Abstract
Objective
This study aimed to determine the incidence and analyze trends related to spinal diseases based on a national database in the Republic of Korea (ROK) and to elucidate the healthcare burden that will serve as a useful resource for researchers, clinicians, and patients.
Methods
This study was a retrospective analysis of data obtained from Healthcare Bigdata Hub, the Korean Statistical Information Service, and Open Data Portal from 2012 through 2016. The main disease codes for spinal diseases (M40–M54) were used for identification of these conditions.
Results
The overall annual incidence rates for spinal disease in the ROK was median 15,877 (men, 13,181; women, 18,588) per 100,000 population, and sex ratio was 1:1.41 (p<0.01). The incidence rate and annual costs per patient increased by 7.6% and 14.7% over 5 years continuously, respectively. The age-adjusted incidence rate increased with age; the highest rates were 42.6% in the 75–79 years group. Patients older than 65 years old accounted for median 31.0% of number of patients and 40.1% of medical expenses over 5 years. Lumbar disc herniation (M51) and spinal stenosis (M48) might accounted for both the highest incidence and medical expenses in patients under the age of 60 and over 60 years, respectively.
Conclusion
The incidence and medical expenditures of spinal disease increased continuously. As the population of ROK in aging, the incidence and medical expenditures due to spondylosis and stenosis (M48) for the old are also increasing. The social burden of spinal diseases in elder patients needs to be prudently considered in health policy makers.
Keywords: Epidemiology, Spine, Cost, Socioeconomic status, Nationwide
INTRODUCTION
Spinal and spinal nervous diseases are some of the most frequently encountered problems in clinical medicine [1]. Lower back pain affects up to 80% of the global population at some point in life, and 1% to 2% of the United States adult population is disabled due to lower back pain [1,2]. Back and neck pain are 2 of the most common reasons for visits to primary care physicians in the United States and cause considerable disability and financial burden [3]. Similar to the existing trend in the Republic of Korea (ROK), the incidence of disc herniation was the highest globally in 2014 [4]. Moreover, degenerative spinal diseases are also increasing in incidence as the average life span increases [5]. Although most spinal diseases are not fatal, their associated morbidity exerts an enormous toll from both personal and societal perspectives [3]. The substantial medical needs of affected patients, coupled with our poor understanding of the epidemiology of spinal diseases, have led to an ever-expanding array of medical costs and treatment options [6,7]. The estimated direct total medical expenditure in the United States for spinal care in 2006 was more than $85 billion, and the data suggest that the use and costs of spine care have been increasing at an alarming rate in recent years [7].
Despite the vast amount of research devoted to spinal diseases, the epidemiology of this condition is not well understood, and the overall prevalence is unclear in many countries, even in the United States [7,8]. The ROK has a National Health Insurance Service (NHIS), which is a compulsory social insurance system that insures approximately 97% of the population [9]. The majority of remaining 3% of population is covered by Medical Aid [9]. All hospitals and clinics in the ROK submit medical records including diagnosis and operation codes of patients covered by the NHIS or Medical Aid to a Health Insurance Review & Assessment Service (HIRA) for review to be reimbursed for any healthcare services provided [9]. The HIRA database nationally representative and contains data on multiple variables important to epidemiological research, such as diagnosis, treatment, procedures performed, surgical history, and treatment prescriptions.
The goals of this study were to describe the incidence and analyze trends related to spinal diseases based on a nationwide database in the ROK and to elucidate the health care burden for researchers, clinicians, patients, and families. Additionally, we aimed to investigate the distribution of medical expenses based on sex, age, and diagnostic code associated with spinal diseases.
MATERIALS AND METHODS
This study involved a retrospective analysis of data obtained from Healthcare Bigdata Hub, the Korean Statistical Information Service (KOSIS), and Open Data Portal from 2012 through 2016. The Healthcare Bigdata Hub, KOSIS, and Open Data Portal are maintained by the HIRA, Statistics Korea, and Ministry of the Interior and Safety, respectively. These databases include records of all patients who receive care at all Korean hospitals and clinics, and medical costs based on disease codes, age, and sex. The database included the beneficiaries of the NHIS and did not included population of Medical Aid. The data were acquired by disease codes according to the Korean Standard Classification of Diseases, seventh edition [10] as same as the International Classification of Diseases, Tenth Revision (ICD-10) [11].
1. Inclusion and Exclusion Criteria
We identified patients with spinal diseases and classified them according to the following ICD-10 codes for spinal diseases: deforming dorsopathy (M40–43), spondylopathy (M45–49), and other dorsopathy (M50–54) (Table 1). Data for patients treated with these disease codes as a main diagnosis were included in this study. Patients diagnosed with these disease code as an accessory diagnosis were not included. Patients with spinal diseases due to congenital disease or trauma were excluded. The entire population data of the ROK were imported from the KOSIS census data to calculate the proportions of patients treated with spinal diseases relative to the entire population.
Table 1.
