Abstract
Purpose
The purpose of this retrospective study with 4–12 years of follow-up was to compare the marginal bone loss (MBL) between external-connection (EC) and internal-connection (IC) dental implants in posterior areas without periodontal or peri-implant disease on the adjacent teeth or implants. Additional factors influencing MBL were also evaluated.
Methods
This retrospective study was performed using dental records and radiographic data obtained from patients who had undergone dental implant treatment in the posterior area from March 2006 to March 2007. All the implants that were included had follow-up periods of more than 4 years after loading and satisfied the implant success criteria, without any peri-implant or periodontal disease on the adjacent implants or teeth. They were divided into 2 groups: EC and IC. Subgroup comparisons were conducted according to splinting and the use of cement in the restorations. A statistical analysis was performed using the Mann-Whitney U test for comparisons between 2 groups and the Kruskal-Wallis test for comparisons among more than 2 groups.
Results
A total of 355 implants in 170 patients (206 EC and 149 IC) fulfilled the inclusion criteria and were analyzed in this study. The mean MBL was 0.47 mm and 0.15 mm in the EC and IC implants, respectively, which was a statistically significant difference (P<0.001). Comparisons according to splinting (MBL of single implants: 0.34 mm, MBL of splinted implants: 0.31 mm, P=0.676) and cement use (MBL of cemented implants: 0.27 mm, MBL of non-cemented implants: 0.35 mm, P=0.178) showed no statistically significant differences in MBL, regardless of the implant connection type.
Conclusions
IC implants showed a more favorable bone response regarding MBL in posterior areas without peri-implantitis or periodontal disease.
Keywords: Alveolar bone loss, Dental implants, Dental implant-abutment design, Retrospective studies
Graphical Abstract
INTRODUCTION
When dental implants confront the oral environment and functional loading, marginal bone loss (MBL) occurs to some degree, even in areas without peri-implant disease. MBL following implant placement can be a critical factor affecting esthetics and implant longevity because it is associated with an increased risk of peri-implantitis and tissue collapse [1]. Therefore, identifying the reasons for MBL has been an important issue in the field of implant dentistry. According to the literature, MBL following implant placement is known to be influenced by the implant design and the surroundings. It has been reported that approximately 0.9–1.5 mm of MBL occurs during the first year of loading, with 0.1–0.2 mm of MBL per year occurring thereafter [2,3,4,5]. Most MBL occurs in the early stage after implant placement, and the bone level seldom changes during the functional life of the implant [6,7]; this is also supported by the study of Assenza et al., who reported that there was no significant change in osteoclastic activity after functional loading [8].
Changes in the marginal bone level around the implant are considered to be a multifactorial phenomenon that has not yet been fully clarified [9,10]. Among the many related factors, biomechanical factors in relation to the implant crest module, including the type of implant (1-piece vs. 2-piece implants), platform switching, the location of microcaps, and the implant connection type, have been actively explored [11,12,13]. The crest module is the transosteal region of an implant body designed to accept the prosthetic component, or the transition zone at the crest of the ridge [14]. As hard and soft tissue breakdown begins at this region in most clinical situations, the importance of studies regarding this topic cannot be overemphasized. The presence of a microgap at the level of the implant-abutment junction is also an important factor from mechanical and bacteriological perspectives. MBL occurs due to micromovement on the site of the microgap, resulting from an insufficient amount of soft tissue for a self-defense mechanism from external stimuli; this dynamic can be regarded as similar to the problems posed by insufficient biologic width of a natural tooth [11]. Therefore, the platform switching concept was introduced in an effort to ensure sufficient distance from external stimuli to the bone. Schwarz et al. [15] reported that the platform switching concept tended to prevent or minimize MBL. Several studies also reported that implant neck design and implant connection types could be related to MBL [15,16,17,18]. From a prosthetic perspective, Quirynen et al. [19] reported that overload caused by a lack of anterior contact, parafunctional habits, and osseointegrated full-fixed prostheses in both arches correlated with excessive MBL after the first year of loading. When loaded, a high stress concentration occurs at the marginal bone area surrounding the neck portion of the implant because of the lack of a periodontal ligament. Prendergast and Huiskes [20] suggested that microdamage caused by overloading seemed to act as the first step in the initiation of bone resorption through finite element analysis. However, most studies regarding MBL around dental implants did not clarify whether periodontal disease on the adjacent teeth and/or peri-implant disease at the implant site was present.
