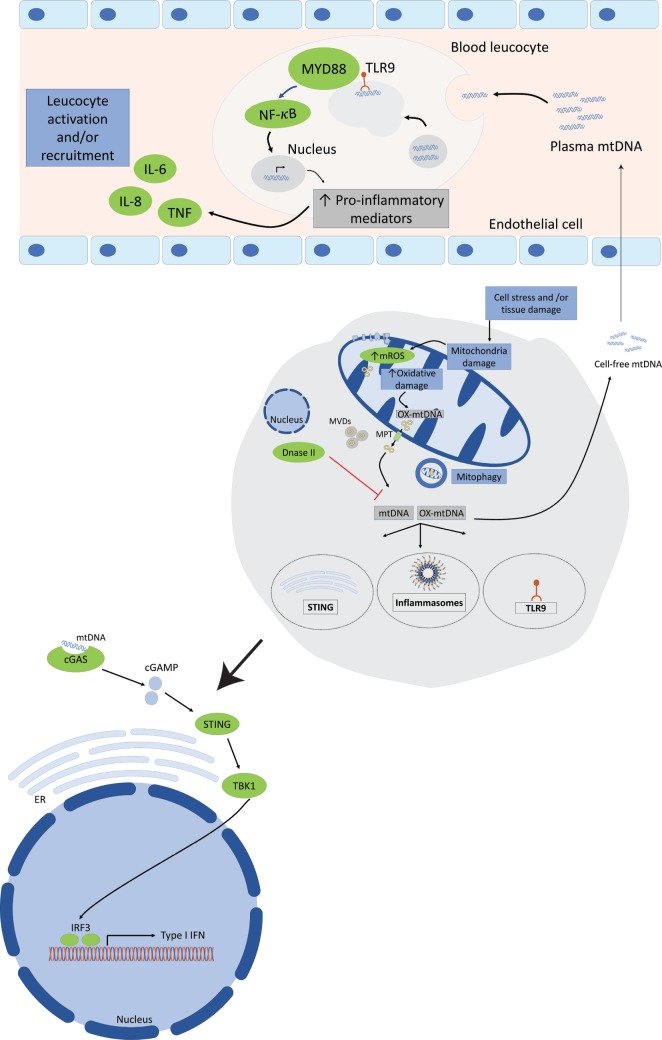
Figure 2.
Mitochondrial DNA (mtDNA) mediates a pro-inflammatory response by interacting with TLR9, cytosolic inflammasomes, and type I interferon response. Tissue injury or cellular damage can cause mitochondrial dysfunction resulting in oxidative damage with increased mitochondrial reactive oxygen species (ROS) production and mtDNA oxidation. Oxidized mtDNA will be released into the cytosol and then to the extracellular milieu by various mechanisms including the transport in mitochondrial derived vesicles (MVDs) or through mitochondrial permeability transition pores (MPT). The whole damaged mitochondria can also be recycled through the mitophagy process. In the plasma, mtDNA activates TLR9-mediated signaling pathway in circulating neutrophils resulting in increased production of pro-inflammatory mediators, such as tumor necrosis factor (TNF), interleukin-6 (IL-6), and adhesion molecules. Cytosolic mtDNA can also engage and activate the NOD, leucine-rich repeats, and pyrin domain-containing protein 3 (NLRP3) inflammasome or absent in melanoma 2 inflammasome and trigger a pro-inflammatory response in cells primed with first signal in inflammasome activation through the nuclear factor (NF)-κB pathway. Finally, cytosolic mtDNA can also be recognized by and engage the cyclic GMP-AMP synthase (cGAS). Once activated cGAS triggers conformational changes of the endoplasmic reticulum-resident protein stimulator of interferon genes (STING), which engages TANK-binding kinase 1 to activate interferon regulatory factor 3 (IRF3) and/or IRF7 to stimulate transcription of type I interferons (IFNs) genes.