Definition of spine disease
| Codea | Inclusion | Codea | Exclusion |
|---|---|---|---|
| M40 | Kyphosis and lordosis | Q76.2-4 | Congenital kyphosis and lordosis |
| M41 | Scoliosis | ||
| M42 | Spinal osteochondrosis | M96. | Postprocedural kyphosis and lordosis |
| M43 | Other deforming dorsopathies | Q76.3-4 | Hemivertebra |
| - Spondylolisthesis | Q76.1 | Klippel-Feil syndrome | |
| - Recurrent atlantoaxial subluxation | |||
| M45 | Ankylosing spondylitis | Q76.4 | Lumbarization and sacralization |
| M46 | Other inflammatory spondylopathies | ||
| M47 | Spondylosis | Q76.4 | Platyspondylisis |
| - Degeneration of facet joints | M80-1 | Spinal curvature in osteoporosis | |
| M48 | Other spondylopathies | M88 | Paget disease of bone |
| - Spinal stenosis | |||
| - Ankylosing hyperostosis | |||
| M49 | Spondylopathies in disease classified elsewhere | M02.3 | Arthropathy in Reiter disease |
| - Tuberculosis | |||
| - Brucella | |||
| - Parasitic disease | |||
| M50 | Cervical disc disorders | M35.2 | Behcet disease |
| M51 | Thoracic, thoracolumbar, and lumbosacral intervertebral disc disorders | ||
| M53 | Other dorsopathy, NEC | M08.1 | Juvenile (ankylosing) spondylitis |
| - Cervicobrachial syndrome | |||
| - Spinal instabilities | |||
| M54 | Dorsalgia | G54.0 | Thoracic outlet syndrome |
| - Coccygodynia | |||
| - Radiculopathy | |||
| - Sciatica |
NEC, not elsewhere classified.
The International Classification of Diseases, Tenth Revision codes (ICD-10), 2016. World Health Organization. [11]
2. Data Variables
The total medical expenditure of beneficiaries of the NHIS in the ROK comprises paid medical expenses by insurers, copayments, unpaid medical expenses by insurers, and pharmacy preparation costs from pharmaceutical prescriptions. Copayments are paid by beneficiaries in addition to payments made by insurers, and made up 5%–20% of the total costs of items covered by the NHIS. Unpaid medical expenses by insurers are costs of devices or services which are not covered by the NHIS, and are paid by the patients themselves. Medication costs are shared between the insurer and the beneficiary, with the beneficiary paying 30%–50% of the medication cost.
Medical expenditure was calculated in Korean won (KRW, ), and converted to United States dollars (USD, $) using the average exchange rate from 2012 to 2016. We tried to demonstrate the costs in both USD and KRW. Otherwise, the standard unit of cost in this study was $, and the raw data for KRW are described in Supplementary Table 1.
3. Analysis
The statistical analysis was mainly descriptive to determine the annual trends in the number and cost of spinal diseases as well as the differences in age, sex, and disease code distributions. Chi-square tests were used to identify any differences in the distribution of numbers and costs by age, sex, and disease code. A p-value of <0.05 was regarded to be significant. Counts, means, rates, ratios, proportions, and other relevant statistics were calculated using R 3.4.3 (R Foundation for Statistical Computing, Vienna, Austria) and/or Microsoft Excel 2016 (Microsoft Corporation, Redmond, DC, USA).
RESULTS
1. Number of Patients With Spinal Diseases
Annually, 7,985,929 patients (men, 3,317,868; women, 4,668,061) among the 52 million of total population in the ROK were diagnosed with spinal diseases during the study period. The overall annual incidence rate of spinal diseases per 100,000 population was 15,743 (men, 13,042; women, 18,460) from 2012 through 2016 in the ROK; their trends are presented in Fig. 1. Over the study period, the annual incidence rate of spinal diseases rose continuously from 15,228 per 100,000 population in 2012 to 16,387 in 2016, which represents an increase of 7.6% over 5 years. Spinal diseases were more frequent among women than among men during the study period, and the sex ratio was 1:1.41 in 2014 (p<0.01). The annual sex ratio of spinal diseases changed from 1:1.46 to 1:1.38, suggesting a decrease in the incidence of spinal diseases among women over that period.
Fig. 1.

Average annual incidence of spinal diseases per 100,000 in the Republic of Korea from 2012 to 2016. The incidence increased in both male and female patients by 11.2% and 5.1%, respectively; the overall increase over the 5-year study period was 7.6%.
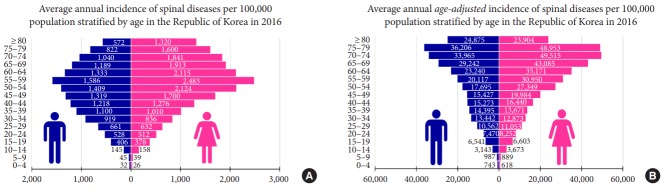
The incidence rate of spinal diseases based on age distribution is shown in Table 2. During the study period, there was no significant difference in the incidence across the years. In 2016, spinal diseases were the most common in the late 50s (55–59 years) age group (Fig. 2A). There were 1,586 men and 2,483 women per 100,000 population diagnosed with spinal diseases in that age group. Considering the age distribution of the population in the ROK, the age-adjusted incidence rate of which denominator is the population of same sex and age group in the ROK increased with age (Fig. 2B). The age-adjusted incidence rate increased rapidly in the 25–29, 50–54, and 65–69 years age groups. The age group with the highest incidence of spinal disease was the 75–79 years age group, with incidences of 42,580 (42.6%) per 100,000 population. The peak incidence rate stratified by sex and age group was 36,206 (36.2%) among men and 48,953 (49.0%) among women in the 75–79 years age group per 100,000 population of the same sex and age group.
Table 2.
