Abstract
Background
Low-wage workers suffer disproportionately high rates of chronic disease and are important targets for workplace health and safety interventions. Child care centers offer an ideal opportunity to reach some of the lowest paid workers, but these settings have been ignored in workplace intervention studies.
Methods
Caring and Reaching for Health (CARE) is a cluster-randomized controlled trial evaluating efficacy of a multi-level, workplace-based intervention set in child care centers that promotes physical activity and other health behaviors among staff. Centers are randomized (1:1) into the Healthy Lifestyles (intervention) or the Healthy Finances (attention control) program. Healthy Lifestyles is delivered over six months including a kick-off event and three 8-week health campaigns (magazines, goal setting, behavior monitoring, tailored feedback, prompts, center displays, director coaching). The primary outcome is minutes of moderate and vigorous physical activity (MVPA); secondary outcomes are health behaviors (diet, smoking, sleep, stress), physical assessments (body mass index (BMI), waist circumference, blood pressure, fitness), and workplace supports for health and safety.
Results
In total, 56 centers and 553 participants have been recruited and randomized. Participants are predominately female (96.7%) and either Non-Hispanic African American (51.6%) or Non-Hispanic White (36.7%). Most participants (63.4%) are obese. They accumulate 17.4 ( ± 14.2) minutes/day of MVPA and consume 1.3 ( ± 1.4) and 1.3 ( ± 0.8) servings/day of fruits and vegetables, respectively. Also, 14.2% are smokers; they report 6.4 ( ± 1.4) hours/night of sleep; and 34.9% are high risk for depression.
Conclusions
Baseline data demonstrate several serious health risks, confirming the importance of workplace interventions in child care.
Keywords: Worksite, Worker health, Child care, Physical activity
1. Introduction
Chronic diseases are the leading cause of death and disability in the United States (US) [1]. In 2012, 117 million Americans - roughly half of all adults - had at least one of 10 chronic illnesses [2]. Low-wage workers are a particularly vulnerable population with disproportionately high rates of chronic disease [3–5] and lower life expectancies [6–8]. Child care staff are a sizable segment of this low-wage workforce including 1.3 million workers. Their median hourly wage is $9.77 (or $20,320 annually) – one of the lowest paid occupations in the US [9].
Little is known about the health of child care staff. In one large-scale survey among Pennsylvania Head Start staff, nearly three-quarters had one or more chronic health conditions; 15% rated their health as fair or poor; and 8.6 days of work were missed in the past year due to illness or injury [10]. A few smaller studies have demonstrated poor health habits (diet, physical activity, sleep) [11], high rates of overweight and obesity [11,12], and increased emotional distress [11,13]. Child care staff appear to suffer significant health risks that have been largely ignored [10].
Workplace health and safety programs hold great potential for addressing these health issues as such programs have been shown to have a positive impact on employee health (e.g., body mass index (BMI), cholesterol, blood pressure) and health behaviors (e.g., physical activity, diet) [14]. The US Guide to Community Preventive Services [15] notes “strong evidence” for the effectiveness of worksite-based physical activity and nutrition programs to reduce obesity.
Child care centers are small workplaces. As such, it may be easier to introduce program and policy changes, and their intimate culture may make it easier to encourage employee participation [16]. However, smaller workplaces are generally less likely to offer such programs or policies [17] due to limited resources and capacity [18,19]. There have been only one pilot and one quasi-experimental study attempting to intervene in child care settings to promote staff health [20,21]. The pilot study demonstrated significant improvements in BMI (−0.8 kg/m2, p < 0.001) [20]. In comparison, the quasi-experimental study demonstrated a significant decrease in sugar sweetened beverages only (−0.10 times/day vs. +0.33 times/day in intervention and controls, respectively, p-0.04) [21]. While differences in design and intervention approaches likely explain inconsistent findings, these studies begin to demonstrate the promise of child care-based worksite health and safety interventions.
Here, we describe Caring and Reaching for Health (CARE), an intervention study evaluating the effectiveness of a workplace-based, multi-level, intervention set in child care centers and designed to increase physical activity and improve other health behaviors among staff. This study is among the first of its kind, and will begin to address the gap in research on strategies to promote health among these low-wage workers. The SPIRIT (Standard Protocol Items: Recommendations for Interventional Trials) recommendations guided the reporting of study components [22,23]. Baseline demographics of the centers as well as behavioral and health indicators of child care staff are presented.
2. Methods
2.1. Study design and administration
CARE uses a cluster randomized controlled study design with two arms: intervention (Healthy Lifestyles) and attention control (Healthy Finances). The primary outcome is change in child care staff’s physical activity (minutes of moderate and vigorous physical activity (MVPA) per day) from baseline to post-intervention (6 months). Secondary outcomes include change in staff’s other health behaviors (e.g., diet, weight, smoking, sleep, stress); change in physical health indicators (e.g., body mass index (BMI), blood pressure, fitness tests); change in health programs, policies and support at the child care workplace; and staff’s practices related to child physical activity. Maintenance effects are also being assessed with a repeat of measures at 18 months (12 months post-intervention). Fig. 1 provides an overview of the study design. All study protocols have been registered at ClinicalTrials.gov (NCT02381938, registered on February 17, 2015). Protocols have been approved by the Institutional Review Board at The University of North Carolina at Chapel Hill with data and safety monitoring conducted regularly by the study’s data safety officer according to a preset data safety monitoring plan.
Fig. 1.
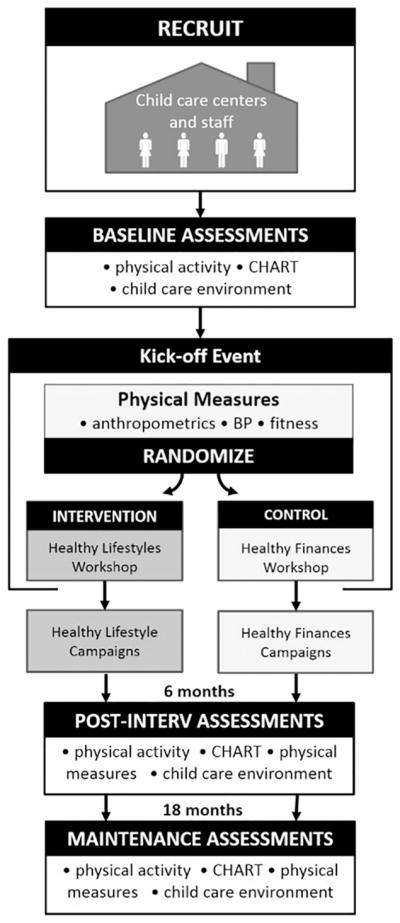
CARE study design.
2.2. Target sample, sample size, and recruitment
The target sample for this study consists of child care centers in central North Carolina and their staff. Based on our original power calculation, the sample size required for the study was 104 centers and 416 child care staff, which provided 80% power to detect an effect size of 0.30 using a two-sided test of significance and an alpha of 0.05. Selection of this effect size was based on a recent meta-analysis of physical activity interventions [24] and our own pilot data. The power calculation also accounted for clustering of staff within centers, which was assumed to include an average of four staff per center. Intra-class correlation associated with staff changes in physical activity, the primary outcome, was estimated at 0.02 based on our previous pilot work. The target sample size also assumed minimal attrition in child care centers (loss of 2 centers) and 10% attrition in child care staff (less than one staff per center). Monitoring of enrollment showed that both cluster size and rate of attrition were larger than originally assumed. On average, clusters included about 10 staff per center and there was about 10% attrition for centers and 20% attrition for staff. Based on these observations during early waves, a revised power calculation suggested a sample size of 58 centers (26 centers per arm +10% for attrition) and 580 child care staff needed to be enrolled to detect the same effect size.
Child care centers and staff were recruited in four waves (during 2015–2016) using a multi-phase recruitment strategy. Each wave targeted a one to three county geographic area. In the first phase of recruitment, we engaged local community partners who were in direct contact with child care centers. Where possible, these partners helped arrange informational sessions and invited local center directors to attend.
In the second phase, the research team initiated direct contact with local child care centers. These centers were identified from a publicly available online database of licensed child care programs available through the North Carolina Division of Child Development and Early Education [25]. Invitations were mailed (or emailed when available), after which research assistants followed up with telephone calls to confirm center eligibility, review study details, and assess interest. To be eligible for the study, centers were required to have at least four staff members (1 administrator and 3 other staff) willing to participate; and, have been in business for at least 2 years with no plans to close in the next 18 months. Head Start Centers were not able to participate because they operate for only 9 months of the year and would therefore close during some point in the study.
The third recruitment phase involved onsite visits to the centers. These visits were scheduled once center eligibility was confirmed and required staff participation was assured. During this visit, a research assistant met with interested staff individually to confirm eligibility, review study details, and collect informed consent. To participate, staff were required to be at least 18 years old, able to read and speak English, and able to pass a physical activity readiness screening [26] or obtain medical approval to take part in the study.
