Abstract
Patent blue is one of the most used dyes for the identification of sentinel lymph nodes in breast cancer. This report describes a case of an anaphylactic shock reaction to patent blue dye in a patient with cross-reactivity to methylene blue. Therefore, after allergy confirmation, the operation was repeated avoiding blue dye and an alternative labelling technique with 99mTc albumin nanocolloids was used.
Keywords: anaesthesia, medical management, intensive care, immunology, healthcare improvement and patient safety
Background
Although neuromuscular blocking drugs, latex and antibiotics are the agents most frequently involved in perioperative hypersensitivity reactions,1 there are other more emerging causative agents.
Patent blue is a synthetic triphenylmethane blue dye, widely used in sentinel lymph node (SLN) biopsy in breast cancer, malignant melanoma and other malignancies.2 3 Its increasing use has led to the occurrence of allergic reactions,4 with features suggestive of IgE-mediated hypersensitivity. There are different degrees for immediate hypersensitivity reactions to patent blue described due to severity and their frequency as: grade 1 (69–87%): urticaria, pruritus, blue wheals and generalised rash; grade 2 (3.2–8%): transient hypotension (systolic blood pressure <70 mm Hg) with no need for vasopressors and/or bronchospasm/laryngospasm; grade 3 (1.1%): severe cardiovascular collapse with need for vasopressors and/or interruption of the planned procedure and/or hospitalization in intensive care; and grade 4 (<1%): respiratory or cardiorespiratory failure.5 Patent blue may also be referred as acid blue 3, disulfide blue and E131 when used as a food additive as a food colouring.3 6
Case presentation
We report a 54-year-old woman with ductal carcinoma in situ of the left breast, proposed for SLN and mastectomy, followed by reconstruction. The patient had a history of rhinitis, lactose intolerance and ofloxacin photosensitivity. After anaesthetic induction and 5 min after subcutaneous administration of 1 mL of blue patent (Guerbet, Sulzbach/Taunus, Germany), she presented with desaturation, tachycardia, hypotension, bluish skin eruption and cervical oedema. The other drugs administered up to the moment of the reaction were cefazolin, midazolam, fentanyl, propofol and rocuronium. The patient remained in hypotension for about 40 min and received treatment with intramuscular epinephrine and intravenous hydrocortisone, clemastine, ranitidine, ringer lactate and physiological serum. Surgical intervention was not performed, and the patient needed hospitalisation at the intensive care unit for treatment, having as additional complication a pneumothorax, probably iatrogenic, maybe due to a difficult orotracheal intubation, described in the surgical report. No tryptase assay was done. She had two previous surgeries, without complications. No prior medical contact with patent blue. She was next referred to our Allergy Department for study.
Investigations
At the Allergy Department, we performed 10 weeks later skin prick tests (SPT) and intradermal skin tests (IDT) with latex, rocuronium, cefazolin, propofol, fentanyl, midazolam, chlorhexidine and patent blue. We also tested, alternatively, SPT and IDT with methylene blue.
Differential diagnosis
The hypotheses of latex allergy, neuromuscular relaxant, cefazolin, propofol, midazolam and fentanyl were excluded by both negative SPT and IDT, according to non-irritating concentrations described in the literature. Also chlorhexidine was tested which was negative on SPT and IDT.
The patent blue(Patentblau V 25 mg/mL, Guerbet) showed positive at SPT at a dilution of 1:1 (figure 1), and we did not perform IDT with patent blue.
Figure 1.
