Abstract
Purpose
The risk of ovarian failure after radiotherapy and/or chemotherapy is a concern among oncologic women. There is no doubt regarding the psycho-emotional benefits of fertility preservation (FP) after a cancer diagnosis because concerns about biological conception are a source of anxiety and can even affect the patient’s cancer recovery. The aim of this study was to evaluate oncology patients’ feelings, concerns, and life quality impacts related to FP.
Methods
This qualitative cross-sectional study was based on a questionnaire administered to a selected group of women diagnosed with cancer who underwent FP. Thirty-four eligible women (23–39 years old) completed this questionnaire.
Results
Two of the participants already had a child, and most of them (61.8%) stated a desire to have children at the time of FP. Their feelings primarily involved safety (44.1%) and hope (23.5%). Time and/or financial issues (82.4%) were the main challenge for FP. All of the women noted the importance of FP, with many stating that it is warranted to allow the possibility of a biological pregnancy due to the risk of infertility. Finally, questions about the impact on their lives if they had not undergone FP indicated emotional impairment, low quality of life, relationship problems, and uncertainty about maternity.
Conclusions
FP for oncology patients is a positive strategy. The women in this study felt that FP was a worthwhile process and that the security of having undergone FP brought them peace during oncological treatment and contributed to their quality of life.
Keywords: Fertility preservation, Oncofertility, Psychological aspects, Questionnaire, Nursing
Introduction
More than 35,000 women between 15 and 39 years old are diagnosed annually with cancer [7]. The incidence of cancer is rising globally, and breast cancer is the most commonly diagnosed type, accounting for 29% of all new cancer cases among women. Early diagnosis and the advancement of therapies have greatly improved the survival rate of cancer patients; in fact, the overall mortality attributed to cancer in women has declined by 1.5% per year in the last 5 years [18].
Consequently, there is an increasing number of young female cancer survivors, making the impact of treatment and its psychological implications of utmost importance. Among the consequences of treatment, one of the main concerns for female cancer survivors is fertility [12, 14]. Fertility issues are a consequence of treatment decisions for approximately one third of patients [15] and can have devastating effects on the quality of life of young oncology patients who did not have the opportunity to start a family before their diagnosis [19].
Although infertility risks after cancer treatment depend on multiple factors, such as the type of cancer, the type of surgery and therapy, and the woman’s age and reproductive health history, recent studies indicate that the iatrogenic potential for fertility loss can be more stressful than the cancer diagnosis itself. In addition to the physical consequences of chemotherapy and the associated emotional suffering, women may fear the loss of their dreams of motherhood and may feel they have lost their feminine identity. Facing both cancer and the probability of infertility makes the disease even more painful [14].
Discussing fertility preservation seems to benefit the psychosocial behavior of women since the impossibility of biological motherhood is a source of suffering. Preserving ovarian function can improve the quality of life of cancer survivors, specifically young women whose disease developed before they had the opportunity to start a biological family [5]. Nonetheless, health care professionals have difficulties communicating about fertility in the context of cancer [9].
Oncologists consider infertility caused by cancer treatment and the impossibility of motherhood a secondary problem in light of the diagnosis of malignant disease. Considering that the incidence of many cancers increases with age and that modern women tend to postpone maternity, it is likely that many cancer survivors who are interested in becoming mothers will not have the opportunity to do so before a cancer diagnosis [4]. Moreover, impacts of emotional impairment, relationship problems, uncertainty about maternity, safety, and low self-esteem on quality of life have been reported by young female cancer survivors [8, 19].
Based on this scenario, we conducted a survey of cancer patients who underwent fertility preservation at our center with the aim of understanding the importance of this procedure and the patients’ expectations regarding maternity and the use of the preserved tissues.
Methodology
Casuistic
This qualitative cross-sectional study was based on a questionnaire administered to a selected group of oncological patients who underwent fertility preservation (FP) from October 2012 to June 2016 at a private reproductive medicine center in Brazil. At the time of FP, all the patients signed the consent form and authorized the use of their data for scientific research. Additionally, the women who answered the questionnaire authorized the use of the data in scientific publications with respect for the anonymized handling of data according to ethical rules. Thus, approval for this study by an ethics committee was not required.
