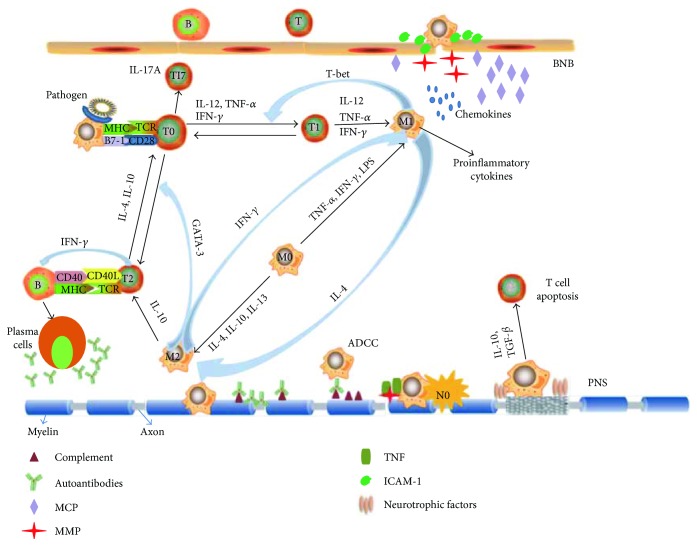
Figure 1.
Role of macrophages in the pathogenesis of EAN. Macrophages as the main professional antigen-presenting cells (APCs) by expressing MHC and costimulatory B7-molecules promote the polarization of T cells. Polarized Th1 cells drive macrophages to express a proinflammatory phenotype (M1). Proinflammatory cytokines from M1 macrophages in turn promote the Th1 responses via GATA-3 transcription, while anti-inflammatory cytokines from M2 macrophages facilitate the Th2 response via T-bet transcription. During disease progression of EAN, M1 macrophages contribute to breakdown the blood-nerve barrier (BNB) by releasing adhesion molecules, matrix metalloproteases (MMPs), and chemokines. Macrophages can directly attack myelin or indirectly cause demyelination by antibody-dependent cellular cytotoxicity (ADCC) or complement-dependent manner and releasing proinflammatory cytokines. In addition, nerve destruction occurs through nitric oxide (NO), MMPs, and other cytotoxic radicals. In the recovery phase of EAN, M2 macrophages contribute to remyelination and tissue repair through secreting anti-inflammatory cytokines such as IL-10 and tumor growth factor (TGF-β) and promoting T cell apoptosis.