2.3. Randomization
Randomization took place following baseline data collection. For a center to be eligible for randomization, one administrator and at least two staff members from the center had to attend a kick-off event. Following the kick-off event’s morning activities (where basic health information was provided and fitness-related measures obtained), center directors drew one envelope from a bowl (bowl contained one envelope for each center expected to attend that day) to reveal results of their randomization. Envelopes were numbered sequentially with a card inside that has a coded randomization assignment (1 = Healthy Lifestyles, 2 = Healthy Finances) created from a computer-generated randomization table using a block randomization approach. The block size was set to two to ensure balance between study arms for each wave due to a possibility of enrolling small number of centers at a given wave.
2.4. Intervention description
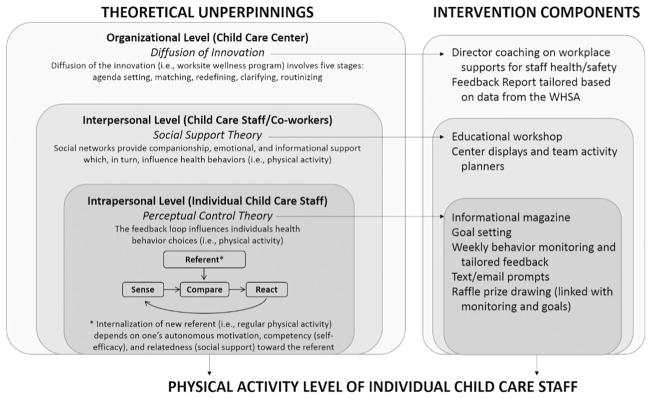
2.4.1. Theoretical underpinnings and conceptual model
The conceptual model for this study (Fig. 2) is based on the social ecological framework [27,28] and integrates theoretical models operating at intrapersonal (child care staff), interpersonal (team interactions), and organizational (child care centers’ programs, policies and environmental supports) levels to inform intervention strategies. At the intrapersonal level, intervention strategies are informed by Perceptual Control Theory [29] which suggests people are constantly perceiving their current condition, comparing it against some referent, and adjusting their behavior in order to bring their current condition closer to this referent – a process known as the “feedback loop”. The intervention’s use of goal setting, self-monitoring, and weekly tailored feedback are intended to facilitate this feedback loop. In addition, several behavior change techniques [30] are used to help motivate and reinforce individuals’ behavior change, including incentive and rewards, behavior practice and substitution, and action planning. At the interpersonal level, intervention strategies are informed by Social Support Theory [31]. Messages are incorporated into tailored feedback and magazine material that encourage engagement in “team” physical activities and foster social support (companionship, emotional, and informational). At the organizational level, Diffusion of Innovation Theory [32] guides the strategies employed to promote the adoption and implementation of the workplace health promotion intervention (e.g. the innovation) by child care centers. Behavior change techniques include feedback on current practices, goal setting, and action planning, all of which are provided through ongoing technical assistance to support diffusion of this innovation and organizational level change at each child care center.
Fig. 2.
CARE study conceptual model.
2.4.2. Healthy Lifestyles program
The Healthy Lifestyles program (intervention arm) is delivered over six months, starting with a half-day kick-off event, including a health and wellness fair (morning) and an educational workshop (afternoon), followed by three consecutive 8-week health and wellness campaigns. The kick-off event is open to all participating child care staff (at least one administrator and two staff per center are required to attend for the center to be randomized). Centers randomized into the intervention arm attend the educational workshop held that afternoon. The workshop is facilitated by the study interventionist and provides an introduction to the benefits of a healthy lifestyle, health behavior targets (comparing current behaviors to recommendations), basics of the program, and how it will be implemented at the center. Content throughout the intervention focuses primarily on physical activity promotion and secondarily on other health behaviors (e.g., diet, weight management, tobacco cessation, sleep, stress management). The integration of the primary and secondary topics are illustrated by the three campaign themes, which are: 1) Every Little Move Counts!, 2) Balance Your Menu with Movement, and 3) Moving for a Healthy Life. Each campaign includes an informational magazine, goal setting, weekly behavior monitoring, weekly tailored feedback, weekly text/email prompts, and a prize raffle linked to self-monitoring and goal attainment, which are designed to work together drive the feedback loop operating at the intrapersonal level. To help center staff get started with each campaign, research assistants visit each center during the first week to deliver materials, help with setting goals, and troubleshoot barriers to using the online tools, specifically focusing on staff who have not logged in to set goals or begin behavior monitoring. In addition, center-level displays and team activity planners accompany each campaign to promote social support for healthier behavior at the interpersonal level.
To support center-level change, directors receive technical assistance and coaching from the interventionist at the end of each campaign (week 7 or 8). The first coaching contact is in-person, and the remaining two are by telephone. Information from the Workplace Health and Safety Assessment (collected as part of baseline measures) is used to create a tailored Director Feedback Report, which is reviewed and expanded upon during the coaching sessions. Guided by the five stages of innovation process, the interventionist works with the director to review successes, troubleshoot challenges, and suggest changes that the director can make to establish additional administrative, programmatic, policy, or environmental supports for staff health to aid implementation and sustainability of their efforts to promote staff well-being. To encourage social support within the organization, the interventionist works with the director to strategize about group activities to support employees’ achievement of the Healthy Lifestyles program goals. Finally, relating to the concept of “wellness champions,” directors are asked to identify who at their center might be able to help organize staff health activities during the Healthy Lifestyles program and into the future once the program has ended.
2.4.3. Healthy Finances program
The Healthy Finances program (attention control arm) is structured similarly to the Healthy Lifestyles program. The program lasts six months, starts with a kick-off event, and includes three campaigns. However, content focuses on personal financial health and organizational financial success – topics that appeal to both low-wage workers, like child care staff, and businesses with low profit margins, like child care centers. During the afternoon of the kick-off event (following randomization), there is an educational workshop for staff focused on good financial practices, basics of the program, and how it will be implemented at their centers. The three campaign themes are: 1) Keys to Financial Fitness, 2) Keys to Growing Your Money, and 3) Keys to Making Credit Work for You. Each campaign includes an informational magazine, weekly prompts and tips delivered via text message or e-mail, two online quizzes to assess knowledge, and a prize raffle linked to taking the online quizzes. A webinar offered during each campaign introduces strategies that can help center directors build a successful business (e.g., bookkeeping, budgeting, marketing, managing legal risks). Materials and content focus on finances and avoid discussion of physical activity and other health behaviors. Use of an attention control was included to help maintain interest of center staff in the control arm and reduce the potential for dropouts. The focus on financial topics, and avoidance of physical activity among other health behavior topics, minimizes any contamination of the control arm. Additional details of the Healthy Lifestyles and the Healthy Finances programs will be described elsewhere.
2.5. Data collection and measures
Child care center directors and participating staff complete a series of assessments at three time points: baseline, post-intervention (immediately following the 6-month intervention), and maintenance (18 months, or 12 months after post-intervention). Data are collected during an onsite center visit and during the morning portion of the kick-off event (baseline only). Data collectors are trained and certified on protocols and blinded to center group assignment. Data collection tools use a combination of an objective physical activity measure, physical measurements, web-based and paper-based surveys, and an environmental assessment. Measures are described below.
2.5.1. Objective physical activity measure
The primary outcome for this study is minutes of moderate to vigorous physical activity (MVPA) per day measured by accelerometry. ActiGraph GT3X (ActiGraph, LLC, Pensacola, FL) monitors are programmed to sample at 30 Hz. Participating staff wear the monitor over the right hip (via an adjustable belt) for 7 consecutive days, 24 h a day, except when bathing or participating in water activities. Monitors are distributed during the onsite center visit and returned via postal mail. Data from the monitor are downloaded using ActiLife software (ActiGraph, LLC, Pensacola, FL) and adult-specific cut points are applied to determine minutes of sedentary (0–100 cpm), light (101–2019 cpm), moderate (≥2020 cpm), and vigorous (≥5999 cpm) physical activity [33,34] for participants with at least 8 h of wear time on a minimum of 4 days. In addition, minutes of lifestyle physical activity are estimated as time above 760 cpm [34].