During this period, 45 oncology patients visited our service for fertility preservation. Of those, four did not undergo FP because of financial issues, four started ovarian stimulation but had their procedure canceled due to non-response, and 37 completed the procedure. Among the 37 women who underwent FP, 29 had oocytes cryopreserved (78.4%), five had embryos cryopreserved (13.5%), and three had ovarian tissue cryopreserved (8.1%) at least 6 months before the study was initiated. The patients were contacted by phone by a nurse, and the questionnaire was administered immediately by phone or sent by email when patients could not answer promptly. Three women (8%) did not answer the questionnaire, and 34 women were evaluated in this study.
Questionnaire
The instrument was an investigator-designed, self-reported questionnaire that included 17 questions addressing the following topics: sociodemographic characteristics (three multiple-choice questions), cancer history (three multiple-choice questions), indications for fertility preservation (one multiple-choice question), feelings about fertility preservation at the time of the procedure and at the time of the interview (eight multiple-choice questions), and the impact of fertility preservation on their lives (two open-ended questions).
The questionnaire was first designed and administered to five women to evaluate its functionality. We subsequently made some adaptations (mainly in the options for the multiple-choice questions), and the questionnaire was considered validated for use with other patients who were eligible for the study. The final questionnaire included 15 multiple-choice and two open-ended questions (Appendix 1).
Data analysis
Descriptive statistics were used to characterize the population. To evaluate cancer patients’ stated feelings before, during, and after fertility preservation, the answers were presented as frequencies and percentages. We used a chi-square test to compare the responses between subgroups. Data were analyzed with SPSS software (version 18, IBM, SPSS, Chicago, IL, USA).
Results
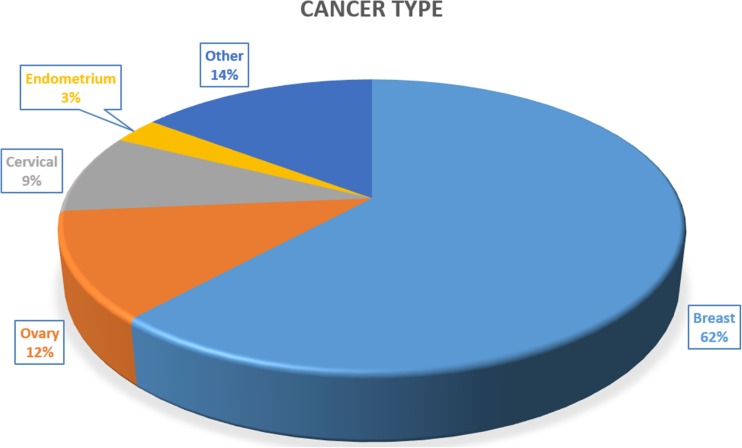
Thirty-four women aged 23 to 39 years (32.1 ± 4.9) answered the questionnaire. Most of the women (61.8%) were married or in a stable relationship. In a similar study, 73% of the patients were married or in a stable relationship [19]. Only two (5.9%) had children at the time of FP, and the most prevalent cancer type among the women who underwent fertility preservation was breast cancer (Fig. 1).
Fig. 1.
Distribution of cancer types among women who underwent fertility preservation
Fertility preservation was performed before any type of intervention in 41.2% of women. Another 52.9% had undergone a previous surgical procedure, and two women (5.9%) had undergone previous chemo-radiotherapy. The indication for FP was determined by oncologists (64.7%) or gynecologists (20.6%). However, some of the women (14.7%) obtained information on their own or received advice from friends and family. The questionnaire was administered 7 to 51 months after FP (18.6 ± 10.6 months). At the time of the questionnaire administration, the patients presented cancer remission (67.6%) or were undergoing treatment with a stable cancer evolution (32.4%). None of them had experienced cancer progression. The period (months) between FP and questionnaire administration for the cured participants (19.8 ± 11.0) and those with a stable cancer evolution (16.0 ± 9.7) was similar (p = 0.332).