The number of patients in spinal disease per 100,000 population stratified by age and sex
| Age (yr) | 2012 |
2013 |
2014 |
2015 |
2016 |
|||||
|---|---|---|---|---|---|---|---|---|---|---|
| Men | Women | Men | Women | Men | Women | Men | Women | Men | Women | |
| 0–4 | 24.6 | 20.2 | 29.9 | 24.1 | 28.5 | 22.9 | 30.1 | 24.1 | 32.5 | 25.8 |
| 5–9 | 44.6 | 38.1 | 42.9 | 37.3 | 44.4 | 38.3 | 42.2 | 36.0 | 45.3 | 38.6 |
| 10–14 | 178.4 | 186.1 | 167.4 | 180.5 | 164.2 | 183.4 | 150.2 | 165.5 | 145.4 | 158.1 |
| 15–19 | 377.1 | 347.7 | 371.5 | 354.0 | 401.4 | 389.6 | 397.8 | 378.4 | 405.8 | 377.9 |
| 20–24 | 420.6 | 433.4 | 441.4 | 449.9 | 487.4 | 494.9 | 493.3 | 489.7 | 528.0 | 511.7 |
| 25–29 | 628.0 | 621.3 | 616.7 | 602.2 | 648.9 | 617.4 | 639.0 | 603.0 | 660.8 | 632.2 |
| 30–34 | 900.3 | 846.7 | 934.5 | 860.1 | 981.1 | 890.2 | 925.9 | 832.5 | 918.7 | 836.1 |
| 35–39 | 1,014.9 | 1,020.9 | 1,017.4 | 981.8 | 1,047.7 | 988.2 | 1,044.4 | 960.0 | 1,100.3 | 1,010.2 |
| 40–44 | 1,161.5 | 1,371.8 | 1,185.3 | 1,338.4 | 1,232.0 | 1,349.1 | 1,211.2 | 1,284.0 | 1,218.0 | 1,275.7 |
| 45–49 | 1,194.2 | 1,711.9 | 1,186.7 | 1,649.4 | 1,263.2 | 1,705.0 | 1,256.8 | 1,655.2 | 1,318.6 | 1,699.9 |
| 50–54 | 1,423.8 | 2,395.8 | 1,439.6 | 2,339.7 | 1,461.3 | 2,317.1 | 1,413.9 | 2,189.7 | 1,409.0 | 2,124.3 |
| 55–59 | 1,274.8 | 2,129.0 | 1,322.5 | 2,153.3 | 1,436.3 | 2,290.0 | 1,477.8 | 2,332.4 | 1,586.0 | 2,483.5 |
| 60–64 | 1,125.9 | 1,852.3 | 1,133.6 | 1,838.3 | 1,170.9 | 1,889.3 | 1,219.2 | 1,954.8 | 1,332.8 | 2,115.4 |
| 65–69 | 1,069.6 | 1,867.5 | 1,059.7 | 1,796.3 | 1,117.2 | 1,843.1 | 1,134.2 | 1,840.3 | 1,189.3 | 1,913.1 |
| 70–74 | 1,017.8 | 1,915.0 | 1,062.9 | 1,958.1 | 1,070.2 | 1,963.9 | 1,047.3 | 1,886.1 | 1,039.6 | 1,840.7 |
| 75–79 | 653.1 | 1,351.9 | 699.7 | 1,418.9 | 757.3 | 1,515.0 | 784.0 | 1,544.6 | 822.0 | 1,600.1 |
| ≥ 80 | 382.8 | 965.0 | 420.6 | 1,035.1 | 468.2 | 1,127.2 | 515.3 | 1,218.8 | 571.6 | 1,319.5 |
Fig. 2.
The incidence of spinal diseases per 100,000 population in 2016. (A) The overall incidence was the highest among those aged 55–59 years; the age-group shows 1,586 male and 2,483 female patients per 100,000 population. (B) The age-adjusted incidences (age-adjusted to the age distribution of the entire population in the Republic of Korea in 2016) increased with increasing age. In the population aged 70–79 years, the average number of patients was 36,206 (36.2%) in men and 48,953 (49.0%) in women. Approximately 42.6% of the age-group population experienced spinal diseases.
Among 15,877 patients, the median annual incidence per 100,000 population, patients older than 65 years old was 4,969 (31.0%), which increased continuously (Table 3). During the study period, proportion of the age (≥ 65 years old) group among the entire population in the ROK increased from 11% through 12.7%. The annual incidence in the age group per 100,000 population of the same age (≥ 65 years old) group was 42,289 in 2012 and 40,897 in 2016, which demonstrated age adjusted incidence rate did not increased.
Table 3.
Statistics of the population over 65 years of age
| Item | 2012 | 2013 | 2014 | 2015 | 2016 | |
|---|---|---|---|---|---|---|
| Annual incidence of spinal disease in the olda per 100,000 populationb | Total | 4,656 | 4,763 | 4,969 | 5,032 | 5,193 |
| M/F | 3,148/6,183 | 3,262/6,282 | 3,433/6,522 | 3,509/6,572 | 3,650/6,749 | |
| Proportion of old patientsa in entire population in the Republic of Koreab | Total | 11.0% | 11.5% | 11.9% | 12.3% | 12.7% |
| M/F | 9.2%/12.8% | 9.7%/13.3% | 10.1%/13.8% | 10.5%/14.1% | 10.9%/14.5% | |
| Annual incidence of spinal disease in the olda per 100,000 population of the same age (≥ 65) groupb | Total | 42,289 | 41,484 | 41,639 | 40,831 | 40,897 |
| M/F | 11,659/8,120 | 10,985/8,143 | 11,086/7,917 | 10,866/7,544 | 11,013/7,277 | |
| Proportion of medical expense of the olda among the total patients with spinal diseasesc | Total | 38.6% | 39.5% | 40.1% | 40.3% | 41.2% |
| M/F | 32.2%/42.9% | 33.0%/43.9% | 33.5%/44.6% | 33.8%/44.8% | 34.6%/45.9% | |
| Rate of medical cost per old patient with spinal disease compared to average medical cost of all patients with spinal diseasesc | Total | 1.28 | 1.28 | 1.29 | 1.28 | 1.31 |
| M/F | 1.2/1.23 | 1.2/1.26 | 1.21/1.25 | 1.2/1.27 | 1.23/1.28 |
Patients older than 65 years old.