2.5.2. Physical measures
Physical measurements, including height, weight, waist circumference, heart rate and blood pressure, are assessed during the onsite center visit using procedures guided by standard protocols [35,36]. Weight is measured to the nearest 0.1 pound with a Seca model 874 portable electronic scale (Seca Corporation, Columbia, MD), with shoes and excess clothing (e.g., coats) removed. Height is measured to the nearest 1/8 in. with a Shorr measuring board (Shorr Productions, Olney, MD), with shoes removed. Gulick II (Patterson Medical, Warrenville, IL) measuring tapes are used to measure waist circumference to the nearest 0.1 cm at the level of the iliac crest. The assessment of heart rate and blood pressure are obtained using an Omron HEM 907-XL digital blood pressure monitor (Omron, Kyoto, Japan) with participants sitting quietly with their legs uncrossed and feet flat on the floor. All measures are taken twice. Assuming reasonable agreement between the two measures (≤¼ inch for height, ≤1.0 pound for weight, ≤3.0 cm for waist circumference, < 5 mm Hg for systolic and diastolic blood pressure), the final measure is recorded as the average of the two values. Otherwise, a third measure is taken. Calculation of BMI (weight in kg/height in m2) is made from height and weight, which is then used to determine weight status (underweight = BMI < 18.5, normal weight = BMI 18.5–24.9, overweight = BMI 25.0–29.9, obese = BMI ≥30.0). Systolic and diastolic blood pressure are used to calculate mean arterial pressure.
In addition, a series of physical fitness assessments are used to assess cardiovascular fitness (six-minute walk test) [37], muscular strength and endurance (hand grip and chair sit and stand) [38–40], and balance (four-stage balance test also known as FICSIT-4) [41,42]. At baseline, these physical fitness assessments were collected during the morning portion of the kick-off event. At post-intervention, measures are collected during the onsite center visit.
2.5.3. Web-based surveys of health behaviors and psychosocial determinants
Health habits and potential mediating and moderating variables are assessed using a series of web-based surveys collected via an online system known as the Carolina Health Assessment and Research Tool (CHART) [43]. More specifically, CHART is used to assess current health behaviors (i.e., physical activity, diet, tobacco and e-cigarette use, sleep, and emotional health) and psychosocial determinants (i.e., self-efficacy, perceived barriers, readiness to change, and social support) of those behaviors.
Self-reported physical activity is assessed using a modified version of the International Physical Activity Questionnaire [44]. This 16-item survey asks participants to recall general physical activity, job-related physical activity, muscle strengthening activity, and sedentary time from the past seven days.
Dietary intake is assessed using a modified version of the Dietary Screener Questionnaire [45,46] and the Diet History Questionnaire [47]. This combined 27-item screener asks participants to recall the frequency of intake during the past month. Modifications include merging similar items (e.g., soda and sweetened fruit drinks), eliminating items (e.g., salsa, pizza, tomato sauce), and adding items that improve assessment of diet quality (e.g., dark green vegetables, eggs, lean meats, seafood, salty snacks, pre-made foods, and dining out). Within the diet screener, two items ask specifically about intake of fruits and fruit juice; three items asked about potatoes, beans and legumes, and other vegetables; two items ask about intake of sugar-sweetened and artificially-sweetened beverages; two items ask about intake of sweet and salty snacks; and one item asks about frequency of fast food and table-service restaurants. Responses in each group of items are summed to calculate total daily intake of fruits, vegetables, sweetened beverages, sweet and salty snacks, and frequency of fast food and table-service dining.
Tobacco and e-cigarette use is assessed using 12 items modified from the 2012 Behavioral Risk Factor Surveillance System Questionnaire [48] that estimates the average use during the past 30 days. Specific items are used to determine current smokers and those who have ever used e-cigarettes.
Sleep frequency and quality are assessed using one item from the Society for Behavioral Medicine’s Common Data Elements [49], plus two items from the Pittsburgh Sleep Quality Index [50]. Participants report on the typical number of hours of sleep per night in the past 30 days (sleep frequency) and sleep quality.
Emotional health is assessed using a combination of existing scales. A single item from the Society for Behavioral Medicine’s Common Data Elements [49] is used to measure distress, asking participants to rate their perceived level of distress during the past week on a scale of 0 to 10 (0 = no distress, 10 = extreme distress). Depressive symptoms are measured using the 20-item Center for Epidemiologic Studies Depression Scale [51]. Item responses (scored 0–3) are summed, as specified in standard scoring protocols, to create a total depressive symptom score (ranging from 0 to 60) with ≥16 indicating high risk of clinical depression. Emotional strain resulting from the job is assessed with 15 items derived from the Job Content Questionnaire [52], specifically extracting items related to job demand (five items, e.g. ‘My job requires working very fast’), job control (six items on skill discretion, e.g. ‘My job requires me to learn new things’, plus three items on decision authority, e.g. ‘I have a lot to say about what happens at my job’), and job insecurity (one item, i.e., ‘My job security is good’). Responses to these items range from one (strongly disagree) to four (strongly agree) and are reverse-coded when necessary. Modeled from existing scoring protocols [53], higher scores indicate more job demands (scores ranging from 5 to 20), less job control (scores ranging from 12 to 48), and higher job insecurity (0, 1). Lastly, five items from previous studies (i.e., FITShop [54] and WAY to Health [55]) are incorporated to capture additional detail about feelings of distress and job insecurity.
For each of the behaviors noted above, we also assess psychosocial determinants of these behaviors such as self-efficacy, perceived barriers, readiness to change, and social support. Where possible, previously validated scales are used. For example, the survey includes a 5-item assessment of physical activity self-efficacy [56], an adapted version of a 13-item assessment of barriers to exercise [57] (which drew from an unpublished scale by McAuley from 1990), an adapted version of a stages of exercise behavior change scale [56], and a physical activity social-support measure [58] modified for low-income women [59].
Lastly, CHART includes demographics surveys that capture participant characteristics (e.g., sex, age, race, ethnicity, household income, education, and role at the center). Center directors are asked questions about their center including years of operation, daily hours of operation, enrollment fees, number of children and employees, quality rating level (based on North Carolina’s Quality Rating and Improvement System where programs are rated 1–5 stars, with five stars being the highest rating), participation in the Child and Adult Care Food Program (CACFP, the federally-funded US program that provides reimbursement for meals and snacks served in child care programs that serve low-income families), accreditation from the National Association for the Education of Young Children (NAEYC), and enrollment fees.
2.5.4. Paper-based surveys
When necessary, certain surveys are administered in a paper format to limit administration to a specific segment of participants (e.g., child care staff with the role of classroom teachers) or to facilitate survey completion. For example, teacher-child interactions around physical activity are assessed only for participants identified as “teachers”. Items for this survey were adapted from the Environment and Policy Assessment and Observation instrument self-report form, a well-established measure of the child care environment [60]. We also use a 10-item measure of perceived management style [61] (autocratic vs. democratic), which assesses such factors as information flow patterns, decision-making style, communication style, methods of management (task or instrumental focus), and management structure. And finally, health literacy and numeracy are assessed using the 5-item Newest Vital Sign [62]. These complex constructs encompass many aspects of how individuals use health information and the health care system.
2.5.5. Environmental assessment
A Workplace Health and Safety Assessment (WHSA) is conducted using a combination of director interview and environmental observation. The WHSA was developed specifically for this study to ensure relevancy within child care; however, content development for items was guided by existing tools such as the Centers for Disease Control and Prevention’s Worksite Health Score Card [63] and Wisconsin’s Worksite Wellness Resource Kit [64], as well as protocols employed in the Working Well Trial [65]. The WHSA assesses five key elements of a comprehensive health promotion program (i.e., administrative supports, health education opportunities, environmental supports, linkages with other health programs, screening, and adequate follow-up) [17]. WHSA scoring uses items from the director interview and environmental observation to create summary scores for the following constructs: general infrastructure, behavior-specific organizational policies and practices, programs and promotions, internal physical environment, and internal social environment. Identification and categorization of items into these constructs was guided by a recent review of measurement instruments related to worksite environment and policy supports for energy balance [66]. While not part of the WHSA, similar questions were also developed, and incorporated into CHART, that assessed staff’s use of these workplace health and safety resources.
2.5.6. Process evaluation
Extensive process evaluation measures are being collected for each intervention component (kick-off event health fair, educational workshops, magazines, goal setting, self-monitoring, tailored feedback, text/email prompts, campaign raffles, center displays, director technical assistance and coaching) using observation tools, director and staff surveys, and project records. Process evaluation data will be used to assess reach, dose delivered, fidelity, dose received, and context (when relevant) following established protocols [67]. These data will also be used to understand outcome evaluation results, including whether there is a critical level of participation needed or whether certain components are more important in driving behavior change.
2.5.7. Cost effectiveness
A cost-effectiveness analysis is being conducted using well-established methods [68–71]. The evaluation takes the perspective of a community organization, since local organizations (e.g., technical assistance agencies working with child care programs) are the likely adopters and sponsors of this type of program in the future. All costs are tracked for each program component for each wave of implementation. While the primary outcome (minutes of MVPA) will be used to evaluate the program’s incremental cost effectiveness (i.e., cost per unit increase in MVPA), several standard measures will also be included. These standard measures include a single items about current perceived health status [72], the 5-item EQ-5D assessing health-related quality of life [73,74], and the 6-item Work Productivity and Activity Impairment questionnaire [75].