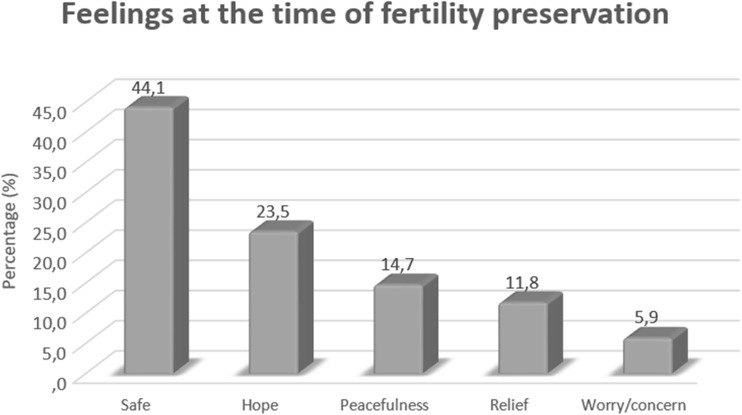
When they were asked about their feelings at the time of FP, 61.8% (n = 21) demonstrated a desire to have a child; among those, most were married (71.4%). In comparison, only 46.2% of the single participants reported wishing to have a child at the time of FP (p = 0.141). Emotions at the time of fertility preservation were positive in 94.1% of the women. Only two patients reported worry or concern (Fig. 2).
Fig. 2.
Feelings regarding fertility preservation at the time of the procedure
Because FP is not a clear option for most people, the difficulties associated with deciding whether to undergo FP were considered in our study. Half of the patients (50%) did not experience difficulty making the decision, whereas the other 50% (n = 17) reported some difficulties. The majority (82.4%) noted that time and/or financial issues presented challenges in terms of undergoing the procedure.
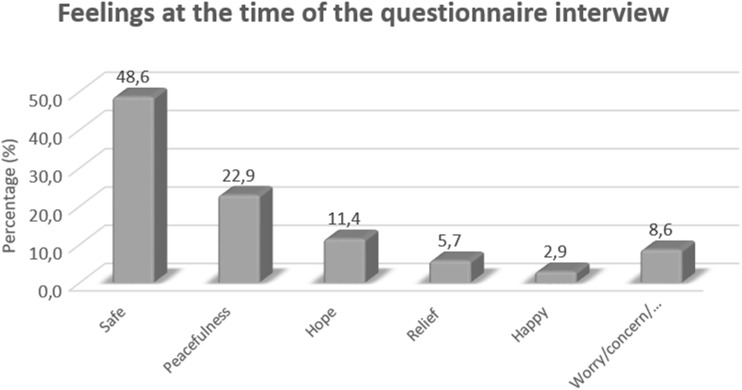
When we asked about the patients’ emotions at the time of the interview (at least 6 months after fertility preservation), most of the patients reported still feeling positive (91.4%) (Fig. 3).
Fig. 3.
Feelings regarding fertility preservation at the time of questionnaire administration
The women were unanimous in reporting that fertility preservation was very important to them, and 88.2% intended to use the cryopreserved material. Yee et al. [19] noted that fertility was identified as a vital survivorship issue for many respondents.
One woman had already attempted in vitro fertilization treatment with cryopreserved oocytes with no success, and one had experienced a spontaneous pregnancy. The reasons that fertility preservation was important were investigated using an open-ended question. The analysis of answers showed that the “possibility of becoming a mother in the future” was the main justification for FP, as stated by 79.4% of the women.
When the women were asked what the impact on their lives (in terms of quality of life and quality of their relationship) would have been if they had not undergone fertility preservation (open-ended question), only three patients said that it would not have had an impact on their lives. Others said that they would feel sorry, sad, frustrated, emotionally traumatized, and uncertain and would have experienced low self-esteem.
It is interesting that in the study by Yee et al. (2014), the patients noted that regardless of what the final FP decision was, almost all (97.6%) respondents replied that it was important to be informed about the options and the possibilities from a fertility preservation specialist.