Denominator was both patients with spinal disease and the other population in the Republic of Korea.
Denominator was only patients diagnosed of spinal diseases.
2. The Distribution of Patients With Spinal Diseases Stratified by Disease Code, Age, and Sex
The distribution of patients with spinal diseases stratified by disease code is shown in Fig. 3. The most frequently reported disease code was dorsalgia (M54), followed by thoracic, thoracolumbar, and lumbosacral intervertebral disc disorders (M51), other spondylosis including spinal stenosis and ankylosing hyperostosis (M48), spondylosis (M47), cervical disc disorders (M50), other dorsopathies, not elsewhere classified (M53), and other deforming dorsopathies including spondylolisthesis and recurrent atlantoaxial subluxation (M43). The incidence ranking did not change substantially over the 5 years. M54 including radiculopathy, sciatica, back pain, and dorsalgia was the most common disease code and a symptom related code, and was usually used as a preliminary diagnosis before diagnostic workup. M51, including lumbar disc herniation was the second most common disease.
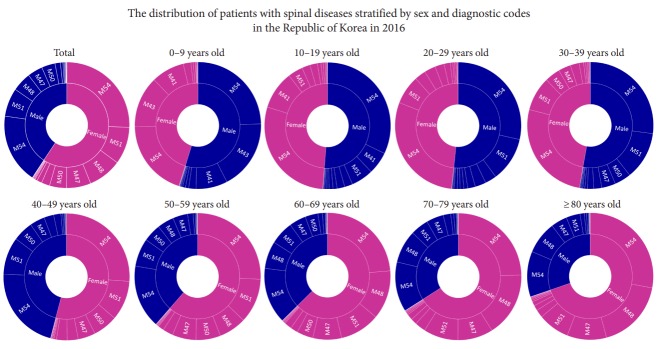
Fig. 3.

The average incidence of spinal diseases per 100,000 population stratified by disease code in the Republic of Korea from 2012 to 2016. The most common spinal disease code was dorsalgia (M54, red line), followed by thoracic, thoracolumbar, and lumbosacral intervertebral disc disorders (M51, pink line), other spondylosis including spinal stenosis and ankylosing hyperostosis (M48, black line), spondylosis (M47, blue line), cervical disc disorders (M50, navy line), other dorsopathy, not elsewhere classified (M53, brown line), and other deforming dorsopathies including spondylolisthesis and recurrent atlantoaxial subluxation (M43, light blue line). There were no substantial changes in the ranking of disease over the study period.
In 2016, the distribution of spinal diseases by disease code (ICD-10) and sex is depicted in Fig. 4. Among all the patients with spinal disease, the ranking of the top 5 conditions regarding incidence rate by patient number was the same in both sexes. Spinal diseases were more frequent among men younger than 39 years, and among women older than 40 years. Among children and adolescents aged 0–19 years, deforming dorsopathy (M40–43) was more common than that observed in other age groups. Among those younger than 59 years, disc herniation and radiculopathy (M51 and M54) was the most common regardless of sex. Among those older than 60 years, spinal stenosis and radiculopathy (M48 and M54) were the most common code for both sexes. Among patients at least 50 years of age, the incidence of spondylopathy including spinal stenosis (M45–49), increased rapidly with increasing age, while that of herniated discs (M50–54) decreased (Table 4).
Fig. 4.
Distribution of patients with spinal diseases stratified by sex and diagnostic codes in the Republic of Korea in 2016. There were more male patients than female patients among those younger than 39 years; however, there were more female patients older than 40 years. Deformity (M41) was common among patients aged 0–19 years. Among those younger than 59 years, diagnostic codes M54 and M51, mainly diseases with disc herniation, were the most common regardless of sex. Among those older than 60 years, M54 and M48 including spinal stenosis was the most common code for both sexes.
Table 4.
The number of patients stratified by common disease code, age, and sex
| Sex | Age (yr) | Deforming dorsopathy (scoliosisa) |
Spondylopathy (stenosisa) |
Other dorsopathy (herniated disca) |
||||
|---|---|---|---|---|---|---|---|---|
| M41b | M43b | M47b | M48b | M50b | M51b | M54b | ||
| Male | 0–9 | 3,006 | 6,624 | 312 | 133 | 90 | 58 | 9,147 |
| 10–19 | 17,313 | 3,142 | 6,212 | 1,397 | 3,022 | 17,130 | 96,827 | |
| 20–29 | 6,447 | 5,148 | 20,044 | 6,761 | 19,022 | 76,968 | 193,408 | |
| 30–39 | 3,337 | 6,121 | 41,272 | 18,747 | 49,383 | 141,886 | 314,266 | |
| 40–49 | 2,334 | 8,539 | 66,141 | 42,975 | 89,721 | 164,384 | 372,499 | |
| 50–59 | 1,912 | 14,975 | 98,153 | 108,781 | 117,875 | 184,900 | 416,239 | |
| 60–69 | 1,578 | 17,878 | 103,422 | 168,294 | 79,828 | 145,780 | 345,341 | |
| 70–79 | 1,153 | 12,671 | 90,029 | 170,832 | 38,947 | 93,728 | 258,821 | |
| ≥ 80 | 407 | 3,052 | 29,514 | 59,368 | 7,966 | 25,382 | 82,273 | |
| Female | 0–9 | 3,143 | 4,842 | 205 | 70 | 58 | 65 | 7,407 |
| 10–19 | 29,455 | 1,724 | 5,780 | 975 | 2,781 | 11,469 | 86,094 | |
| 20–29 | 10,786 | 2,927 | 19,446 | 4,616 | 19,493 | 50,079 | 198,424 | |
| 30–39 | 6,096 | 4,651 | 36,939 | 13,427 | 45,736 | 101,383 | 304,803 | |
| 40–49 | 4,751 | 10,949 | 77,436 | 48,370 | 109,007 | 174,698 | 450,954 | |
| 50–59 | 5,456 | 38,638 | 156,514 | 182,271 | 162,221 | 293,663 | 661,577 | |
| 60–69 | 4,773 | 46,190 | 177,667 | 301,635 | 100,896 | 247,322 | 570,388 | |
| 70–79 | 4,574 | 31,644 | 183,530 | 336,265 | 55,652 | 181,647 | 500,403 | |
| ≥ 80 | 1,523 | 7,673 | 71,961 | 127,425 | 14,316 | 57,384 | 198,937 | |
A representative common disease of each group.