2.6. Statistical analysis
The primary analysis will evaluate the effect of the Healthy Lifestyles intervention by comparing the difference in mean changes in child care staff’s MVPA minutes per day between two study arms under an intent-to-treat principle. This analysis will be conducted using Generalized Linear Mixed Models (GLMM) that include a random intercept for centers to account for the clustering of staff within centers, and intervention and baseline MVPA minutes per day as fixed effects. Furthermore, additional GLMMs will be fit that 1) adjust for covariates identified a priori or differential dropout patterns detected, 2) test interaction terms between arms and covariates such as race, weight, and income to assess homogeneity of intervention effects in these subgroups, and 3) examine completers only. If necessary, missing data will be addressed using multiple imputation techniques [76] after determining whether data are missing not at random and estimate the effect of the intervention after removing selection77 bias ] and pattern [ mixture models to assess the sensitivity of our results to various assumptions of missing data patterns [77]. Differences in the secondary outcomes, such as staff health behaviors (e.g., weight, diet, sleep, smoking, emotional health), center level supports for staff health and safety, and staff physical activity practices employed with children will be analyzed in a parallel fashion. Mediating and moderating effects of the factors mentioned above will also be explored.
3. Results
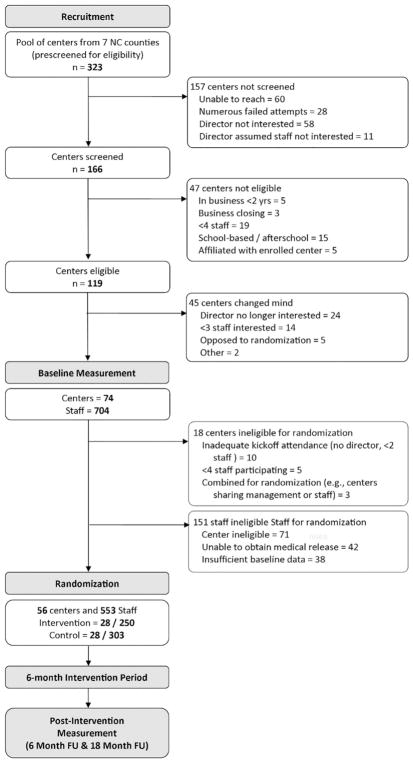
The study has completed all four waves of participant recruitment, successfully randomizing a total of 56 centers and 553 participants. Fig. 3 presents the CONSORT diagram for the study, starting with the identification of a pool of centers for recruitment and continuing through the randomization of centers and staff. Baseline descriptive statistics on center and participant demographic characteristics and participant health and behavioral indicators are presented in Tables 1–3 and described below.
Fig. 3.
CONSORT diagram for the CARE study.
Table 1.
Characteristics of the child care center participating in the CARE study (n = 56).
| n (%) | mean (SD) | |
|---|---|---|
| Years in operation | 18.3 (11.9) | |
| Hours per day of operation | 12.9 (3.0) | |
| Enrollment fee ($/week) | 141.7 (18.7) | |
| Size | ||
| # of children | 66.4 (35.9) | |
| # of employees | 14.7 (9.2) | |
| Star rating | 4.3 (0.7) | |
| Privately owned | 40 (71.4) | |
| Faith-based | 15 (26.8) | |
| Early Head Start | 1 (1.8) | |
| Accepts subsidies | 55 (98.2) | |
| Participates in CACFP | 49 (87.5) | |
| NAEYC accredited | 11 (19.6) | |
Table 3.
Baseline health characteristics and behaviors of participants in the CARE study (n = 553).
| n (%) | mean (SD) | |
|---|---|---|
| BMI (kg/m2) | 34.0 (8.9) | |
| Weight status | ||
| Underweight | 4 (0.7) | |
| Overweight | 132 (23.9) | |
| Obese | 350 (63.3) | |
| Body weight (kg) | 89.3 (24.5) | |
| Waist circumference (cm) | 105.4 (18.2) | |
| Heart rate (bpm) | 77.8 (12.0) | |
| Mean arterial pressure | 94.6 (13.6) | |
| Systolic blood pressure (mm Hg) | 123.4 (19.8) | |
| Diastolic blood pressure (mm Hg) | 80.3 (12.1) | |
| Physical fitness | ||
| 6 min walk (m) | 445.3 (80.2) | |
| Grip strength (kg) | 27.7 (9.2) | |
| Chair sit and stand (reps) | 15.1 (4.5) | |
| Balance | ||
| Completed phase 1 | 324 (100.0) | |
| Completed phase 2 | 323 (99.7) | |
| Completed phase 3 | 309 (95.7) | |
| Completed phase 4 | 250 (80.7) | |
| Physical activity | ||
| MVPA (minutes/day) | 17.4 (14.2) | |
| MVPA (minutes/week) | 123.7 (103.9) | |
| Meeting PA Guidelines (≥150 min/week) | 157 (29.4) | |
| Sedentary time (minutes/day) | 513.6 (75.0) | |
| Dietary intake | ||
| Fruit consumption (times/day) | 1.3 (1.4) | |
| Vegetable consumption (times/day) | 1.3 (0.8) | |
| Sweetened beverage consumption (times/day)# | 1.7 (1.8) | |
| Sweet and salty snack consumption (times/day) | 1.3 (1.7) | |
| Fast food or restaurant (times/day) | 0.3 (0.4) | |
| Cigarette use | ||
| Current cigarette smoker | 78 (14.2) | |
| Ever used e-cigarettes | 53 (9.6) | |
| Sleep (hours/night) | 6.4 (1.4) | |
| Sleep quality | ||
| Very bad | 30 (5.4) | |
| Fairly bad | 95 (17.2) | |
| Fairly good | 359 (65.2) | |
| Very good | 67 (12.2) | |
| Perceived level of distress ± | 4.0 (2.8) | |
| CES-D | 13.9 (9.3) | |
| CES-D ≥16 | 192 (34.9) | |
3.1. Child care center demographics
Center-level demographics for the 56 participating centers (n = 28 in Healthy Lifestyles and n = 28 in Healthy Finances) are presented in Table 1. Centers, on average, had been in business for 18.3 ( ± 11.9) years, serve approximately 66.4 ( ± 35.9) children and employ 14.7 ( ± 9.2) staff. Overall, centers meet high quality standards, averaging 4.3 ( ± 0.7) out of a possible 5 stars. Most centers are privately owned (71.4%), accept subsidies (98.2%), and participate in CACFP (87.5%).
3.2. Participant demographics
Demographic characteristics of the 553 participants (n = 250 in Healthy Lifestyles and n = 303 in Healthy Finances) are presented in Table 2. Participants are largely female (96.7%) and on average 40.5 ( ± 13.1) years old. Most participants are non-Hispanic African American (51.6%) or non-Hispanic White (36.7%), and few are Hispanic (6.2%). About three-quarters (75.2%) of the sample have an Associate’s degree or less. Roughly half (52.2%) of participants are married or living with a partner, with an average household size of 3.2 ( ± 1.6). Of this sample, 39.9% report an annual household income of $20,000 or less; and 77.4% of participants report that they have health insurance. Most (81.7%) of the study participants are classified as staff (vs. administrators).
Table 2.
Demographic characteristics of participants in the CARE study (n = 553).
| n (%) | mean (SD) | |
|---|---|---|
| Female | 534 (96.7) | |
| Age (years) | 40.5 (13.1) | |
| Race and ethnicity | ||
| Non-Hispanic White | 202 (36.7) | |
| Non-Hispanic African American | 284 (51.6) | |
| Non-Hispanic Other | 30 (5.5) | |
| Hispanic | 34 (6.2) | |
| Household income (annual) | ||
| < $10K | 49 (8.9) | |
| $10–15K | 78 (14.1) | |
| $15–20K | 93 (16.9) | |
| $20–25K | 61 (11.1) | |
| $25–35K | 73 (13.2) | |
| $35–50K | 66 (12.0) | |
| $50–75K | 36 (6.5) | |
| $75K | 37 (6.7) | |
| prefer not to answer | 59 (10.7) | |
| Highest level of education | ||
| High school diploma/GED | 66 (12.0) | |
| Some college | 205 (37.1) | |
| Associate’s degree | 144 (26.1) | |
| Bachelor’s degree | 113 (20.5) | |
| Graduate, MS, or higher | 24 (4.4) | |
| Married/Living with a partner | 288 (52.2) | |
| # in household | 3.2 (1.6) | |
| Health insured | 427 (77.4) | |
| Employee role at center | ||
| Administrator | 101 (18.3) | |
| Staff | 452 (81.7) | |
3.2.1. Participants’ physical measures of health and fitness
On average, participants have a BMI of 34.0 ( ± 8.9) kg/m2, with 23.9% of the sample classified as overweight and 63.3% as obese. Mean waist circumference was 105.4 ( ± 18.2) cm, which is well above the 80 cm cut-point associated with disease risk in women [78]. Elevated blood pressure (≥140/90 mm Hg) was observed among 26.5% of the sample.