Considering the factors involved in crest module design, which may or may not affect changes in the marginal bone level, implants can be generally classified into the external-connection (EC) type and internal-connection (IC) type according to the type of implant-abutment connection [17,19]. Although EC implants characterized by an external hexagon were developed first and have been widely used for several decades, the micromovements of the abutments due to their limited hexagonal height have remained a drawback [21]. In contrast, IC implants, with a conical internal self-locking system, have shown excellent mechanical stability and the ability to reduce stress on the marginal bone by transferring the exerted stress toward the apical area [22]. Although both types have shown high success rates in many previous studies, less MBL has been reported in IC implants [3,17,23]. As for splinting, Vigolo and Zaccaria [24] reported that the peri-implant MBL around non-splinted implants was not statistically significantly different from that observed in splinted implants in a 5-year prospective study. Five years later, however, they additionally reported that multiple implants with splinted restorations showed significantly less MBL than did non-splinted implants in a 10-year randomized controlled trial, although the difference was not clinically meaningful [25]. In addition to splinting, the use of cement could also be related to MBL. Although this issue remains controversial, several studies have reported that cement-retained implant restorations had more frequent biological complications involving inflammation [26,27].
To the best of our knowledge, most studies comparing MBL between EC and IC implants did not clarify whether periodontal disease on the adjacent teeth and/or peri-implant disease at the implant site was present. Therefore, the purpose of this retrospective study with 4–12 years of follow-up was to compare the MBL between EC and IC dental implants in posterior areas without periodontal disease on the adjacent teeth or peri-implant disease at the implant site, and to determine whether splinting or the use of cement affected MBL.
MATERIALS AND METHODS
Study design and subjects
This retrospective study was performed based on dental records and radiographic data obtained from patients who underwent dental implant treatment at the Department of Periodontics, Seoul National University Dental Hospital, from March 2006 to March 2007. This study was approved by the Institutional Review Board of the Seoul National University Dental Hospital (approval No. CRI15019).
The following inclusion criteria were defined: 1) implants with a follow-up period of more than 4 years after loading; 2) single implants and multiple implants splinted with a fixed dental prosthesis in the posterior region; 3) cases with sufficient records and radiographs showing pre-surgical, post-surgical, post-prosthetic, and more than 4-year follow-up status after loading; 4) bone-level implants placed at the level of the alveolar bone crest; 5) implants satisfying the success criteria proposed by Albrektsson et al. [4] without any sign of peri-implant disease (1.5 mm of MBL in the first year after loading plus 0.2 mm per year in the subsequent years until the last follow-up); 6) implants with no definable radiographic bone loss representing periodontitis on the adjacent teeth; and 7) implants without any history of active periodontal therapy on the adjacent teeth and implant site during the follow-up period.
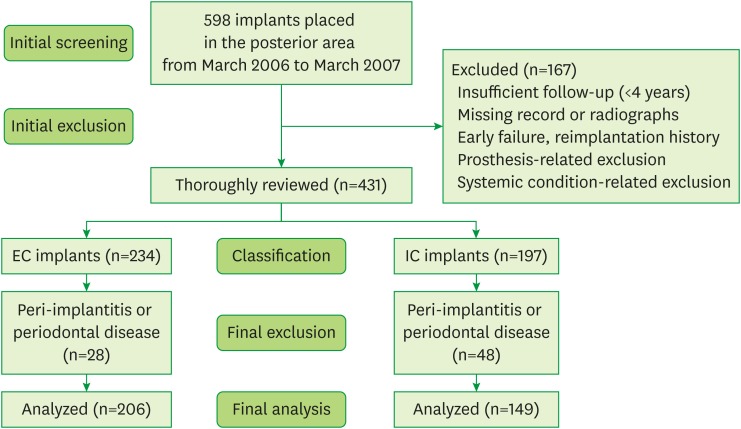
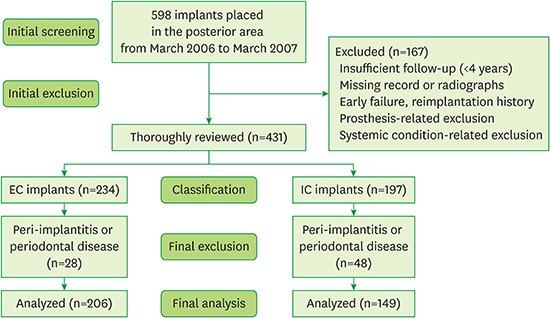
The exclusion criteria were as follows: 1) implants splinted with the adjacent natural teeth; 2) implants supporting any types of overdentures or removable partial dentures; 3) implants with cantilevered fixed partial dentures; 4) implants with restorations opposing removable partial or complete dentures; 5) tissue-level IC implants; 6) immediately placed implants; 7) any uncontrolled systemic diseases that could influence the outcomes of implant therapy (e.g., diabetes or osteoporosis); 8) any medications that could influence bone and mucosal healing (e.g., steroids or anti-resorptives); 9) less than 4 years of follow-up after loading; 10) insufficient records and/or unmeasurable radiographs; 11) additional therapy to control inflammation around the implants or adjacent teeth; 12) any type of implant failures or reimplantation. The flow diagram for this study is shown in Figure 1.