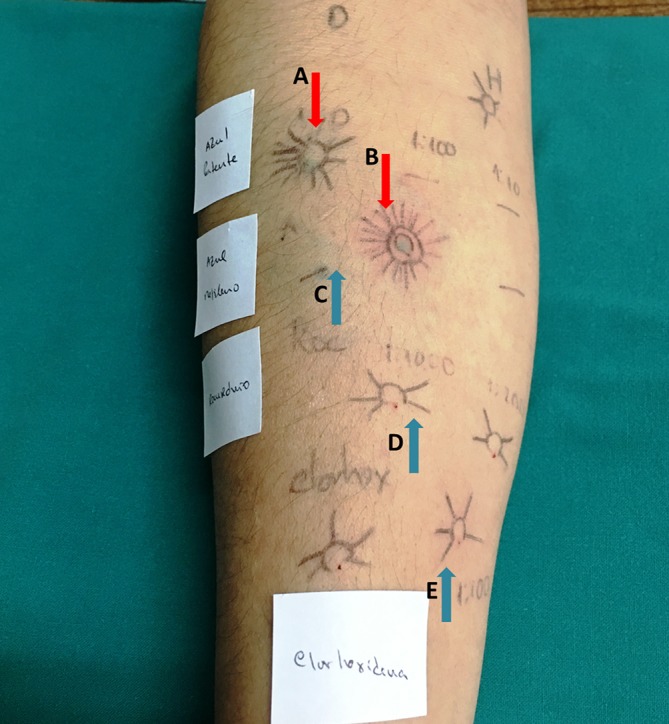
Skin prick tests and intradermal tests. The cutaneous positive reactions marked with red arrows is visible: (A) prick test with patent blue dye and (B) intradermal test with methylene blue. The blue arrows illustrate the negative cutaneous tests: (C) skin prick test to methylene blue; (D) prick and intradermal test with rocuronium and (E) prick and intradermal tests with chlorhexidine.
Methylene blue was also positive in the IDT only (dilution of 1:100), confirming an IgE-mediated mechanism in both dyes.
Outcome and follow-up
The patient was reoperated without the use of blue dyes and with all the other drugs used in the first surgery, without intercurrences. For SLN, lymphoscintigraphy was performed with 99mTc albumin nanocolloids.
Discussion
The cascade of the presented symptoms left no doubt that it was an anaphylactic reaction with shock; however, tryptase assay was not performed.
Allergic reactions to patent blue are rare but, when they occur, cases of anaphylaxis are common.5 7 In a multicentre retrospective study, Krishna et al8 reported patent blue dye as a culprit of anaphylaxis reaction in 5%–6% of cases in general anaesthesia procedures. Investigating the culprit and obtaining therapeutic alternatives is essential in perioperative anaphylaxis. Skin tests with patent blue were useful to confirm the diagnosis of allergy to this dye, as well as the timing of the reaction and its clinical complains. The immediate reaction, underlying specific IgE to patent blue, was also proposed by Woehrl et al.9 In this case we did not perform ELISA test. Even though methylene blue was positive in the IDT only, we can predict an IgE-mediated mechanism in both dyes.
Although structurally distinct, cross-reactivity was observed between the methylene blue and the blue patent. Basophil activation test has been useful in the diagnosis of blue patent allergy and on searching for safe alternative.10 In this case the methylene blue test, as a therapeutic alternative, was also important to identify a probable cross-reactivity between the two dyes that made it impossible to use it in the following surgery.
This patient had never contacted bluish contrast before. However, it is known that this dye may appear, in trace amounts, in some foods, which could explain a previous sensitisation.2 11 12
Patient’s perspective.
I have to admit that I always presented a very apprehensive posture during the skin tests procedures. I underwent two surgeries in the past without any complications and this particular episode was the source of many doubts and anxiety, considering that the mastectomy surgery should not be delayed for much longer.
After finding the culprit and the accomplishment of the surgery with alternative nanocolloids I became much more relieved and grateful.
Learning points.
All the drugs and antiseptics used in surgery, including latex, should be investigated in an anaphylactic reaction work-up study.
Even with a positive result for one culprit, the remaining drugs used should be excluded, at risk of a new allergic reaction, possibly of greater severity.
Searching for alternative is of utmost importance both to solve the patient’s problem and to assist the remaining clinicians in the approach and therapeutic options of the patient.