Discussion
Modern anticancer treatments have led to significant reductions in mortality as well as to an increase in unwanted side effects, such as infertility [10]. Although the number of cancer patients undergoing FP remains low compared with the number of people diagnosed with cancer per year, fertility has been identified as the second most important factor for cancer patients who are considering treatment options, surpassed only by survival. FP offers hope and enhances self-competence in oncologic treatment decisions [11].
In 2013, more than 25% of the cancers diagnosed in women in Brazil were breast cancer [3], a proportion similar to the proportion of women with breast cancer seen at our center. However, it is interesting to note the high proportion of gynecological cancers in our population. This profile is consistent with the knowledge that the doctors involved in gynecologic cancer diagnosis and treatment are knowledgeable about fertility issues and options for FP due to their practice area. In Brazil, more than 35,000 women between 15 and 39 years are diagnosed with some type of cancer annually [7]. However, although our center performs approximately 4000 cycles of assisted reproduction treatments per year and has a specialized oncofertility team, the number of women seeking FP is extremely low: only 45 women in a period of 4 years (approximately ten per year). This finding corroborates with the situation in other countries, such as the Netherlands, where patients diagnosed with breast cancer or lymphoma were referred for FP more frequently than patients diagnosed with other malignancies [2].
Our data show that doctors indicated FP for most of the patients (85.3%), which probably encouraged the patients to seek the specialized service of FP. Nonetheless, we can speculate that most patients are not informed about infertility and FP because the number of women who come to our center is extremely small. Another drawback is the high cost of the procedure for FP, which is consistent with the main difficulties that our patients and other patients [17] reported, which were financial and time related.
Time is another important drawback because starting cancer treatment as soon as possible is a priority. More than half of the women in this study came to us after having undergone some intervention related to cancer treatment. Although most of these interventions were surgical procedures, two had undergone chemo-radiotherapy, which decreases the chances of successful FP. The women were not asked about their reasons for delaying FP, but we assume that the severity and evolution of the cancer may have influenced their scheduling of FP procedures. Supporting that hypothesis, other authors have reported that time is a negative factor associated with decisional conflicts regarding FP [1].
Reinforcing the high rate of cure for cancer patients, none of the women included in our study had disease progression. This situation further supports the importance of attention to quality of life issues, including FP, for such patients. This is in accordance with patients’ interest in becoming pregnant in the future and the positive feelings they experienced at the time of FP.
Many studies have indicated that biological pregnancy is a major issue for patients in their reproductive years who have cancer, particularly for those with a desire to have children [13]. In a recent study, when patients with a cancer diagnosis were asked about their experiences with potential loss of fertility, they used terms such as lonely, feeling alone, and being on their own [9]. Therefore, issues related to quality of life, such as fertility preservation, have become paramount in the lives of women of reproductive age who are fighting malignancies. Supporting this hypothesis, the majority of the patients in the present study (79.4%) cited the “possibility of becoming a mother in the future” as the most important reason for fertility preservation (79.4%). Moreover, most of them reported that if they had not undergone fertility preservation, it would have had a negative impact on their lives, highlighting the importance of FP for women of reproductive age.
Women with a cancer diagnosis face certain problems. First, oncofertility still faces resistance from oncologists because oncology patients normally have a short time for optimal treatment, and preservation strategies require part of this time. In 2016, a study acknowledged this point when and noted that oncologists often lack the necessary information and expertise in the fertility field, and, in practice, few patients are informed of the risks before the start of treatment, and even fewer are offered the possibility to preserve their fertility [16]. This attitude may change to one of individual support, and in time, medicine may consider humanization, autonomy, and quality of life pillars of treatment within any specialty. Another problem is a lack of knowledge regarding specific FP techniques, which prevents patients from considering assisted human reproduction options and leads to a loss of the possibility of biological maternity. In a recent study developed by our group that included 242 questionnaires distributed to the general population, only 34.0% of respondents were aware that cancer treatment can lead to infertility, and only 22.0% had heard about FP options [6].