Disease code of the International Classification of Diseases, Tenth Revision codes (ICD-10), 2016. World Health Organization. [11]
3. Medical Expenditure for Spinal Diseases
The mean annual medical cost per patient for spinal diseases rose continuously from $216.66 (248,080) in 2012 to $248.62 (284,660) in 2016, which represents a 14.7% increase over 5 years (Fig. 5). The medical costs for male and female patients increased by 13.9% and 15.4% over the 5 years, respectively. Male and female patients visited the clinic or hospital on an average of 6.25 and 7.45 times per year, respectively (p=0.74). Proportion of medical expenditure of patients older than 65 years old increased from 38.6% (men, 32.2%; women, 42.9%) in 2012 to 41.2% (men, 34.6%; women, 45.9%) in 2016 (Table 3). Average annual cost per patient older than 65 years old was approximately 1.28 times to that of total patients of spinal diseases.
Fig. 5.
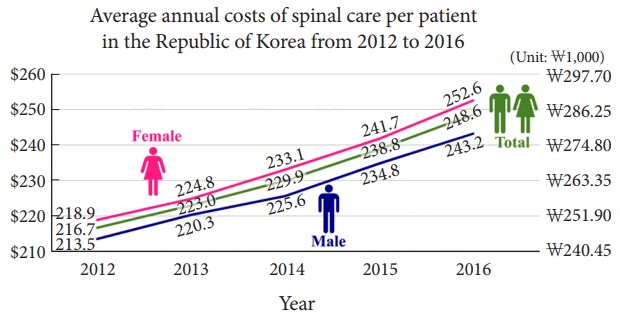
The average annual medical costs of spinal disease per patient in the Republic of Korea from 2012 to 2016. The cost increased from $216.66 (₩248,080) in 2012 to $248.62 (₩284,660) in 2016. Over the 5-year study period, the expenditure increased by a total of 14.7%; it increased by 13.9% and 15.4% for male and female patients, respectively. ₩, Korean Won.
The average medical cost per visit was $36.38 (41,660) among male patients, and $31.44 (36,000) among female patients. Although the medical cost per visit for female patients was cheaper than that for male patients, female patients had higher expenditure because of more frequent visit to the clinic than male patients.
The number of claims, total medical costs, and amounts of copayment per 100,000 population are shown in Table 5 (the expenditure in KRW is shown in Supplementary Table 1). Although the number of claims increased by 3.1%, the total medical cost increased by 23.5% over 5 years. Copayments also increased by 20.9% during the study period. An increase in medical cost per claim was estimated. In a comparison of the annual medical expenditure of inpatients and outpatients, the cost per outpatient visit increased by 18.3% over 5 years; however, that of inpatients decreased by 9.1%. The increment of medical expenditure over 5 years may be related to the increase in the cost of outpatient visits.
Table 5.
Number of claims and total medical cost per 100,000 population and mean copayment per each visit in the Republic of Korea from 2012 to 2016
| Service | Sex | Item | 2012 | 2013 | 2014 | 2015 | 2016 | Change ratec |
|---|---|---|---|---|---|---|---|---|
| Inpatient | Male | Number of claims | 990 | 1,086 | 1,260 | 1,217 | 1,266 | 27.9% |
| Total cost of medical care servicea | $933,304 | $957,539 | $976,210 | $998,868 | $1,086,929 | 16.5% | ||
| Mean copayment per visitb | $221.70 | $206.37 | $181.38 | $190.61 | $199.01 | -10.2% | ||
| Female | Number of claims | 1,359 | 1,453 | 1,657 | 1,634 | 1,717 | 26.3% | |
| Total cost of medical care servicea | $1,280,500 | $1,298,574 | $1,324,041 | $1,358,381 | $1,495,316 | 16.8% | ||
| Mean copayment per visitb | $224.70 | $212.49 | $190.28 | $196.26 | $204.89 | -8.8% | ||
| Both | Annual cost per one patient | $1,299.2 | $1,227.3 | $1,075.1 | $1,135.2 | $1,181.2 | -9.1% | |
| Outpatient | Male | Number of claims | 77,779 | 79,041 | 81,247 | 80,584 | 83,251 | 7.0% |
| Total cost of medical care servicea | $1,708,471 | $1,825,329 | $1,997,184 | $2,110,039 | $2,260,911 | 32.3% | ||
| Mean copayment per visitb | $6.48 | $6.80 | $7.17 | $7.72 | $8.05 | 24.2% | ||
| Female | Number of claims | 136,559 | 134,958 | 137,961 | 133,566 | 137,206 | 0.5% | |
| Total cost of medical care servicea | $2,681,180 | $2,775,211 | 3,007,798 | $3,101,778 | $3,309,188 | 23.4% | ||
| Mean copayment per visitb | $5.66 | $5.91 | $6.22 | $6.75 | $7.08 | 25.1% | ||
| Both | Annual cost per one patient | $145.2 | $150.9 | $159.5 | $166.2 | $171.7 | 18.3% | |
| Total | Number of claims | 108,240 | 108,190 | 110,981 | 108,419 | 111,645 | 3.1% | |
| Total cost of medical care servicea | $3,299,428 | $3,426,512 | $3,650,696 | $3,782,456 | $4,074,150 | 23.5% | ||
| Mean copayment per visitb | $8.32 | $8.63 | $8.94 | $9.57 | $10.05 | 20.9% |
The standard unit of cost is United States dollars, and the table in terms of Korean won (₩) is in the appendix Table 1.
