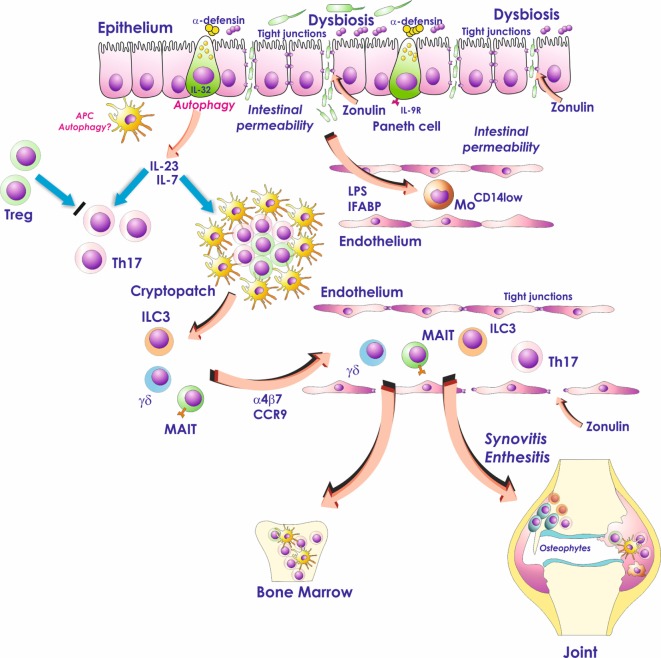
Figure 1.
Role of the gut inflammation in the pathogenesis of ankylosing spondylitis. Dysbiosis, occurring in the gut of AS patients, activates Paneth cells to produce antimicrobial peptides and possibly modulates the production of IL-23. Dysbiosis is also associated with zonulin-dependent alteration of both gut-epithelial barrier and gut-vascular barrier. The presence of altered epithelial and endothelial permeability is followed by the translocation in the systemic circulation of bacterial products such as lipopolysaccharide (LPS) and intestinal fatty acid binding protein (iFABP). These bacterial products may downregulate the expression of CD14 on circulating monocytes leading to an “anergic” phenotype. In the gut, IL-23 may induce the expansion of innate immune cells such as mucosal-associated invariant T (MAIT) cells, gd T cells, and innate lymphoid cells of group 3 (ILC3) that through the interaction with MAdCAM1 may recirculate form the gut to the sites of AS active inflammation.