Considering the aforementioned aspects, necessary aspects of a strategy to disseminate information about oncofertility and to provide knowledge of fertility preservation techniques to professionals directly related to cancer patients with potential for survival include the development of training, lectures, and fertility preservation specialists for cancer patients at oncology conferences as well as ongoing networking. In this way, the multidisciplinary approach and the outcomes for patients’ quality of life will be more successful.
Conclusion
There is no doubt that one of the greatest benefits of FP after a diagnosis of cancer is psychoemotional since the impossibility of achieving a biological pregnancy creates feelings such as anguish and fear in these patients. The hope of raising a child after a cancer diagnosis can contribute to better acceptance of oncologic treatment and its adverse effects. Our findings showed that patients have positive feelings about preserving their fertility; unfortunately, the number of patients referred for FP is still very small compared with the number diagnosed with cancer. Currently, the technologies available for oncological treatment are advanced and contribute to higher life expectancy and a greater chance of cure, making it possible for female cancer survivors to form their own biological families. This situation supports the need for oncologists to indicate FP whenever it is possible, thus giving patients the opportunity to experience a biological pregnancy, contributing to a higher quality of life, and encouraging positive thinking regarding cancer treatment.
Acknowledgements
We are very thankful to Huntington Medicina Reprodutiva for conducting the fertility preservation procedures and care for the cancer patients.
Appendix
Multiple-choice questions:
What was your marital status at the time of FP?
What is your marital status now?
Did you have children before FP?
What type of cancer were you treated for?
Did you have any type of cancer treatment before FP?
What is the current status of your cancer?
Who advised you regarding FP?
Did you want to have a child at the time of FP?
Do you want to have a child currently?
What was your feeling about FP at the time of the procedure?
Do you intend to use the cryopreserved material?
Do you consider it important to have FP?
What is your feeling about FP now?
What was your main difficulty regarding the decision to undergo FP?
What was your main difficulty regarding the FP procedure?
Open-ended questions:
If you answered YES to question 12, why do you think it was important to undergo FP?
If you had not undergone FP, would it have affected your life? For the open-ended questions, the answers were transcribed and evaluated qualitatively.
References
- 1.Bastings L, Baysal Ö, Beerendonk CCM, IntHout J, Traas MAF, Verhaak CM, Braat DDM, Nelen WLDM. Deciding about fertility preservation after specialist counselling. Hum Reprod. 2014;29:1721–1729. doi: 10.1093/humrep/deu136. [DOI] [PubMed] [Google Scholar]
- 2.Bastings L, Baysal, Beerendonk CCM, Braat DDM, Nelen WLDM. Referral for fertility preservation counselling in female cancer patients. Hum Reprod. 2014;29:2228–2237. doi: 10.1093/humrep/deu186. [DOI] [PubMed] [Google Scholar]
- 3.Brasil. Ministério da Saúde. Gabinete do Ministro. Portaria n° 874, de 16 de maio de 2013. Institui a Política Nacional para a Prevenção e Controle do Câncer na Rede de Atenção à Saúde das Pessoas com Doenças Crônicas no âmbito do Sistema Único de Saúde (SUS).; Brasília: Ministério da Saúde; 2013.