Figure 1. Flow diagram of this study. A total of 598 implants were initially surveyed, and 167 implants with an insufficient follow-up period (<4 years), missing records or radiographs, early failure or reimplantation (due to fixture fracture or failure for any other reason), and any prosthetic state or systemic condition corresponding to the exclusion criteria were excluded. The remaining 431 implants were thoroughly reviewed and classified as EC (n=234) or IC (n=197) implants. Implants with peri-implantitis or periodontal disease on the adjacent teeth were further excluded. Finally, 355 implants from 170 patients (206 EC implants, 73 patients/149 IC implants, 97 patients) were included and analyzed in this study.
EC: external-connection, IC: internal-connection.
Implants and reviewed surgical protocols
Implants were primarily classified as EC implants (Brånemark Mk III TiUnite [Nobel Biocare AB, Gothenburg, Sweden], Hexplant [Warantec, Seongnam, Korea], Restore RBM [Keystone Dental, Burlington, MA, USA], and US II [Osstem implant, Seoul, Korea]) or IC implants (Inplant [Warantec], ITI SLA [Institut Straumann, Basel, Switzerland], GS II [Osstem implant], Implantium [Dentium, Seoul, Korea], and Osseotite [3i/Implant Innovations, Palm Beach Gardens, FL, USA]) and additionally divided into subgroups according to whether a splint was used and whether cement was used (screw-retained vs. cement-retained or screw and cement-retained prostheses) in the restorations. Detailed information about the patients according to implant connection type is presented in Table 1.
Table 1. Demographic characteristics of the patients (n=170).
| Age (yr) | External-connection | Internal-connection | Total (No.) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Male | Female | Subtotal | Male | Female | Subtotal | Male | Female | Subtotal | |
| <20 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 20–39 | 2 | 3 | 5 | 2 | 6 | 8 | 4 | 9 | 13 |
| 40–59 | 27 | 24 | 51 | 34 | 35 | 69 | 61 | 59 | 120 |
| 60–79 | 11 | 6 | 17 | 11 | 9 | 20 | 22 | 15 | 37 |
| ≥80 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Mean±SD | 54±9 | 52±8 | 53±8 | 56±9 | 51±10 | 53±10 | 55±9 | 51±9 | 53±9 |
| Patients (No.) | 40 | 33 | 73 | 47 | 50 | 97 | 87 | 83 | 170 |
SD: standard deviation.
All the implant operations were conducted under sterilized conditions, using either a 1- or a 2-stage protocol. Prosthetic procedures commenced at least 3 and 5 months after the operation for the mandible and maxilla, respectively. Based on the patients' records, primary stability was achieved in every case and antibiotics, nonsteroidal anti-inflammatory drugs, and chlorhexidine mouth rinse were routinely administered postoperatively.
Radiographic evaluation
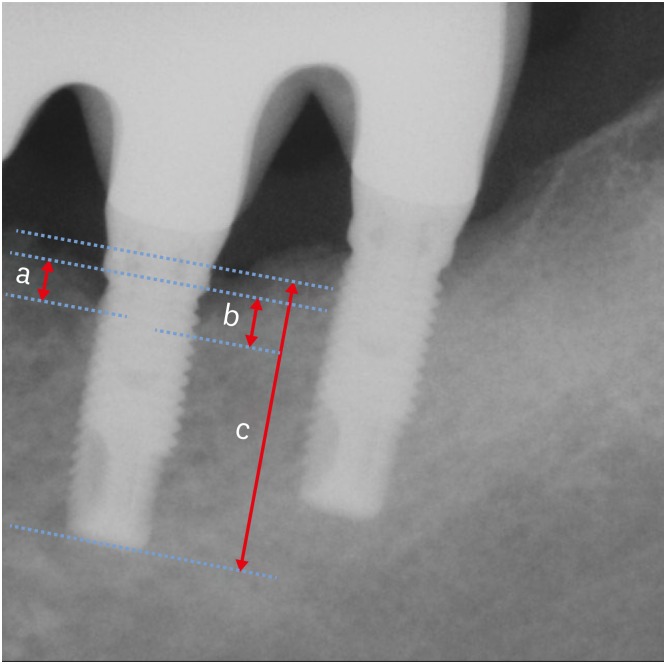
Radiographic measurements of MBL were performed using either panoramic radiographs or intraoral periapical radiographs according to previously described methods [28,29]. MBL was calculated using the known length of the implant fixture (IF) as follows:
Separate measurements were made for the mesial and distal aspects, and larger values were used for further analysis (Figure 2). MBL was presented as total bone loss and annual bone loss (ABL). The latter was obtained from dividing the total bone loss by the number of follow-up years since prosthetic loading. Radiographic measurements were performed by a single investigator to minimize the repetition of possible operator-dependent bias. The intraexaminer reliability over 2 repeated measurements was strong (intraclass correlation=0.862; P<0.001).