Fitness tests showed that participants walked an average distance of 445.3 m ( ± 80.2) during the six-minute walk test, which is about 100 m shorter than distances observed in a multi-country sample of adult females [79]. In terms of strength, participants had on average a hand grip strength of 27.6 ( ± 9.2) kg, similar to normative data for similarly-aged women [80]. They also completed an average of 15.1 ( ± 4.5) repetitions of the chair sit and stand test, indicating average strength and endurance [40]. In terms of balance, 80.7% of participants successfully completed all four phases of the balance test.
3.2.2. Participants’ health behaviors
Participants accumulated, on average, 17.4 ( ± 14.2) minutes per day of MVPA (or 123.6 ( ± 104.0) min per week); hence, only 29.2% met the physical activity guideline for 150 min per week of MVPA [81]. Meanwhile, participants accumulated 513.8 ( ± 75.0) minutes per day (over 8 h) of sedentary time. Average frequency of fruit and vegetable consumption was 1.3 ( ± 1.4) and 1.3 ( ± 0.8) times per day, respectively, suggesting that participants fall short of the 4–5 cups per day that is recommended [82]. At the same time, participants regularly consumed sweetened beverages, averaging 1.7 ( ± 1.8) times per day, and regularly ate sweet and salty snacks, averaging 1.3 ( ± 1.7) times per day. Eating from fast food and table-service restaurants was also common, averaging 0.3 ( ± 0.4) times per day (or 2.1 times per week when multiplied by 7 days). Overall, 14.2% of staff were current cigarette smokers, and 9.6% had used e-cigarettes. Participants reported sleeping, on average, 6.4 ( ± 1.4) hours each night, which again is below the 7–9 h per night that is recommended [83]. Participants reported a distress level of 4.0 ( ± 2.8), on a scale of 0–10 where lower scores indicate lower distress. Participants scored, on average, 13.9 (± 9.3) on the depression scale; 34.9% had scores ≥16, indicating high risk for depression.
4. Discussion
The CARE study addresses an important gap in the current work-place health and safety literature by evaluating an innovative, child care-based, multi-level intervention designed to promote increased physical activity and improved health behaviors among child care staff. Child care staff, most of whom are low-wage workers, represent a population at high-risk for chronic disease. Hence, child care settings offer excellent places to reach a high need population working in demanding environments and introduce programs that help improve staff well-being. Unfortunately, child care staff and child care settings (e.g., centers) have been largely absent in workplace health and safety literature. To our knowledge, only one pilot study with six Head Start centers [20] and one quasi-experimental controlled trial conducted in 13 centers in California [21] have evaluate a child care-based health promotion program targeting child care staff. Thus, the CARE study represents the first randomized control trial evaluating the impact of a workplace health and safety intervention delivered at the child care setting.
Baseline data from this study confirm the importance of intervening with child care staff. We found that overweight/obesity levels among these child care staff were quite high (87%) compared to the national average (66%) [84]. In a study of Head Start staff in Texas, 79% of their sample was overweight or obese [12]. These rates are similar to those we recently reported among a sample of family child care home providers, individuals who care for children in their own homes, with > 90% of these women being classified as overweight or obese [11]. Using accelerometer-measured physical activity, nearly 30% of staff met physical activity guidelines; however, a large majority did not obtain sufficient physical activity even though their job responsibilities potentially included physical demands. Other health issues, such a lower consumption of fruits and vegetables, regular consumption of sweetened beverages and sweet and salty snacks, cigarette use, and lack of sleep, may also compromise the health of these workers.
In addition to these poor lifestyle habits, the health of child care staff is also threatened by low wages and challenging working conditions. Forty percent of participants reported an annual household income of $20,000 or less, indicating that many are living in poverty. These data are not surprising given that child care is one of the lowest paid occupations in the US [9]. Scores on the depression scale also speak to the challenges to their mental health, for which their stressful work environment is a likely contributor. A previous analysis of data from this study found that child care staff work long hours and report high job strain [85]. Previous research has shown that day-to-day child care staff must deal with challenges like working alone (limited contact with other adults), managing children’s misbehaviors and emotions (e.g., tantrums), and confronting pressures to ensure that children achieve [86]. In addition to these stressors, child care staff are also frequently exposed to infectious diseases and physical injuries [86]. Creating a healthy work environment in the child care centers requires a comprehensive approach with strategies that improve not only access to health and safety programming, but also improve wages, increase access to health insurance, and build healthy interactions between workers-center administrators [87,88].
While workplace health promotion is well-recognized as an effective strategy for improving health habits [14] and reducing weight among employees [89], child care centers represent a unique setting with specific opportunities and challenges. First, child care settings offer an important opportunity to provide access to health promotion programs for these low-income workers. Workplace health promotion programs have been identified as an important strategy for addressing disparities in health and chronic disease among low-wage workers [90,91]. Recent calls to action for child care settings to be a part of health promotion efforts for children [92–94] might provide some needed momentum. The health behaviors and attitudes of child care staff, including discomfort with their own physical abilities, dislike of healthier foods, and a lack of knowledge about physical activity and nutrition, impairs staff’s ability to be healthy role models for young children [12,95]. Hence, health promotion initiatives for children would likely be enhanced if staff well-being were also addressed. A notable challenge is the small size of most child care workplaces. Smaller workplaces are less likely to provide health promotion programming, policies, or environmental supports for their employees [16,17]. Given the fact that child care centers employ low-wage workers who are higher risk and that healthier staff are healthier role models for children, efforts are needed to find effective strategies for promoting health within these settings.
The CARE study has many strengths in both its design and the measures employed. Our cluster randomized controlled study design allows us to test the efficacy of the Healthy Lifestyles intervention in improving health behaviors, especially moderate to vigorous physical activity, our primary outcome. The use of accelerometers to assess physical activity, in combination with self-reported physical activity measures, is the gold standard for physical activity measurement and is preferred over self-reported measures alone [96]. In addition, our accelerometry output data can provide us with information about the number of steps taken as well as minutes of sedentary, light, moderate, and vigorous physical activity [33]. In addition to measuring the impact of our intervention on physical activity, our study will assess impact on a large number of health and behavioral outcomes, allowing us to explore the possible carryover effect to other health behaviors and outcomes. The “gateway” hypothesis [97] suggests that experiencing positive changes with physical activity could enhance one’s self-efficacy, motivation, and awareness to engage in other health behaviors. With the CARE study, the simultaneous measurement of multiple health behaviors at several time points will allow us to test whether (or not) physical activity acts as a gateway health behavior that triggers other healthy behaviors, such as healthy eating [98]. Also, this study will be among the first to investigate the work environment at child care settings including an evaluation of job strain and health promotion characteristics of these centers. Because of the important role child care staff play in the care of young children, it is critical to understand their health challenges and opportunities for health promotion.
5. Conclusions
The CARE study represents the first randomized controlled trial designed to promote physical activity, other health behaviors and create a supportive work environment for a diverse sample of low-wage child care center staff. If proven effective, this comprehensive multilevel intervention has the potential to be disseminated to child care centers throughout North Carolina and nationally.
Acknowledgments
The investigators and study team would like to acknowledge and thank the child care centers participating in this project, our many community partners, and the dedicated research staff who are implementing these protocols.
Funding
This work was supported by the National Heart, Lung, and Blood Institute (R01-HL119568). This project was conducted out of the Center for Health Promotion and Disease Prevention at The University of North Carolina at Chapel Hill (UNC), which is a Prevention Research Center funded through a Cooperative Agreement with the Centers for Disease Control and Prevention (U48-DP005017). The project also engaged the services of the CHAI Core, which is part of the UNC Nutrition Obesity Research Center funded by the National Institutes of Health (P30-DK056350). The findings and conclusions in this article are those of the authors and do not necessarily represent the official position of the funders.
Abbreviations
- BMI
body mass index
- CACFP
Child and Adult Care Food Program
- CARE
Caring and Reaching for Health
- CHART
Carolina Health Assessment and Research Tool
- GLMM
Generalized Linear Mixed Models
- MVPA
moderate to vigorous physical activity
- NAEYC
National Association for the Education of Young Children
- US
United States
- WHSA
Workplace Health and Safety Assessment
Contributor Information
Dianne S. Ward, Email: dsward@email.unc.edu.
Amber E. Vaughn, Email: avaughn@email.unc.edu.
Derek Hales, Email: derekh@email.unc.edu.
Anthony J. Viera, Email: anthony.viera@duke.edu.
Ziya Gizlice, Email: ziya_gizlice@unc.edu.
Lori A. Bateman, Email: lbateman@email.unc.edu.
Anna H. Grummon, Email: agrummon@live.unc.edu.
Gabriela Arandia, Email: arandia@live.unc.edu.
Laura A. Linnan, Email: linnan@email.unc.edu.
