatively sensitive and specific way to calculate relative risk.
5. Conclusions
We showed that the incidence of LBW in rural areas of China is 4.54%, and that south China has a higher incidence of LBW than north China (P < .05). Our work is the first to show the relationship between paternal exposure to radiation and LBW. The risk factors for LBW identified in this study are modifiable and preventable. To reduce LBW incidence in China, holistic approaches such as health education, maternal nutrition, improvement in socioeconomic indices, and increasing the quality and quantity of antenatal care services are of paramount importance.
Acknowledgments
The authors gratefully acknowledge the help of Xu Ma of National Research Institute for Family Planning, QiaoMei WANG,HaiPing SHEN, YiPing ZHANG of National health and family planning commission of the people's republic of China. They have given permission to be named in our study.
Footnotes
Abbreviations: BMI = body mass index, CIs = confidence intervals, CT = computed tomography, LBW = low birthweight, NBW = normal birthweight, NPCP = National Pre-pregnancy Checkups Project, ORs = odds ratios, PET-CT = positron emission tomography-computed tomography.
SC and YY contribute equally to this article.
This research received funding supported by National Natural Science Fund (81673184) and CAMS initiative for Innovative Medicine(2016-I2M-1–008).
The authors report no conflicts of interest.
References
- [1].Khalessi N, Kalani M, Araghi M, et al. The relationship between maternal vitamin d deficiency and low birth weight neonates. J Family Reprod Health 2015;9:113–7. [PMC free article] [PubMed] [Google Scholar]
- [2].Chen Y, Li G, Ruan Y, et al. An epidemiological survey on low birth weight infants in China and analysis of outcomes of full-term low birth weight infants. BMC Pregnancy Childbirth 2013;13:242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Loret de Mola C, de Franca GV, Quevedo Lde A, et al. Low birth weight, preterm birth and small for gestational age association with adult depression: systematic review and meta-analysis. Br J Psychiatry 2014;205:340–7. [DOI] [PubMed] [Google Scholar]
- [4].Osmond C, Barker DJ. Fetal, infant, and childhood growth are predictors of coronary heart disease, diabetes, and hypertension in adult men and women. Environ Health Perspect 2000;108(suppl 3):545–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Barker DJ. Early growth and cardiovascular disease. Arch Dis Child 1999;80:305–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Kaijser M, Bonamy AK, Akre O, et al. Perinatal risk factors for ischemic heart disease: disentangling the roles of birth weight and preterm birth. Circulation 2008;117:405–10. [DOI] [PubMed] [Google Scholar]
- [7].Huxley R, Neil A, Collins R. Unravelling the fetal origins hypothesis: is there really an inverse association between birthweight and subsequent blood pressure? Lancet (London, England) 2002;360:659–65. [DOI] [PubMed] [Google Scholar]
- [8].Carmody JB, Charlton JR. Short-term gestation, long-term risk: prematurity and chronic kidney disease. Pediatrics 2013;131:1168–79. [DOI] [PubMed] [Google Scholar]
- [9].Hogberg U. The World Health Report 2005: ”make every mother and child count“—including Africans. Scand J Public Health 2005;33:409–11. [DOI] [PubMed] [Google Scholar]
- [10].Bailey HD, Armstrong BK, de Klerk NH, et al. Exposure to diagnostic radiological procedures and the risk of childhood acute lymphoblastic leukemia. Cancer Epidemiol Biomarkers Prev 2010;19:2897–909. [DOI] [PubMed] [Google Scholar]
- [11].Pearce MS, Hammal DM, Dorak MT, et al. Paternal occupational exposure to electro-magnetic fields as a risk factor for cancer in children and young adults: a case-control study from the North of England. Pediatr Blood Cancer 2007;49:280–6. [DOI] [PubMed] [Google Scholar]
- [12].Mettler FA, Jr, Bhargavan M, Faulkner K, et al. Radiologic and nuclear medicine studies in the United States and worldwide: frequency, radiation dose, and comparison with other radiation sources—1950-2007. Radiology 2009;253:520–31. [DOI] [PubMed] [Google Scholar]
- [13].Chen C, Lu FC. The guidelines for prevention and control of overweight and obesity in Chinese adults. Biomed Environ Sci 2004;17(suppl):1–36. [PubMed] [Google Scholar]
- [14].de Onis M, Blossner M, Villar J. Levels and patterns of intrauterine growth retardation in developing countries. Eur J Clin Nutr 1998;52(suppl 1):S5–15. [PubMed] [Google Scholar]
- [15].Bergmann RL, Bergmann KE, Dudenhausen JW. Undernutrition and growth restriction in pregnancy. Nestle Nutr Workshop Ser Paediatr Program 2008;61:103–21. [DOI] [PubMed] [Google Scholar]
- [16].Andriani H, Kuo HW. Adverse effects of parental smoking during pregnancy in urban and rural areas. BMC Pregnancy Childbirth 2014;14:414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Shah PS. Paternal factors and low birthweight, preterm, and small for gestational age births: a systematic review. Am J Obstet Gynecol 2010;202:103–23. [DOI] [PubMed] [Google Scholar]
- [18].Reeb KG, Graham AV, Zyzanski SJ, et al. Predicting low birthweight and complicated labor in urban black women: a biopsychosocial perspective. Social Sci Med 1987;25:1321–7. [DOI] [PubMed] [Google Scholar]
- [19].Liu A, Zhang R, Li Z, et al. [Incidence of low birth weight among single live birth neonates and influencing factors in Shaanxi]. Zhonghua Liu Xing Bing Xue Za Zhi 2015;36:1244–8. [PubMed] [Google Scholar]
- [20].Dahlui M, Azahar N, Oche OM, et al. Risk factors for low birth weight in Nigeria: evidence from the 2013 Nigeria Demographic and Health Survey. Global Health Action 2016;9:28822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Zhang X, Liu Y, Lin L, et al. A case-control study on risk factors for low birth weight in China. Zhonghua Yu Fang Yi Xue Za Zhi 2002;36:158–60. [PubMed] [Google Scholar]
- [22].Cheng ER, Park H, Wisk LE, et al. Examining the link between women's exposure to stressful life events prior to conception and infant and toddler health: the role of birth weight. J Epidemiol Community Health 2016;70:245–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Bian Y, Zhang Z, Liu Q, et al. Maternal risk factors for low birth weight for term births in a developed region in China: a hospital-based study of 55,633 pregnancies. J Biomed Res 2013;27:14–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Fan C, Huang T, Cui F, et al. Paternal factors to the offspring birth weight: the 829 birth cohort study. Int J Clin Exp Med 2015;8:11370–8. [PMC free article] [PubMed] [Google Scholar]


