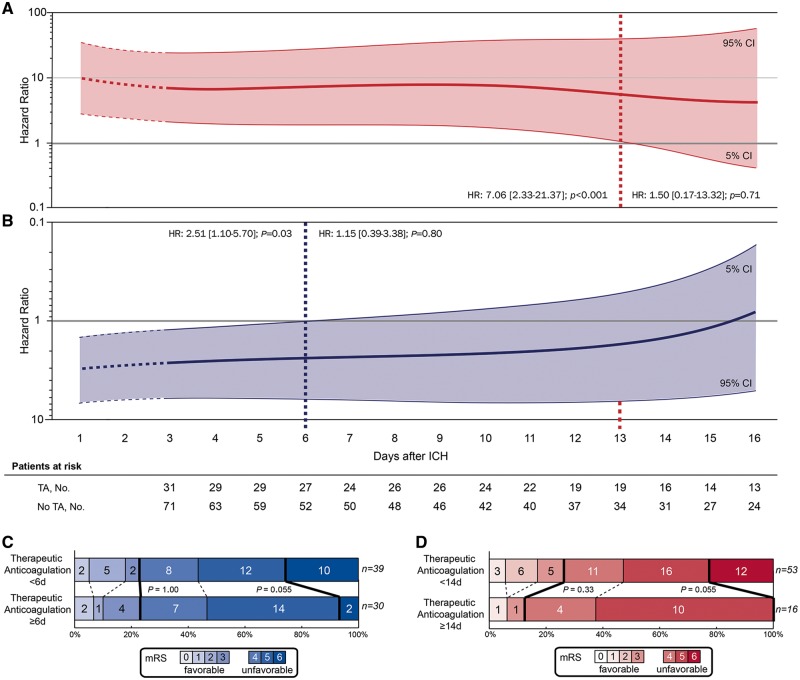
Figure 3.
Timing of therapeutic anticoagulation and clinical outcome. Adjusted cox proportional hazard models were used to visualize the association between the day of restarting therapeutic anticoagulation after intracerebral haemorrhage and (A) haemorrhagic complications and (B) the composite of haemorrhagic and thromboembolic complications during hospital stay. Patients were dichotomized according to treatment exposure (therapeutic anticoagulation vs. no therapeutic anticoagulation) and sequentially included into analyses at the day therapeutic anticoagulation was restarted. Specifically, we calculated hazard ratio estimates (y-axis) for both outcomes at each day after intracerebral haemorrhage using time-patient-clusters (3 day intervals) of patients that restarted therapeutic anticoagulation at a median of the presented day on the x-axis, and compared these with patients without therapeutic anticoagulation with available datapoints within these time-patient-clusters. Hazard ratio estimates were weighted and smoothed by the method of moving averages to correct for overestimation. ’Patients at risk‘ represents the number of individuals with attributed treatment exposure (either therapeutic anticoagulation or no therapeutic anticoagulation) at that specific day post-intracerebral haemorrhage. Stepwise-forward Cox proportional hazard modelling was adjusted for haemorrhagic and thromboembolic risk (CHADS2 and HAS-BLED scores) as well as for statistical imbalances among baseline characteristics (Glasgow Coma Scale, intracerebral haemorrhage volume). The thick lines (red for haemorrhagic complications, blue for the composite of haemorrhagic and thromboembolic complications) represent the hazard ratio estimates generated for every single day after intracerebral haemorrhage; the thin lines with shaded area indicate the 95% confidence intervals. The distribution of mortality and functional outcome (C and D) at discharge is displayed using the modified Rankin Scale. Analyses of in-hospital mortality and functional outcome at discharge in patients who received therapeutic anticoagulation (including three patients who died before 72 h but were restarted on therapeutic anticoagulation before) is displayed as dichotomized comparison at the identified time-threshold for (D) haemorrhagic complications and for the (C) composite of haemorrhagic and thromboembolic complications. Each score on the modified Rankin Scale is separated by dashed lines. Thick lines separate the proportion of patients with favourable (modified Rankin Scale 0–3) and unfavourable (modified Rankin Scale 4–6) outcome as well as patients with and without in-hospital mortality. HR, hazard ratio; ICH, intracerebral haemorrhage.