References
- 1.Heron M. Deaths: leading causes for 2012. Natl Vital Stat Rep. 2015;64(10):1–93. [PubMed] [Google Scholar]
- 2.Ward BW, Schiller JS, Goodman RA. Multiple chronic conditions among US adults: a 2012 update. Prev Chronic Dis. 2014;11:E62. doi: 10.5888/pcd11.130389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kanjilal S, Gregg EW, Cheng YJ, Zhang P, Nelson DE, Mensah G, Beckles GL. Socioeconomic status and trends in disparities in 4 major risk factors for cardiovascular disease among US adults, 1971–2002. Arch Intern Med. 2006;166(21):2348–2355. doi: 10.1001/archinte.166.21.2348. [DOI] [PubMed] [Google Scholar]
- 4.Diez Roux AV, Chambless L, Merkin SS, Arnett D, Eigenbrodt M, Nieto FJ, Szklo M, Sorlie P. Socioeconomic disadvantage and change in blood pressure associated with aging. Circulation. 2002;106(6):703–710. doi: 10.1161/01.cir.0000025402.84600.cd. [DOI] [PubMed] [Google Scholar]
- 5.Kanervisto M, Vasankari T, Laitinen T, Heliovaara M, Jousilahti P, Saarelainen S. Low socioeconomic status is associated with chronic obstructive airway diseases. Respir Med. 2011;105(8):1140–1146. doi: 10.1016/j.rmed.2011.03.008. [DOI] [PubMed] [Google Scholar]
- 6.Clarke CA, Miller T, Chang ET, Yin D, Cockburn M, Gomez SL. Racial and social class gradients in life expectancy in contemporary California. Soc Sci Med. 2010;70(9):1373–1380. doi: 10.1016/j.socscimed.2010.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lin CC, Rogot E, Johnson NJ, Sorlie PD, Arias E. A further study of life expectancy by socioeconomic factors in the National Longitudinal Mortality Study. Ethn Dis. 2003;13(2):240–247. [PubMed] [Google Scholar]
- 8.Singh GK, Siahpush M. Widening socioeconomic inequalities in US life expectancy, 1980–2000. Int J Epidemiol. 2006;35(4):969–979. doi: 10.1093/ije/dyl083. [DOI] [PubMed] [Google Scholar]
- 9.Bureau of Labor Statistics, U.S. Department of Labor. [Assessed May 10 2017];Occupational Outlook Handbook, 2016–17 Edition. https://www.bls.gov/ooh/personal-care-and-service/childcare-workers.htm.
- 10.Whitaker RC, Becker BD, Herman AN, Gooze RA. The physical and mental health of head start staff: the Pennsylvania head start staff wellness survey, 2012. Prev Chronic Dis. 2013;10:E181. doi: 10.5888/pcd10.130171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tovar A, Vaughn AE, Grummon A, Burney R, Erinosho T, Ostbye T, Ward DS. Family child care home providers as role models for children: cause for concern? Prev Med Rep. 2017;5:308–313. doi: 10.1016/j.pmedr.2016.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sharma S, Dortch KS, Byrd-Williams C, Truxillio JB, Rahman GA, Bonsu P, Hoelscher D. Nutrition-related knowledge, attitudes, and dietary behaviors among head start teachers in Texas: a cross-sectional study. J Acad Nutr Diet. 2013;113(4):558–562. doi: 10.1016/j.jand.2013.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Baldwin D, Gaines S, Wold JL, Williams A, Leary J. The health of female child care providers: implications for quality of care. J Community Health Nurs. 2007;24(1):1–17. doi: 10.1080/07370010709336582. [DOI] [PubMed] [Google Scholar]
- 14.Osilla KC, Van Busum K, Schnyer C, Wozar Larkin J, Eibner C, Mattke S. Systematic review of the impact of worksite wellness programs. Am J Manag Care. 2012;18(2):e68–81. [PubMed] [Google Scholar]
- 15.Task Force on Community Preventive Services. Recommendations to increase physical activity in communities. Am J Prev Med. 2002;22(4 Suppl):67–72. doi: 10.1016/s0749-3797(02)00433-6. [DOI] [PubMed] [Google Scholar]
- 16.Harris JR, Hannon PA, Beresford SA, Linnan LA, McLellan DL. Health promotion in smaller workplaces in the United States. Annu Rev Public Health. 2014;35:327–342. doi: 10.1146/annurev-publhealth-032013-182416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Linnan L, Bowling M, Childress J, Lindsay G, Blakey C, Pronk S, Wieker S, Royall P. Results of the 2004 National Worksite Health Promotion Survey. Am J Public Health. 2008;98(8):1503–1509. doi: 10.2105/AJPH.2006.100313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nelson CC, Allen JD, McLellan D, Pronk N, Davis KL. Integrating health promotion and occupational safety and health in manufacturing worksites: perspectives of leaders in small-to-medium sized businesses. Work. 2015;52(1):169–176. doi: 10.3233/WOR-152038. [DOI] [PubMed] [Google Scholar]
- 19.Witt LB, Olsen D, Ablah E. Motivating factors for small and midsized businesses to implement worksite health promotion. Health Promot Pract. 2013;14(6):876–884. doi: 10.1177/1524839912472504. [DOI] [PubMed] [Google Scholar]
- 20.Herman A, Nelson BB, Teutsch C, Chung PJ. “Eat healthy, stay active!”: a coordinated intervention to improve nutrition and physical activity among head start parents, staff, and children. Am J Health Promot. 2012;27(1):e27–36. doi: 10.4278/ajhp.110412-QUAN-157. [DOI] [PubMed] [Google Scholar]
- 21.Gosliner WA, James P, Yancey AK, Ritchie L, Studer N, Crawford PB. Impact of a worksite wellness program on the nutrition and physical activity environment of child care centers. Am J Health Promot. 2010;24(3):186–189. doi: 10.4278/ajhp.08022719. [DOI] [PubMed] [Google Scholar]
- 22.Chan AW, Tetzlaff JM, Gotzsche PC, Altman DG, Mann H, Berlin JA, Dickersin K, Hrobjartsson A, Schulz KF, Parulekar WR, et al. SPIRIT 2013 explanation and elaboration: guidance for protocols of clinical trials. BMJ. 2013;346:e7586. doi: 10.1136/bmj.e7586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chan AW, Tetzlaff JM, Altman DG, Laupacis A, Gotzsche PC, Krleza-Jeric K, Hrobjartsson A, Mann H, Dickersin K, Berlin JA, et al. SPIRIT 2013 statement: defining standard protocol items for clinical trials. Ann Intern Med. 2013;158(3):200–207. doi: 10.7326/0003-4819-158-3-201302050-00583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Michie S, Abraham C, Whittington C, McAteer J, Gupta S. Effective techniques in healthy eating and physical activity interventions: a meta-regression. Health Psychol. 2009;28(6):690–701. doi: 10.1037/a0016136. [DOI] [PubMed] [Google Scholar]
- 25.North Carolina Division of Child Development and Early Education. [Accessed date: 10 May 2017];Child care facility search site. http://ncchildcaresearch.dhhs.state.nc.us.