Figure 2. MBL measurements were made separately for the mesial and distal aspects, and larger values were used for further analysis. “a” and “b” depict the measured length from the top of the rough surface of the IF to the mesial and distal first bone implant contact points, respectively. “c” depicts the measured length of the IF.
MBL: marginal bone loss, IF: implant fixture.
Statistical analysis
As the mean ABL values did not follow a normal distribution (Kolmogorov-Smirnov test, P<0.05), the Mann-Whitney U test for non-parametric statistical analysis was used. Since splinting and cement use were significant variables based on the results of the multivariate analysis, the mean MBL was transformed into an ordinal variable, and 2-way analysis of variance was performed. The Kruskal-Wallis test was used for comparisons among more than 2 groups. Data were presented as the mean±standard deviation (SD), and P values less than 0.05 were considered to indicate statistical significance. Statistical analyses were performed using commercially available software (SPSS 22.0, IBM Corp., Armonk, NY, USA and Microsoft Excel, Microsoft Corp., Redmond, WA, USA).
RESULTS
A total of 355 implants in 170 patients (206 EC implants and 149 IC implants) fulfilled the inclusion criteria and were ultimately included in this study.
Overall statistics
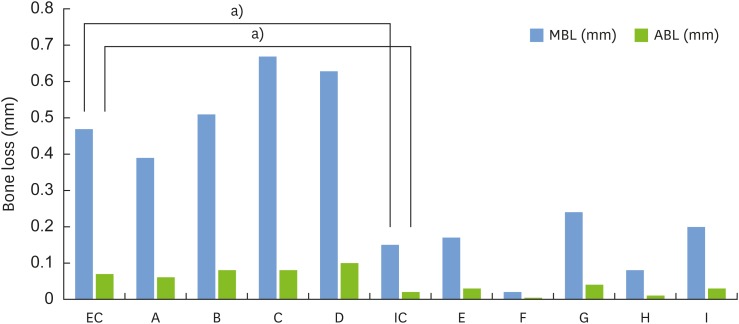
The mean follow-up period was 6.73±1.33 years. The mean MBL was 0.33±0.56 mm and the mean ABL was 0.05±0.08 mm (Table 2). The mean MBL and mean ABL around EC and IC implants, as well as the results of the subgroup analyses of single-stand versus splinted implants and cemented versus non-cemented implants, are presented in Table 3. Both the mean MBL and mean ABL were significantly greater around EC implants than around IC implants (P<0.001, Figure 3 and Table 3). No statistically significant differences were found between the single-stand implants and the splinted implants. Additionally, no statistically significant differences were found between the cemented and non-cemented implants in either the MBL or ABL measurements (Table 3).
Table 2. General characteristics of dental implants (n=355).
| Variables | Mean±SD | Max–Min |
|---|---|---|
| Follow-up period (yr) | 6.73±1.33 | 4.0–12.0 |
| Mean MBL (mm) | 0.33±0.56 | 0.0–2.5 |
| Mean ABL (mm/yr) | 0.05±0.08 | 0.00–0.44 |
SD: standard deviation, MBL: marginal bone loss, ABL: annual bone loss.
Table 3. The amount of MBL and ABL according to the implant connection type (n=355).
| Variables | Category | Subjects | MBL (mm) | ABL (mm) | P value (MBL/ABL) |
|---|---|---|---|---|---|
| Connection type | EC | 206 (58.0) | 0.47±0.65a) | 0.07±0.09a) | <0.001/<0.001 |
| IC | 149 (42.0) | 0.15±0.33a) | 0.02±0.05a) | ||
| Splinting | Single | 70 (19.7) | 0.31±0.58 | 0.05±0.08 | 0.676/0.642 |
| Splinted | 285 (80.3) | 0.34±0.56 | 0.05±0.08 | ||
| Use of cement | Cemented | 77 (21.3) | 0.27±0.53 | 0.04±0.08 | 0.178/0.195 |
| Non-cemented | 270 (78.7) | 0.35±0.58 | 0.05±0.08 |
Data are shown number (%) or mean±SD.
MBL: marginal bone loss, ABL: annual bone loss, EC: external-connection, IC: internal-connection, SD: standard deviation.
a)Statistically significant between groups (P<0.05). EC implants showed more MBL and ABL.
Figure 3. Mean MBL and mean ABL according to the type of implant-abutment connection (A to D: EC implants, E to I: IC implants). EC implants showed greater values of MBL and ABL.
MBL: marginal bone loss, ABL: annual bone loss, EC: external-connection, IC: internal-connection.
a)Statistically significant between groups (P<0.05).
EC implants
The mean MBL and mean ABL around EC implants (n=206) were 0.47±0.65 mm and 0.07±0.09 mm, respectively (Table 3). The subgroup analyses of MBL within the EC group (single-stand implants vs. splinted implants and cemented vs. non-cemented implants) showed no statistically significant differences, with values of 0.44±0.64 mm vs. 0.58±0.72 mm (P=0.691) and 0.44±0.64 mm vs. 0.58±0.72 mm (P=0.307), respectively (Table 4).