Sum of payment by both insurer and beneficiary excluding unpaid items designated by insurer and pharmacy preparation costs by pharmaceutical prescriptions.
Copayment, a payment made by a beneficiary at each visit in addition to that made by an insurer.
Change rate, a rate over 5 years from 2012 to 2016.
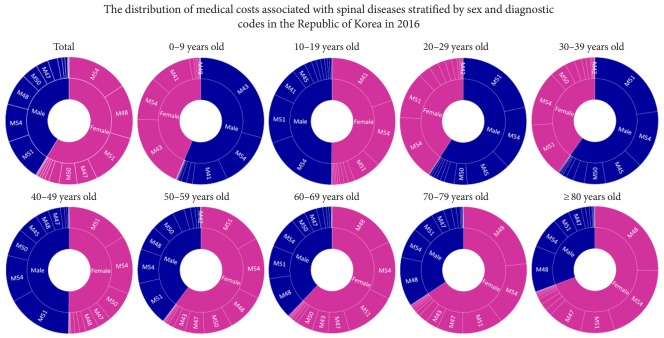
4. The Distribution of Medical Cost Stratified by Disease Code, Age, and sex
The total medical expenditure of spinal diseases per 100,000 population-year stratified by disease code is demonstrated in Fig. 6. The largest medical expenditure was spent on M51, followed by thoracic, thoracolumbar, and lumbosacral intervertebral disc disorders (M51), followed by dorsalgia (M54), other spondylosis including spinal stenosis and ankylosing hyperostosis (M48), cervical disc disorders (M50), spondylosis (M47), and other deforming dorsopathies including spondylolisthesis and recurrent atlantoaxial subluxation (M43). The medical cost of spondylopathy (M48) increased rapidly over 5 years and was close to that of M51 in 2016. The medical cost of radiculopathy (M54) showed a trend similar to M48, and comprised the highest medical expense in 2016.
Fig. 6.
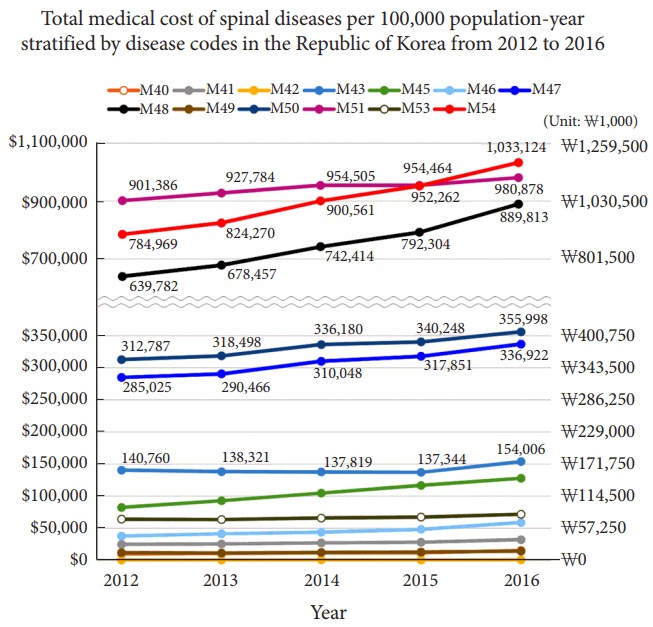
M51 (purple) accounted for the largest medical expenses, followed by M54 (red), M48 (black), M50 (navy), and M47 (blue). M48 (black) showed rapid increment and medical cost of M48 was close to that of M51 (purple) in 2016. M54 (red) also showed rapid increase similar to M48 (black), and surpassed M51 (purple) in 2016. ₩, Korean Won.
The distribution of the medical expenses stratified by age, sex, and disease codes in 2016 is shown in Fig. 7. In female patients, dorsalgia (M54) accounted for the largest proportion of total medical costs for spinal diseases followed by spondylosis and stenosis (M48) and herniated disc disorders (M51). In male patients, herniated disc (M51) accounted for the largest proportion of total medical costs for spinal diseases followed by dorsalgia (M54), and spondylosis and stenosis (M48). Among women and men younger than 19 and 9 years of age, respectively, deforming dorsopathy (M40–43) had the highest medical expenses. In patients at least 60 years of age, other spondylosis including spinal stenosis (M48) accounted for the largest proportion of total medical costs. Other spondylosis (M48) had the largest expenditure even though patients were frequently diagnosed with disc herniation (M51).
Fig. 7.
The distribution of medical costs associated with spinal diseases stratified by sex and diagnostic codes in the Republic of Korea in 2016. In total, the largest medical expenditure was on dorsalgia (M54), followed by other spondylosis including spinal stenosis and ankylosing hyperostosis (M48), and thoracic, thoracolumbar, and lumbosacral intervertebral disc disorders (M51). The ranking of medical expenditure did not exactly match the ranking of the number of patients. In patients aged 0–19 years, M43 and M41 including deformity accounted for the largest expenditure. Among those older than 60 years of age, M48, including spinal stenosis, it accounted for the highest expenditure for both sexes.