- 26.Warburton DER, Jamnik VK, Bredin SSD, Gledhill N. The physical activity readiness questionnaire for everyone (PAR-Q+) and electronic physical activity readiness medical examination (ePARmed-X+) Health Fitness J Can. 2011;4(2):3–23. [Google Scholar]
- 27.Sallis JF, Owen N, Fisher EB. Ecological models of health behavior. In: Glantz K, Rimer BK, Viswanath K, editors. Health Behavior and Health Education: Theory, Research, and Practice. 4. Josey-Bass, John Wiley & Sons, Inc; 2008. pp. 465–486. [Google Scholar]
- 28.Stokols D, Allen J, Bellingham RL. The social ecology of health promotion: implications for research and practice. Am J Health Promot. 1996;10(4):247–251. doi: 10.4278/0890-1171-10.4.247. [DOI] [PubMed] [Google Scholar]
- 29.Powers WT. Behavior: The Control of Perception. Aldine Publishing Co; Chicago, IL: 1973. [Google Scholar]
- 30.Michie S, Richardson M, Johnston M, Abraham C, Francis J, Hardeman W, Eccles MP, Cane J, Wood CE. The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: building an international consensus for the reporting of behavior change interventions. Ann Behav Med. 2013;46(1):81–95. doi: 10.1007/s12160-013-9486-6. [DOI] [PubMed] [Google Scholar]
- 31.Israel BA. Social networks and social support: implications for natural helper and community level interventions. Health Educ Q. 1985;12(1):65–80. doi: 10.1177/109019818501200106. [DOI] [PubMed] [Google Scholar]
- 32.Rogers EM. Diffusion of Innovations. 5. Free Press; New York, NY: 1995. [Google Scholar]
- 33.Troiano RP, Berrigan D, Dodd KW, Masse LC, Tilert T, McDowell M. Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc. 2008;40(1):181–188. doi: 10.1249/mss.0b013e31815a51b3. [DOI] [PubMed] [Google Scholar]
- 34.Matthews CE, Chen KY, Freedson PS, Buchowski MS, Beech BM, Pate RR, Troiano RP. Amount of time spent in sedentary behaviors in the United States, 2003–2004. Am J Epidemiol. 2008;167(7):875–881. doi: 10.1093/aje/kwm390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Centers for Disease Control and Prevention. National Health and Nutrition Examination Survey (NHANES): Anthropometry procedures manual. Atlanta, GA: 2013. [Google Scholar]
- 36.Pickering TG, Hall JE, Appel LJ, Falkner BE, Graves J, Hill MN, Jones DW, Kurtz T, Sheps SG, Roccella EJ. Recommendations for blood pressure measurement in humans and experimental animals: part 1: blood pressure measurement in humans: a statement for professionals from the Subcommittee of Professional and Public Education of the American Heart Association Council on high blood pressure research. Hypertension. 2005;45(1):142–161. doi: 10.1161/01.HYP.0000150859.47929.8e. [DOI] [PubMed] [Google Scholar]
- 37.American Thoracic Society. Guidelines for the six-minute walk test. Am J Respir Crit Care Med. 2003;166:111–117. doi: 10.1164/ajrccm.166.1.at1102. [DOI] [PubMed] [Google Scholar]
- 38.Roberts HC, Denison HJ, Martin HJ, Patel HP, Syddall H, Cooper C, Sayer AA. A review of the measurement of grip strength in clinical and epidemiological studies: towards a standardised approach. Age Ageing. 2011;40(4):423–429. doi: 10.1093/ageing/afr051. [DOI] [PubMed] [Google Scholar]
- 39.Jones CJ, Rikli RE, Beam WC. A 30-s chair-stand test as a measure of lower body strength in community-residing older adults. Res Q Exerc Sport. 1999;70(2):113–119. doi: 10.1080/02701367.1999.10608028. [DOI] [PubMed] [Google Scholar]
- 40.Centers for Disease Control and Prevention. [Accessed date: 5 February 2015];The 30-second chair stand test. http://www.cdc.gov/homeandrecreationalsafety/pdf/steadi/30_second_chair_stand_test.pdf.
- 41.Rossiter-Fornoff JE, Wolf SL, Wolfson LI, Buchner DM. A cross-sectional validation study of the FICSIT common data base static balance measures. Frailty and Injuries: Cooperative Studies of Intervention Techniques. J Gerontol A Biol Sci Med Sci. 1995;50(6):M291–297. doi: 10.1093/gerona/50a.6.m291. [DOI] [PubMed] [Google Scholar]
- 42.Centers for Disease Control and Prevention. [Accessed date: 10 May 2017];The 4-stage balance test. https://www.cdc.gov/steadi/pdf/4-stage_balance_test-a.pdf.
- 43. [Accessed date: 10 May 2017];UNC Lineberger Comprehensive Cancer Center, What is CHART? https://chart.unc.edu.
- 44.Craig CL, Marshall AL, Sjostrom M, Bauman AE, Booth ML, Ainsworth BE, Pratt M, Ekelund U, Yngve A, Sallis JF, et al. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc. 2003;35(8):1381–1395. doi: 10.1249/01.MSS.0000078924.61453.FB. [DOI] [PubMed] [Google Scholar]
- 45.Thompson FE, Midthune D, Subar AF, McNeel T, Berrigan D, Kipnis V. Dietary intake estimates in the National Health Interview Survey, 2000: methodology, results, and interpretation. J Am Diet Assoc. 2005;105(3):352–363. doi: 10.1016/j.jada.2004.12.032. [DOI] [PubMed] [Google Scholar]
- 46.Thompson FE, Midthune D, Subar AF, Kahle LL, Schatzkin A, Kipnis V. Performance of a short tool to assess dietary intakes of fruits and vegetables, percentage energy from fat and fibre. Public Health Nutr. 2004;7(8):1097–1105. doi: 10.1079/PHN2004642. [DOI] [PubMed] [Google Scholar]
- 47.Block G, Woods M, Potosky A, Clifford C. Validation of a self-administered diet history questionnaire using multiple diet records. J Clin Epidemiol. 1990;43(12):1327–1335. doi: 10.1016/0895-4356(90)90099-b. [DOI] [PubMed] [Google Scholar]
- 48.Centers for Disease Control and Prevention. [Accessed date: 10 May 2017];Behavioral Risk Factor Surveillance System: BRFSS questionnaires. https://www.cdc.gov/brfss/questionnaires/index.htm.
- 49.Glasgow R, Emmons KM. The public health need for patient-reported measures and health behaviors in electronic health records: a policy statement of the Society of Behavioral Medicine. Transl Behav Med. 2011;1(1):108–109. doi: 10.1007/s13142-011-0017-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Buysse DJ, Reynolds CF, 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 51.Radloff LS. The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1(3):385–401. [Google Scholar]
- 52.Karasek R, Brisson C, Kawakami N, Houtman I, Bongers P, Amick B. The Job Content Questionnaire (JCQ): an instrument for internationally comparative assessments of psychosocial job characteristics. J Occup Health Psychol. 1998;3(4):322–355. doi: 10.1037//1076-8998.3.4.322. [DOI] [PubMed] [Google Scholar]
- 53.Landsbergis PA, Schnall PL, Pickering TG, Schwartz JE. Validity and reliability of a work history questionnaire derived from the Job Content Questionnaire. J Occup Environ Med. 2002;44(11):1037–1047. doi: 10.1097/00043764-200211000-00010. [DOI] [PubMed] [Google Scholar]
- 54.Linnan LA, Reiter PL, Duffy C, Hales D, Ward DS, Viera AJ. Assessing and promoting physical activity in African American barbershops: results of the FITStop pilot study. Am J Mens Health. 2011;5(1):38–46. doi: 10.1177/1557988309360569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Linnan L, Tate DF, Harrington CB, Brooks-Russell A, Finkelstein E, Bangdiwala S, Birken B, Britt A. Organizational- and employee-level recruitment into a worksite-based weight loss study. Clin Trials. 2012;9(2):215–225. doi: 10.1177/1740774511432554. [DOI] [PubMed] [Google Scholar]
- 56.Marcus BH, Selby VC, Niaura RS, Rossi JS. Self-efficacy and the stages of exercise behavior change. Res Q Exerc Sport. 1992;63(1):60–66. doi: 10.1080/02701367.1992.10607557. [DOI] [PubMed] [Google Scholar]
- 57.Resnick B, Jenkins LS. Testing the reliability and validity of the self-efficacy for exercise scale. Nurs Res. 2000;49(3):154–159. doi: 10.1097/00006199-200005000-00007. [DOI] [PubMed] [Google Scholar]
- 58.Sallis JF, Grossman RM, Pinski RB, Patterson TL, Nader PR. The development of scales to measure social support for diet and exercise behaviors. Prev Med. 1987;16(6):825–836. doi: 10.1016/0091-7435(87)90022-3. [DOI] [PubMed] [Google Scholar]
- 59.Eyler AA, Brownson RC, Donatelle RJ, King AC, Brown D, Sallis JF. Physical activity social support and middle- and older-aged minority women: results from a US survey. Soc Sci Med. 1999;49(6):781–789. doi: 10.1016/s0277-9536(99)00137-9. [DOI] [PubMed] [Google Scholar]
- 60.Ward DS, Mazzucca S, McWilliams C, Hales D. Use of the Environment and Policy Evaluation and Observation as a Self-Report Instrument (EPAO-SR) to measure nutrition and physical activity environments in child care settings: validity and reliability evidence. Int J Behav Nutr Phys Act. 2015;12:124. doi: 10.1186/s12966-015-0287-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Witte K. Managerial style and health promotion programs. Soc Sci Med. 1993;36(3):227–235. doi: 10.1016/0277-9536(93)90006-p. [DOI] [PubMed] [Google Scholar]
- 62.Weiss BD, Mays MZ, Martz W, Castro KM, DeWalt DA, Pignone MP, Mockbee J, Hale FA. Quick assessment of literacy in primary care: the newest vital sign. Ann Fam Med. 2005;3(6):514–522. doi: 10.1370/afm.405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Division for Heart Disease and Stroke Prevention. [Accessed date: 24 March 2017];The CDC Worksite Health ScoreCard: An Assessment Tool for Employees to Prevent Heart Disease, Stroke, and Related Conditions. http://www.cdc.gov/dhdsp/pubs/worksite_scorecard.htm.
- 64.Department of Health Services, Division of Public Health N. [Accessed date: 10 May 2017];Physical Activity and Obesity Program, Wisconsin Nutrition PAaOP, Worksite Wellness Resource Kit. https://www.dhs.wisconsin.gov/physical-activity/worksite/kit.htm.