Table 4. The amount of MBL and ABL according to splinting and cement use in EC implants (n=206).
| Variables | Category | Subjects | MBL (mm) | ABL (mm) | P value (MBL/ABL) |
|---|---|---|---|---|---|
| Splinting | Single | 32 (15.5) | 0.52±0.76 | 0.08±0.10 | 0.691/0.714 |
| Splinted | 174 (84.5) | 0.45±0.63 | 0.07±0.09 | ||
| Use of cement | Cemented | 27 (13.1) | 0.58±0.72 | 0.09±0.10 | 0.223/0.415 |
| Non-cemented | 179 (86.9) | 0.44±0.64 | 0.07±0.09 |
Data are shown number (%) or mean±SD.
MBL: marginal bone loss, ABL: annual bone loss, EC: external-connection, SD: standard deviation.
IC implants
The mean MBL and mean ABL around IC implants (n=149) were 0.15±0.33 mm and 0.02±0.05 mm, respectively (Table 3). The subgroup analyses of MBL within the IC group (single-stand implants vs. splinted implants and cemented vs. non-cemented implants) showed no statistically significant differences, with values of 0.13±0.28 mm vs. 0.16±0.35 mm (P=0.978) and 0.11±0.29 mm vs. 0.17±0.33 mm (P=0.148), respectively (Table 5).
Table 5. Amount of MBL according to splinting and cement use in IC implants (n=149).
| Variables | Category | Subjects | MBL (mm) | ABL (mm) | P value (MBL/ABL) |
|---|---|---|---|---|---|
| Splinting | Single | 38 (15.5) | 0.13±0.28 | 0.02±0.04 | 0.978/0.878 |
| Splinted | 111 (84.5) | 0.16±0.35 | 0.03±0.06 | ||
| Use of cement | Cemented | 91 (13.1) | 0.11±0.29 | 0.02±0.05 | 0.148/0.268 |
| Non-cemented | 50 (86.9) | 0.17±0.33 | 0.03±0.05 |
Data are shown number (%) or mean±SD.
MBL: marginal bone loss, IC: internal-connection, ABL: annual bone loss, SD: standard deviation.
DISCUSSION
The purpose of this study was to compare MBL between EC and IC dental implants in posterior areas without periodontal disease on the adjacent teeth or the peri-implant disease at the implant site. This study also sought to identify the medium- to long-term effects on MBL not caused by the bacteria-induced inflammatory environment, but by biomechanical influences depending on the implant abutment connection type itself. Comparisons of MBL were additionally conducted in subgroup analyses according to splinting and cement use to take into account the possible contributions of these factors to MBL. All included implants satisfied the implant success criteria [4] and had an available follow-up of at least 4 years after functional loading. The reason why we selected only the posterior area was to exclude the possible influence of differences in alveolar bone thickness and occlusal force on MBL. In addition, precise measurements on panoramic radiographs of bone loss in the anterior teeth are technically very difficult due to image distortion, especially if no other radiographs are available.
In the present study, the mean MBL around EC implants was greater than that around IC implants, which is consistent with most previous studies. Koo et al. [17] investigated MBL according to the implant abutment connection mode. The mean MBL around EC implants was 0.61 mm until loading and 0.29 mm in the next year, whereas the mean MBL around IC implants was only 0.08 mm until loading and marginal bone gain was achieved in the subsequent year. Laurell and Lundgren [23] also reported favorable outcomes regarding marginal bone level changes around IC implants in a meta-analysis. Goiato et al. [3] reported similar findings in a literature review. Areas of MBL around IC implants with a Morse taper structure showed less bacterial infiltration [3], suggesting that the implant connection type could influence bacterial infection and the occurrence of inflammation in the peri-implant tissue. IC implants have an inherent platform switching structure, in which the implant abutment junction is moved away from the adjacent marginal bone, and the Morse taper structure could also minimize microgaps and thereby prevent bacterial infiltration [30,31,32]. The conical structure of the Morse taper has high resistance to distortion and rotation, which could minimize the load on the screw itself and also prevent screw looseness and fracture. In this study, implants with peri-implantitis or periodontal disease on the adjacent teeth were excluded, because the goal was to focus on the MBL caused not by the bacteria-induced inflammatory response, but by biomechanical factors depending on the implant abutment connection type. Although bone loss thresholds for diagnosing peri-implantitis vary in the literature, more than 2 mm of bone loss around a dental implant is the most widely accepted criterion for peri-implantitis [33,34]. Considering the diversity of the follow-up periods, the criterion (1.5 mm in the first year after loading plus 0.2 mm per year in the subsequent years until the last follow-up) suggested by Albrektsson et al. [4] was selected as the acceptable MBL limit in this study. In addition to the direct comparison of MBL in EC and IC implants, we also performed subgroup analyses according to splinting and cement use to exclude the influence of those factors. For similar reasons, overdenture cases were not included because the implant suprastructure could influence the stress distribution and clinical outcomes [35,36].