DISCUSSION
This study provides a comprehensive overview of the incidence and trends in spinal diseases in the ROK at the national level based on integrated data from the HIRA. The nationwide incidence of spinal diseases and medical costs increased continuously over the study period. While the incidence rate of spinal diseases was the highest among people in their 50s who mainly experienced disc herniation, the age-adjusted incidence rate was the highest among those in their 70s who mainly experienced spinal stenosis. M48 including spinal stenosis, which was frequent among older age groups, consumed more medical expenditure per patient.
The number of patients diagnosed with spinal diseases increased by 7.6% over the 5-year study period. As the age of population increased, the incidence of spinal diseases also increased and the peak incidence rate stratified by age was 42.6% in the 75–79 years age group. The reason for the increase in the number of patients may be related to the increase in the elderly population in the ROK because the age adjusted incidence rate of the population in ≥65 years old did not increase from 42.3% in 2012 to 40.9% in 2016, and proportion of the age group increased from 11.5% through 12.7% continuously as Korean society is aging. The population over 65 years of age in the ROK rapidly increased and made up 14.3% of the total population in 2018 [12]. The World Health Organization and the United Nations define an “aging society” as one in which more than 7% of the population in ≥65 years old, an “aged society” as a society in which more than 14% of the population is ≥65 years old, and a “super-aged society” as a society in which more than 21% of the population is ≥65 years old [13]. The ROK has become an aged society in 2018.
The number of claims increased by 3.1% over 5 years, with a 7.6% increase in the number of patients. The number of claims among male patients increased by 27.9% and 7.0% in both inpatient and outpatient clinics, and that of female patients increased by 26.3% and 0.5%, respectively. The reason for the mild increase in the number of claims may be due to the slight increase in claims among female outpatients who had the highest proportion of claims. They may have been hospitalized (as inpatients) and undergone surgical treatments instead of utilizing only outpatient services. Besides, the trend that male patients tend to have fewer hospital visits than female patients may be related with the result. Over the 5-year study period, the average cost per inpatient decreased by 9.1%, whereas the cost per outpatient increased by 18.3%. The reason for the increase in medical expenses was mainly due to +outpatient services. The reason for the increment in medical cost for outpatients may be related to pain interventions [14]. Further prospective studies are needed on this topic to find out this relationship.
Although the ICD-10 code is used worldwide, the code system cannot clearly distinguish specific diseases of the spine and some diseases have multiple codes. Moreover, M54 including dorsalgia, coccygodynia, radiculopathy, and sciatica was a symptom related code, and was usually used as a preliminary diagnosis before diagnostic workup. Thus, M54 was hard to regard as a primary disease code and excluded from this analysis. The largest medical expenditure was on thoracic and lumbosacral intervertebral disc disorders (M51) followed by dorsalgia (M54), and other spondylosis including spinal stenosis (M48). The medical expenditure on M48 increased rapidly during the study period, which may be due to the increased number of patients and medical cost per claim. The majority of spinal diseases differed by age and sex. Among individuals younger than 19 years, the most common spinal disease was scoliosis (M41), and might have been adolescent idiopathic scoliosis. In that age group, deforming dorsopathy (M40–43) had the highest medical expenses, which may be related to corrective surgeries for deformities due to adolescent idiopathic scoliosis. In patients younger than 39 years, the most common disease was lumbar and thoracic disc herniation (M51) and male patients accounted for the higher proportion. Disc herniation among young men may be related with hard work, vigorous physical activity, and obligatory military service. Among patients older than 40 years, females accounted for the higher proportion. Among patients at least 60 years of age, other spondylosis including spinal stenosis (M48) accounted for the highest incidence and the largest proportion of total medical costs. Spinal stenosis among elderly women may be related with degenerative change due to long kitchen work and farm work [15].
There are limitations that need to be acknowledged and addressed in the present study. The first limitation is with regards to the use of ICD-10 codes. ICD-10 codes are assigned for inpatient hospital diagnoses at discharge, and represent a patient’s diagnostic and procedural events [11]. However, studies utilizing ICD-10 codes in databases should be interpreted with caution, as their original purpose was not intended for research. Unfortunately, there is neither a specific term nor a specific diagnostic ICD-10 code to describe degenerative spinal diseases such as cervical spondylotic myelopathy, ossification of the posterior longitudinal ligament, and ossification of the ligamentum flavum [16]. This has resulted in the inconsistent use of diagnostic terms when referring to patients with these diseases, and subsequently, has given rise to ambiguity in critically exploring diagnoses, interventions, and outcomes for this prevalent and disabling set of conditions. A previous study has questioned the accuracy of administrative data for capturing clinical diagnoses [17].
The second limitation is the included population of this study. This study included only beneficiaries of NHIS, which is 97% of the total population in the ROK. The remaining 3% of the population was covered with the Medical Aids, and were applied totally different system from the beneficiaries of NHIS. Because their incidence and medical expenses were not disclosed to public, we analyzed the data from the beneficiaries of NHIS. Although this study did not include the entire population of the ROK, we think it would be more important to analyze the population of 97%, which is subject to common regulations by NHIS, for health policy formulation.
The third limitation is related to the accuracy of the medical expenditures to which the findings can be generalized. Among total medical costs comprising paid medical expenses by insurers, copayments, unpaid medical expenses by insurers, and pharmacy preparation costs, the unpaid expenses and pharmacy preparation costs were not included in the medical expenditure. Although these were a relatively small proportion of the total medical costs, estimation of the exact cost of medical expenditures need to be made with caution.
Finally, retrospective surveys obtain information directly from affected individuals but may be subject to recall bias. The claimsbased data used in our study may have enabled us to avoid this limitation; they are not dependent on individual reporting and only detect subjects whose physicians coded for back pain associated with a given episode of care [7]. Prospective methods of data collection for spinal diseases are superior for determining incidence and associations between patient characteristics, medical costs, and specific diseases.