- 65.Abrams DB, Boutwell WB, Grizzle J, Heimendinger J, Sorensen G, Varnes J. Cancer control at the workplace: the Working Well Trial. Prev Med. 1994;23(1):15–27. doi: 10.1006/pmed.1994.1003. [DOI] [PubMed] [Google Scholar]
- 66.Hipp JA, Reeds DN, van Bakergem MA, Marx CM, Brownson RC, Pamulapati SC, Hoehner CM. Review of measures of worksite environmental and policy supports for physical activity and healthy eating. Prev Chronic Dis. 2015;12:E65. doi: 10.5888/pcd12.140410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Steckler A, Linnan L, editors. Process Evaluation for Public Health Intervention and Research. Jossey-Bass Publishers, Inc; San Francisco: 2002. [Google Scholar]
- 68.Finkelstein EA, Khavjou O, Will JC. Cost-effectiveness of WISEWOMAN, a program aimed at reducing heart disease risk among low-income women. J Women’s Health (2002) 2006;15(4):379–389. doi: 10.1089/jwh.2006.15.379. [DOI] [PubMed] [Google Scholar]
- 69.Finkelstein EA, Linnan LA, Tate DF, Birken BE. A pilot study testing the effect of different levels of financial incentives on weight loss among overweight employees. J Occup Environ Med. 2007;49(9):981–989. doi: 10.1097/JOM.0b013e31813c6dcb. [DOI] [PubMed] [Google Scholar]
- 70.Finkelstein EA, Allaire BT, Dibonaventura MD, Burgess SM. Incorporating indirect costs into a cost-benefit analysis of laparoscopic adjustable gastric banding. Value Health. 2012;15(2):299–304. doi: 10.1016/j.jval.2011.12.004. [DOI] [PubMed] [Google Scholar]
- 71.de Lima Lopes G, Segel JE, Tan DSW, Do YK, Mok T, Finkelstein EA. Costeffectiveness of epidermal growth factor receptor mutation testing and first-line treatment with gefitinib for patients with advanced adenocarcinoma of the lung. Cancer. 2012;118(4):1029–1032. doi: 10.1002/cncr.26372. [DOI] [PubMed] [Google Scholar]
- 72.Idler EL, Benyamini Y. Self-rated health and mortality: a review of twenty-seven community studies. J Health Soc Behav. 1997;38(1):21–37. [PubMed] [Google Scholar]
- 73.EuroQol Group Association. [Accessed date: 10 May 2017];About EQ-5D. http://www.euroqol.org/about-eq-5d.html.
- 74.Brooks R, de Charro F, Rabin R, Kind R. EQ-5D Concepts and Methods: A Developmental History. Springer; Dordrecht: 2005. [Google Scholar]
- 75.Reilly MC, Zbrozek AS, Dukes EM. The validity and reproducibility of a work productivity and activity impairment instrument. PharmacoEconomics. 1993;4(5):353–365. doi: 10.2165/00019053-199304050-00006. [DOI] [PubMed] [Google Scholar]
- 76.Little R, Rubin D. Statistical Analysis With Missing Data. 2. John Wiley and Sons, Inc; Hoboken, NJ: 2002. [Google Scholar]
- 77.Molenberghs G, Kenward M. Missing Data in Clinical Studies. John Wiley and Sons, Ltd; West Sussex: 2007. [Google Scholar]
- 78.World Health Organization. Waist Circumference and Waist–hip ratio: Report of a WHO Expert Consultation; Geneva. 8–11 December 2008; Geneva, Switzerland: WHO Document Production Services; 2011. p. 39. [Google Scholar]
- 79.Casanova C, Celli BR, Barria P, Casas A, Cote C, de Torres JP, Jardim J, Lopez MV, Marin JM, Montes de Oca M, et al. The 6-min walk distance in healthy subjects: reference standards from seven countries. Eur Respir J. 2011;37(1):150–156. doi: 10.1183/09031936.00194909. [DOI] [PubMed] [Google Scholar]
- 80.Dodds RM, Syddall HE, Cooper R, Benzeval M, Deary IJ, Dennison EM, Der G, Gale CR, Inskip HM, Jagger C, et al. Grip strength across the life course: normative data from twelve British studies. PLoS One. 2014;9(12):e113637. doi: 10.1371/journal.pone.0113637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.U.S. Department of Health and Human Services. 2008 Physical Activity Guidelines for Americans. Washington, DC: 2008. p. 61. 2013. [Google Scholar]
- 82.U.S. Department of Agriculture. [Accessed date: 12 December 2016];MyPlate. https://www.choosemyplate.gov/MyPlate.
- 83.Ohayon MM, Wickwire EM, Hirshkowitz M, Albert SM, Avidan A, Daly FJ, Dauvilliers Y, Ferri R, Fung C, Gozal D, et al. National Sleep Foundation’s sleep quality recommendations: first report. Sleep Health. 2017;3(1):6–19. doi: 10.1016/j.sleh.2016.11.006. [DOI] [PubMed] [Google Scholar]
- 84.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA. 2014;311(8):806–814. doi: 10.1001/jama.2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Linnan L, Arandia G, Bateman LA, Vaughn A, Smith N, Ward D. The health and working conditions of women employed in child care. Int J Environ Res Public Health. 2017;14(3) doi: 10.3390/ijerph14030283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Gratz RR, Claffey A. Adult Health in Child Care: Health Status. Behaviors, and Concerns of Teachers, Directors, and Family Child Care Providers. 1996;11:243–267. [Google Scholar]
- 87.Hammer LB, Truxillo DM, Bodner T, Rineer J, Pytlovany AC, Richman A. Effects of a workplace intervention targeting psychosocial risk factors on safety and health outcomes. Biomed Res Int. 2015;2015:836967. doi: 10.1155/2015/836967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Odle-Dusseau HN, Hammer LB, Crain TL, Bodner TE. The influence of family-supportive supervisor training on employee job performance and attitudes: an organizational work-family intervention. J Occup Health Psychol. 2016;21(3):296–308. doi: 10.1037/a0039961. [DOI] [PubMed] [Google Scholar]
- 89.Task Force on Community Preventive Services. A recommendation to improve employee weight status through worksite health promotion programs targeting nutrition, physical activity, or both. Am J Prev Med. 2009;37(4):358–359. doi: 10.1016/j.amepre.2009.07.004. [DOI] [PubMed] [Google Scholar]
- 90.Baron SL, Beard S, Davis LK, Delp L, Forst L, Kidd-Taylor A, Liebman AK, Linnan L, Punnett L, Welch LS. Promoting integrated approaches to reducing health inequities among low-income workers: applying a social ecological framework. Am J Ind Med. 2014;57(5):539–556. doi: 10.1002/ajim.22174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Kneipp SM, Beeber LL, Linnan LA. Headache and health-related job loss among disadvantaged women. J Nurs Pract. 2014;10(5):316–324. doi: 10.1016/j.nurpra.2014.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Story M, Kaphingst KM, French S. The role of child care settings in obesity prevention. Futur Child. 2006;16(1):143–168. doi: 10.1353/foc.2006.0010. [DOI] [PubMed] [Google Scholar]
- 93.Institute of Medicine. Early Childhood Obesity Prevention Policies. The National Academies Press; Washington, DC: 2011. [Google Scholar]
- 94.American Academy of Pediatrics, American Public Health Association, National Resource Center for Health, Safety in Child Care and Early Education. Caring for our children: National health and safty performance standards, Guidelines for Early Care and Education Programs. 3. American Academy of Pediatrics; American Public Health Association; Elk Grove Village, IL; Washington, DC: 2011. [Google Scholar]
- 95.Hughes CC, Gooze RA, Finkelstein DM, Whitaker RC. Barriers to obesity prevention in Head Start. Health Aff (Millwood) 2010;29(3):454–462. doi: 10.1377/hlthaff.2009.0499. [DOI] [PubMed] [Google Scholar]
- 96.Ward DS, Evenson KR, Vaughn A, Rodgers AB, Troiano RP. Accelerometer use in physical activity: best practices and research recommendations. Med Sci Sports Exerc. 2005;37(11 Suppl):S582–588. doi: 10.1249/01.mss.0000185292.71933.91. [DOI] [PubMed] [Google Scholar]
- 97.Dutton GR, Napolitano MA, Whiteley JA, Marcus BH. Is physical activity a gateway behavior for diet? Findings from a physical activity trial. Prev Med. 2008;46(3):216–221. doi: 10.1016/j.ypmed.2007.12.012. [DOI] [PubMed] [Google Scholar]
- 98.Blakely F, Dunnagan T, Haynes G, Moore S, Pelican S. Moderate physical activity and its relationship to select measures of a healthy diet. J Rural Health. 2004;20(2):160–165. doi: 10.1111/j.1748-0361.2004.tb00023.x. [DOI] [PubMed] [Google Scholar]