In the subgroup analysis, there was no statistically significant difference between single-stand and splinted prostheses. Naert et al. [37] reported that implants in a 2-implant mandibular overdenture concept exposed to overload in inflammatory conditions showed accelerated inflammatory bone resorption. In addition to splinting, several studies reported that cement-retained implant restorations had more frequent biological complications related to inflammation [26,27]. It has been reported that cement-retained restorations exhibited a more even stress distribution than did screw-retained prostheses [26], although they had larger marginal openings [26] and showed more frequent biological complications, such as MBL exceeding 2 mm [27]. However, there were no statistically significant differences in this study between cemented and non-cemented restorations.
The main limitation of this study is that we could not differentiate among surgical protocols, such as 1-stage or 2-stage procedures performed by multiple surgeons. In addition, the analysis of X-ray-based computed tomography, rather than 2-dimensional radiographs, would have allowed a better characterization of bone loss. This study also has the limitation of being record-dependent, which is an inherent issue in retrospective studies. We could not exclude smokers due to a lack of detailed information. Additionally, as Galindo-Moreno et al. [38] reported that abutment length could influence the MBL and that short abutments (<2 mm) showed more MBL, abutment length should have been taken into account as a contributing factor.
The amount of MBL was significantly greater around EC implants than around IC implants in posterior areas without periodontal or peri-implant disease on the adjacent teeth or implants. Splinting and cement use did not influence MBL around implants regardless of the implant connection type. IC implants presented more favorable bone responses regarding changes in the marginal bone level in posterior areas without peri-implantitis or periodontal disease.
Footnotes
Funding: This study was supported by grant No. 04-2013-0071 from the Seoul National University Dental Hospital (SNUDH) Research Fund.
Author Contributions: Conceptualization: Dae-Hyun Kim, Sungtae Kim, Ki-Tae Koo, Tae-Il Kim; Formal analysis: Dae-Hyun Kim, Hyun Ju Kim, Ki-Tae Koo, Yang-Jo Seol, Yong-Moo Lee; Investigation: Dae-Hyun Kim, Hyun Ju Kim, Tae-Il Kim; Methodology: Dae-Hyun Kim, Hyun Ju Kim, Yang-Jo Seol, Tae-Il Kim; Project administration: Sungtae Kim, Young Ku, In-Chul Rhyu; Writing - original draft: Dae-Hyun Kim, Hyun Ju Kim; Writing - review & editing: Sungtae Kim, Ki-Tae Koo, Tae-Il Kim, Yang-Jo Seol, Yong-Moo Lee, Young Ku, In-Chul Rhyu.
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
References
- 1.Aparna IN, Dhanasekar B, Lingeshwar D, Gupta L. Implant crest module: a review of biomechanical considerations. Indian J Dent Res. 2012;23:257–263. doi: 10.4103/0970-9290.100437. [DOI] [PubMed] [Google Scholar]
- 2.Adell R, Lekholm U, Rockler B, Brånemark PI. A 15-year study of osseointegrated implants in the treatment of the edentulous jaw. Int J Oral Surg. 1981;10:387–416. doi: 10.1016/s0300-9785(81)80077-4. [DOI] [PubMed] [Google Scholar]
- 3.Goiato MC, Pellizzer EP, da Silva EV, Bonatto LR, dos Santos DM. Is the internal connection more efficient than external connection in mechanical, biological, and esthetical point of views? A systematic review. Oral Maxillofac Surg. 2015;19:229–242. doi: 10.1007/s10006-015-0494-5. [DOI] [PubMed] [Google Scholar]
- 4.Albrektsson T, Zarb G, Worthington P, Eriksson AR. The long-term efficacy of currently used dental implants: a review and proposed criteria of success. Int J Oral Maxillofac Implants. 1986;1:11–25. [PubMed] [Google Scholar]
- 5.Romeo E, Lops D, Margutti E, Ghisolfi M, Chiapasco M, Vogel G. Long-term survival and success of oral implants in the treatment of full and partial arches: a 7-year prospective study with the ITI dental implant system. Int J Oral Maxillofac Implants. 2004;19:247–259. [PubMed] [Google Scholar]