Even underlying a severe allergic reaction, surgery could be performed again without complications, and an alternative option was given to the patient.
No data are known about the possible eviction measures of future contacts, besides the surgical context.
Footnotes
Contributors: Skin tests were performed by CR and JPA. JPA and MA did the literature review and JPA was the main writer. ATB was the supervisor and elaborated the main take home messages. All authors approved the final version of the article.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Dong SW, Mertes PM, Petitpain N, et al. . Hypersensitivity reactions during anesthesia. Results from the ninth French survey (2005-2007). Minerva Anestesiol 2012;78:868–78. [PubMed] [Google Scholar]
- 2.Hunting AS, Nopp A, Johansson SG, et al. . Anaphylaxis to Patent Blue V. I. Clinical aspects. Allergy 2010;65:117–23. 10.1111/j.1398-9995.2009.02192.x [DOI] [PubMed] [Google Scholar]
- 3.Aurich S, Seitz AT, Tomm J, et al. . A case of anaphylaxis to patent blue in a patient with sentinel lymph node excision. Iran J Allergy Asthma Immunol 2016;15:547–50. [PubMed] [Google Scholar]
- 4.Martín-Lázaro J, Núñez-Orjales R, Battikhi-Precedo N, et al. . Allergy to blue dye. J Investig Allergol Clin Immunol 2016;26:381–3. 10.18176/jiaci.0101 [DOI] [PubMed] [Google Scholar]
- 5.Lanitis S, Filippakis G, Sidhu V, et al. . Atypical anaphylactic reaction to patent blue during sentinel lymph node biopsy for breast cancer. Ann R Coll Surg Engl 2008;90:338–9. 10.1308/003588408X285702 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hamelin A, Vial-Dupuy A, Lebrun-Vignes B, et al. . [Acute blue urticaria following subcutaneous injection of patent blue dye]. Ann Dermatol Venereol 2015;142:670–4. 10.1016/j.annder.2015.08.008 [DOI] [PubMed] [Google Scholar]
- 7.Mertes PM, Malinovsky JM, Mouton-Faivre C, et al. . Anaphylaxis to dyes during the perioperative period: reports of 14 clinical cases. J Allergy Clin Immunol 2008;122:348–52. 10.1016/j.jaci.2008.04.040 [DOI] [PubMed] [Google Scholar]
- 8.Krishna MT, York M, Chin T, et al. . Multi-centre retrospective analysis of anaphylaxis during general anaesthesia in the United Kingdom: aetiology and diagnostic performance of acute serum tryptase. Clin Exp Immunol 2014;178:399–404. 10.1111/cei.12424 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wöhrl S, Focke M, Hinterhuber G, et al. . Near-fatal anaphylaxis to patent blue V. Br J Dermatol 2004;150:1037–8. 10.1111/j.1365-2133.2004.05931.x [DOI] [PubMed] [Google Scholar]
- 10.Boita M, Mietta S, Bommarito L, et al. . Basophil activation test in the diagnosis of patent blue V anaphylaxis. Ann Allergy Asthma Immunol 2015;115:78–9. 10.1016/j.anai.2015.05.002 [DOI] [PubMed] [Google Scholar]
- 11.Shinzato JY, Marcaccini ACP, Braga AFA, et al. . Anaphylactic reaction to patent blue dye during sentinel lymph node biopsy in early-stage breast cancer - a case report. Rev Bras Ginecol Obstet 2006;28:728–32. [Google Scholar]
- 12.Scherer K, Studer W, Figueiredo V, et al. . Anaphylaxis to isosulfan blue and cross-reactivity to patent blue V: case report and review of the nomenclature of vital blue dyes. Ann Allergy Asthma Immunol 2006;96:497–500. 10.1016/S1081-1206(10)60921-0 [DOI] [PubMed] [Google Scholar]