CONCLUSION
This nationwide big data on spinal diseases from 2012 to 2016 in the ROK demonstrated increases in the incidence and medical expenditures due to spinal diseases. The reason of increase in the incidence and the expenses may be caused by increased population ≥60 years old as the Korean society is aging. M51 including lumbar disc herniation accounted for the highest incidence and the largest medical expenses in patients <60 years old, and M48 including spinal stenosis did in patients ≥60 years old. As the population of the ROK continues to age, the incidence and medical expenditures of spondylosis and stenosis (M48) are also increasing. The social burden of spinal disease in elder patient needs to be prudently considered in health policy makers.
Acknowledgments
CK Chung: This research was supported by a grant of the Korean Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI) funded by the Ministry of Health & Welfare, Republic of Korea (HC15C1320). CH Lee: This work was supported by the National Research Foundation of Korea (NRF) grant funded by the Korea government (Ministry of Education) (No. 2017R1D1A3B03028470).
Footnotes
The authors have nothing to disclose.
SUPPLEMENTARY MATERIAL
Supplementary Table 1 can be found via (https://doi.org/10.14245/ns.1836038.019).
REFERENCES
- 1.Andersson G. The epidemiology of spinal disorders. In: Frymoyer J, editor. The adult spine: principles and practice. 2nd ed. Philadelphia: Lippincott-Raven; 1997. pp. 93–141. [Google Scholar]
- 2.Deyo RA, Weinstein JN. Low back pain. N Engl J Med. 2001;344:363–70. doi: 10.1056/NEJM200102013440508. [DOI] [PubMed] [Google Scholar]
- 3.Vassilaki M, Hurwitz EL. Insights in public health: perspectives on pain in the low back and neck: global burden, epidemiology, and management. Hawaii J Med Public Health. 2014;73:122–6. [PMC free article] [PubMed] [Google Scholar]
- 4.Healthcare Bigdata Hub Frequent disease statistics of inpatients in 2014 [Internet] Available at: http://opendata.hira.or.kr/op/opc/olapHifrqSickInfo.do. Accessed Feb 14, 2018.
- 5.Kim CH, Chung CK, Kim MJ, et al. Increased volume of lumbar surgeries for herniated intervertebral disc disease and cost-effectiveness analysis: a nationwide cohort study. Spine (Phila Pa 1976) doi: 10.1097/BRS.0000000000002473. 2017 Oct 31 [Epub]. https://doi.org/10.1097/BRS.0000000000002473. [DOI] [PubMed] [Google Scholar]
- 6.Deyo RA, Mirza SK, Turner JA, et al. Overtreating chronic back pain: time to back off? J Am Board Fam Med. 2009;22:62–8. doi: 10.3122/jabfm.2009.01.080102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Friedly J, Standaert C, Chan L. Epidemiology of spine care: the back pain dilemma. Phys Med Rehabil Clin N Am. 2010;21:659–77. doi: 10.1016/j.pmr.2010.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Neuhauser H, Ellert U, Ziese T. Chronic back pain in the general population in Germany 2002/2003: prevalence and highly affected population groups. Gesundheitswesen. 2005;67:685–93. doi: 10.1055/s-2005-858701. [DOI] [PubMed] [Google Scholar]
- 9.Oh H, Boo S. Burns in South Korea: an analysis of nationwide data from the Health Insurance Review and Assessment Service. Burns. 2016;42:675–81. doi: 10.1016/j.burns.2015.10.005. [DOI] [PubMed] [Google Scholar]
- 10.Statstics Korea Korean Standard Classification Of Diseases. 7th ed (KCD-7) [Internet] 2016 Available at: http://kssc.kostat.go.kr/ksscNew_web/link.do?gubun=004#. Accessed August 2, 2018.
- 11.World Health Organization International Classification of Diseases [Internet] 2016 Available at: http://www.who.int/classifications/icd/en/. Accessed Feb 14, 2018.
- 12.Statistics Korea Estimated population in Republic of Korea [Internet] 2016 Available at: http://kosis.kr/conts/nsportalStats/nsportalStats_0102Body.jsp?menuId=10&NUM=1001. Accessed Feb 17, 2018.
- 13.Tahara Y. Cardiopulmonary resuscitation in a super-aging society - Is there an age limit for cardiopulmonary resuscitation? Circ J. 2016;80:1102–3. doi: 10.1253/circj.CJ-16-0307. [DOI] [PubMed] [Google Scholar]
- 14.Choi HJ, Hahn S, Kim CH, et al. Epidural steroid injection therapy for low back pain: a meta-analysis. Int J Technol Assess Health Care. 2013;29:244–53. doi: 10.1017/S0266462313000342. [DOI] [PubMed] [Google Scholar]
- 15.Lee CH, Chung CK, Jang JS, et al. 'Lumbar degenerative kyphosis’ is not byword for degenerative sagittal imbalance: time to replace a misconception. J Korean Neurosurg Soc. 2017;60:125–9. doi: 10.3340/jkns.2016.0607.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nouri A, Tetreault L, Singh A, et al. Degenerative cervical myelopathy: epidemiology, genetics, and pathogenesis. Spine (Phila Pa 1976) 2015;40:E675–93. doi: 10.1097/BRS.0000000000000913. [DOI] [PubMed] [Google Scholar]
- 17.Campbell PG, Malone J, Yadla S, et al. Comparison of ICD-9-based, retrospective, and prospective assessments of perioperative complications: assessment of accuracy in reporting. J Neurosurg Spine. 2011;14:16–22. doi: 10.3171/2010.9.SPINE10151. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Table 1 can be found via (https://doi.org/10.14245/ns.1836038.019).