- 6.Laine P, Salo A, Kontio R, Ylijoki S, Lindqvist C, Suuronen R. Failed dental implants - clinical, radiological and bacteriological findings in 17 patients. J Craniomaxillofac Surg. 2005;33:212–217. doi: 10.1016/j.jcms.2004.12.004. [DOI] [PubMed] [Google Scholar]
- 7.Behneke A, Behneke N, d'Hoedt B. A 5-year longitudinal study of the clinical effectiveness of ITI solid-screw implants in the treatment of mandibular edentulism. Int J Oral Maxillofac Implants. 2002;17:799–810. [PubMed] [Google Scholar]
- 8.Assenza B, Scarano A, Petrone G, Iezzi G, Thams U, San Roman F, et al. Osteoclast activity around loaded and unloaded implants: a histological study in the beagle dog. J Oral Implantol. 2003;29:1–7. doi: 10.1563/1548-1336(2003)029<0001:OAALAU>2.3.CO;2. [DOI] [PubMed] [Google Scholar]
- 9.Atieh MA, Ibrahim HM, Atieh AH. Platform switching for marginal bone preservation around dental implants: a systematic review and meta-analysis. J Periodontol. 2010;81:1350–1366. doi: 10.1902/jop.2010.100232. [DOI] [PubMed] [Google Scholar]
- 10.Jones AA, Cochran DL. Consequences of implant design. Dent Clin North Am. 2006;50:339–360. v. doi: 10.1016/j.cden.2006.03.008. [DOI] [PubMed] [Google Scholar]
- 11.Hermann JS, Buser D, Schenk RK, Schoolfield JD, Cochran DL. Biologic Width around one- and two-piece titanium implants. Clin Oral Implants Res. 2001;12:559–571. doi: 10.1034/j.1600-0501.2001.120603.x. [DOI] [PubMed] [Google Scholar]
- 12.Hermann JS, Schoolfield JD, Nummikoski PV, Buser D, Schenk RK, Cochran DL. Crestal bone changes around titanium implants: a methodologic study comparing linear radiographic with histometric measurements. Int J Oral Maxillofac Implants. 2001;16:475–485. [PubMed] [Google Scholar]
- 13.Hermann JS, Schoolfield JD, Schenk RK, Buser D, Cochran DL. Influence of the size of the microgap on crestal bone changes around titanium implants. A histometric evaluation of unloaded non-submerged implants in the canine mandible. J Periodontol. 2001;72:1372–1383. doi: 10.1902/jop.2001.72.10.1372. [DOI] [PubMed] [Google Scholar]
- 14.Misch CE. Generic root form component terminology. In: Misch CE, editor. Contemporary implant dentistry. 3rd ed. St Louis (MO): Mosby; 2008. p. 2638. [Google Scholar]
- 15.Schwarz F, Alcoforado G, Nelson K, Schaer A, Taylor T, Beuer F, et al. Impact of implant-abutment connection, positioning of the machined collar/microgap, and platform switching on crestal bone level changes. Camlog Foundation Consensus Report. Clin Oral Implants Res. 2014;25:1301–1303. doi: 10.1111/clr.12269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pieri F, Aldini NN, Marchetti C, Corinaldesi G. Influence of implant-abutment interface design on bone and soft tissue levels around immediately placed and restored single-tooth implants: a randomized controlled clinical trial. Int J Oral Maxillofac Implants. 2011;26:169–178. [PubMed] [Google Scholar]
- 17.Koo KT, Lee EJ, Kim JY, Seol YJ, Han JS, Kim TI, et al. The effect of internal versus external abutment connection modes on crestal bone changes around dental implants: a radiographic analysis. J Periodontol. 2012;83:1104–1109. doi: 10.1902/jop.2011.110456. [DOI] [PubMed] [Google Scholar]
- 18.Shin YK, Han CH, Heo SJ, Kim S, Chun HJ. Radiographic evaluation of marginal bone level around implants with different neck designs after 1 year. Int J Oral Maxillofac Implants. 2006;21:789–794. [PubMed] [Google Scholar]
- 19.Quirynen M, Naert I, van Steenberghe D. Fixture design and overload influence marginal bone loss and fixture success in the Brånemark system. Clin Oral Implants Res. 1992;3:104–111. doi: 10.1034/j.1600-0501.1992.030302.x. [DOI] [PubMed] [Google Scholar]
- 20.Prendergast PJ, Huiskes R. Microdamage and osteocyte-lacuna strain in bone: a microstructural finite element analysis. J Biomech Eng. 1996;118:240–246. doi: 10.1115/1.2795966. [DOI] [PubMed] [Google Scholar]
- 21.Becker W, Becker BE. Replacement of maxillary and mandibular molars with single endosseous implant restorations: a retrospective study. J Prosthet Dent. 1995;74:51–55. doi: 10.1016/s0022-3913(05)80229-x. [DOI] [PubMed] [Google Scholar]
- 22.Maeda Y, Satoh T, Sogo M. In vitro differences of stress concentrations for internal and external hex implant-abutment connections: a short communication. J Oral Rehabil. 2006;33:75–78. doi: 10.1111/j.1365-2842.2006.01545.x. [DOI] [PubMed] [Google Scholar]