- 4.Carvalho BR. Oncofertility: foundations for bioethical reflection. Reprodução & Climatério. 2015;30:132–139. doi: 10.1016/j.recli.2015.11.003. [DOI] [Google Scholar]
- 5.Carvalho BR, Rodrigues JK, Campos JR, Marinho RM, Caetano JPJ, Silva ACJSR. An overview of female fertility preservation after cancer. Reproduçao & Climatério. 2015;29:123–129. doi: 10.1016/j.recli.2015.04.003. [DOI] [Google Scholar]
- 6.Chehin MB, Bonetti TC, Serafini PC, Motta ELA. Knowledge regarding fertility preservation in cancer patients: a population-based survey among Brazilian people during the pink October awareness event. JBRA Assist Reprod. 2017;21:84–88. doi: 10.5935/1518-0557.20170021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Coccia PF, Pappo AS, Altman J. Adolescent and young adult oncology. J Natl Compr Cancer Netw. 2014;12:21–32. doi: 10.6004/jnccn.2014.0004. [DOI] [PubMed] [Google Scholar]
- 8.Deshpande NA, Braun IM, Meyer FL. Impact of fertility preservation counseling and treatment on psychological outcomes among women with cancer: a systematic review. Cancer. 2015;121:3938–3947. doi: 10.1002/cncr.29637. [DOI] [PubMed] [Google Scholar]
- 9.Goossens J, Delbaere I, Beeckman D, Verhaeghe S, Van Hecke A. Communication difficulties and the experience of loneliness in patients with cancer dealing with fertility issues: a qualitative study. Oncol Nurs Forum. 2015;42:34–43. doi: 10.1188/15.ONF.34-43. [DOI] [PubMed] [Google Scholar]
- 10.Johnson JA, Tough S. Society of obstetricians and gynecologists of Canada, delayed child-bearing. J Obstet Gynaecol Can. 2012;34:80–93. doi: 10.1016/S1701-2163(16)35138-6. [DOI] [PubMed] [Google Scholar]
- 11.Kim SY, Kim SK, Lee JR, Woodruff TK. Toward precision medicine for preserving fertility in cancer patients: existing and emerging fertility preservation options for women. J Gynecol Oncol. 2016;27 [DOI] [PMC free article] [PubMed]
- 12.Lambertini M, Del Mastro L, Pescio MC, Andersen CY, Azim HA, Peccatori FA, Costa M, Revelli A, Salvagno F, Gennari A, et al. Cancer and fertility preservation: international recommendations from an expert meeting. BMC Med. 2016;14:1. doi: 10.1186/s12916-015-0545-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lee SJ, Schover LR, Patridge AH, Patrizio P, Wallace WH, Hagerty K. American society of clinical oncology recommendations on fertility preservation in cancer patients. J Clin Oncol. 2006;24:2917–2931. doi: 10.1200/JCO.2006.06.5888. [DOI] [PubMed] [Google Scholar]
- 14.Loren AW, Mangu PB, Beck LN, Brennan L, Magdalinski AJ, Partridge AH, Quinn G, Wallace WH, Oktay K. Fertility preservation for patients with cancer: American Society of Clinical Oncology clinical practice guideline update. J Clin Oncol. 2013;31:2500–2510. doi: 10.1200/JCO.2013.49.2678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Partridge AH, Gelber S, Peppercorn J, Sampson E, Knudsen K, Laufer M, Rosenberg R, Przypyszny M, Rein A, Winer EP, et al. Web-based survey of fertility issues in young women with breast cancer. J Clin Oncol. 2004;22:4174–4183. doi: 10.1200/JCO.2004.01.159. [DOI] [PubMed] [Google Scholar]
- 16.Preaubert L, Pibarot M, Courbiere B. Can we improve referrals for fertility preservation? Evolution of practices after the creation of a fertility network. Future Oncol. 2016;12(19):2175–2177. doi: 10.2217/fon-2016-0240. [DOI] [PubMed] [Google Scholar]
- 17.Samrsla M, Nunes JC, Kalume C, Cunha ACR, Garrafa V. Bioethical study on the expectations of women awaiting assisted reproduction in a public hospital in the Federal District, Brazil. Rev Assoc Med Bras. 2007;53:47–52. doi: 10.1590/S0104-42302007000100019. [DOI] [PubMed] [Google Scholar]
- 18.Siegel R, Naishadham D, Jemal A. Cancer statistics, 2013. CA Cancer J Clin. 2013;63:11–30. doi: 10.3322/caac.21166. [DOI] [PubMed] [Google Scholar]
- 19.Yee S, Abrol K, McDonald M, Tonelli M, Liu KE. Addressing oncofertility needs: views of female cancer patients in fertility preservation. J Psychosoc Oncol. 2012;30:331–346. doi: 10.1080/07347332.2012.664257. [DOI] [PubMed] [Google Scholar]