- 23.Laurell L, Lundgren D. Marginal bone level changes at dental implants after 5 years in function: a meta-analysis. Clin Implant Dent Relat Res. 2011;13:19–28. doi: 10.1111/j.1708-8208.2009.00182.x. [DOI] [PubMed] [Google Scholar]
- 24.Vigolo P, Zaccaria M. Clinical evaluation of marginal bone level change of multiple adjacent implants restored with splinted and nonsplinted restorations: a 5-year prospective study. Int J Oral Maxillofac Implants. 2010;25:1189–1194. [PubMed] [Google Scholar]
- 25.Vigolo P, Mutinelli S, Zaccaria M, Stellini E. Clinical evaluation of marginal bone level change around multiple adjacent implants restored with splinted and nonsplinted restorations: a 10-year randomized controlled trial. Int J Oral Maxillofac Implants. 2015;30:411–418. doi: 10.11607/jomi.3837. [DOI] [PubMed] [Google Scholar]
- 26.Guichet DL, Caputo AA, Choi H, Sorensen JA. Passivity of fit and marginal opening in screw- or cement-retained implant fixed partial denture designs. Int J Oral Maxillofac Implants. 2000;15:239–246. [PubMed] [Google Scholar]
- 27.Sailer I, Mühlemann S, Zwahlen M, Hämmerle CH, Schneider D. Cemented and screw-retained implant reconstructions: a systematic review of the survival and complication rates. Clin Oral Implants Res. 2012;23(Suppl 6):163–201. doi: 10.1111/j.1600-0501.2012.02538.x. [DOI] [PubMed] [Google Scholar]
- 28.Zechner W, Watzak G, Gahleitner A, Busenlechner D, Tepper G, Watzek G. Rotational panoramic versus intraoral rectangular radiographs for evaluation of peri-implant bone loss in the anterior atrophic mandible. Int J Oral Maxillofac Implants. 2003;18:873–878. [PubMed] [Google Scholar]
- 29.Kullman L, Al-Asfour A, Zetterqvist L, Andersson L. Comparison of radiographic bone height assessments in panoramic and intraoral radiographs of implant patients. Int J Oral Maxillofac Implants. 2007;22:96–100. [PubMed] [Google Scholar]
- 30.Fickl S, Zuhr O, Stein JM, Hürzeler MB. Peri-implant bone level around implants with platform-switched abutments. Int J Oral Maxillofac Implants. 2010;25:577–581. [PubMed] [Google Scholar]
- 31.Cappiello M, Luongo R, Di Iorio D, Bugea C, Cocchetto R, Celletti R. Evaluation of peri-implant bone loss around platform-switched implants. Int J Periodontics Restorative Dent. 2008;28:347–355. [PubMed] [Google Scholar]
- 32.Maeda Y, Miura J, Taki I, Sogo M. Biomechanical analysis on platform switching: is there any biomechanical rationale? Clin Oral Implants Res. 2007;18:581–584. doi: 10.1111/j.1600-0501.2007.01398.x. [DOI] [PubMed] [Google Scholar]
- 33.Padial-Molina M, Suarez F, Rios HF, Galindo-Moreno P, Wang HL. Guidelines for the diagnosis and treatment of peri-implant diseases. Int J Periodontics Restorative Dent. 2014;34:e102–11. doi: 10.11607/prd.1994. [DOI] [PubMed] [Google Scholar]
- 34.Sanz M, Chapple IL. Working Group 4 of the VIII European Workshop on Periodontology. Clinical research on peri-implant diseases: consensus report of Working Group 4. J Clin Periodontol. 2012;39(Suppl 12):202–206. doi: 10.1111/j.1600-051X.2011.01837.x. [DOI] [PubMed] [Google Scholar]
- 35.Sadowsky SJ. The implant-supported prosthesis for the edentulous arch: design considerations. J Prosthet Dent. 1997;78:28–33. doi: 10.1016/s0022-3913(97)70084-2. [DOI] [PubMed] [Google Scholar]
- 36.Heckmann SM, Winter W, Meyer M, Weber HP, Wichmann MG. Overdenture attachment selection and the loading of implant and denture-bearing area. Part 2: a methodical study using five types of attachment. Clin Oral Implants Res. 2001;12:640–647. doi: 10.1034/j.1600-0501.2001.120613.x. [DOI] [PubMed] [Google Scholar]
- 37.Naert I, Duyck J, Vandamme K. Occlusal overload and bone/implant loss. Clin Oral Implants Res. 2012;23(Suppl 6):95–107. doi: 10.1111/j.1600-0501.2012.02550.x. [DOI] [PubMed] [Google Scholar]
- 38.Galindo-Moreno P, León-Cano A, Ortega-Oller I, Monje A, Suárez F. Prosthetic abutment height is a key factor in peri-implant marginal bone loss. J Dent Res. 2014;93:80S–5S. doi: 10.1177/0022034513519800. [DOI] [PMC free article] [PubMed] [Google Scholar]