Abstract
Background: The evaluation of freestanding integrative cancer clinical programs is challenging and is rarely done. We have developed an approach called the Claim Assessment Profile (CAP) to identify whether evaluation of a practice is justified, feasible, and likely to provide useful information. Objectives: A CAP was performed in order to (1) clarify the healing claims at InspireHealth, an integrative oncology treatment program, by defining the most important impacts on its clients; (2) gather information about current research capacity at the clinic; and (3) create a program theory and path model for use in prospective research. Study Design/Methods: This case study design incorporates methods from a variety of rapid assessment approaches. Procedures included site visits to observe the program, structured qualitative interviews with 26 providers and staff, surveys to capture descriptive data about the program, and observational data on program implementation. Results: The InspireHealth program is a well-established, multi-site, thriving integrative oncology clinical practice that focuses on patient support, motivation, and health behavior engagement. It delivers patient-centered care via a standardized treatment protocol. There arehigh levels of research interest from staff and resources by which to conduct research. Conclusions: This analysis provides the primary descriptive and claims clarification of an integrative oncology treatment program, an evaluation readiness report, a detailed logic model explicating program theory, and a clinical outcomes path model for conducting prospective research. Prospective evaluation of this program would be feasible and valuable, adding to our knowledge base of integrative cancer therapies.
Keywords: Claims Assessment Profile, evaluability assessment, optimal healing environment, cancer research, complementary and integrative cancer evaluation
There are a growing number of complementary and integrative practices being adopted in cancer care, including development of cancer care centers and networks adopting complementary and alternative medicine (CAM) and integrating them with conventional cancer treatment. Sometimes referred to as complementary and integrative medicine (CIM), these clinics are often sought out by cancer patients, who are among the highest users of CIM.1 While research is growing on the use of supplements, acupuncture, herbs, and other modalities, few studies have been conducted on whole clinics that integrate many of these modalities. The Physician Data Query database maintained by the National Cancer Institute summarizes research on these modalities on a regular basis but finds few studies on combined integrative clinics.2 These clinics often claim to have very different types of practices and outcomes than their counterparts in conventional medicine, yet there are few systematic, in-depth evaluations of these types of clinics, their practices, their patients, and their clinical outcomes. Thus, objective information about what these practices do, how they are delivered, and the outcomes they provide to their patients remain unavailable to the public.
The concept of conducting CIM research within the practice setting is not unique. From 1995 to 1999, the National Institutes of Health, Office of Alternative Medicine (OAM) received a governmental mandate to document and evaluate alternative therapies and practices, especially in cancer. In collaboration with the Centers for Disease Control (CDC), the OAM developed the Field Investigation and Practice Assessment (FIPA) program that conducted evaluations of dozens of CIM practices around the world and made 33 site visits of CIM clinics with descriptions of the practices and what they did, their outcomes claims and rationale, and their capacity to do further research. The OAM followed up on initial site visits by contracting with the CDC to conduct formal field study investigations of promising clinical practices. An example of this work is a field investigation on naturopathy in the treatment of menopause symptoms.3 In addition, OAM, in conjunction with the National Cancer Institute (NCI), established the Cancer Advisory Panel for Complementary and Alternative Medicine to advise them on conducting a Best Case Series program.4 This program led to the development of large-scale randomized clinical trials to study therapies that offer promise for cancer outcomes, and evolved into using the best case series design to screen other therapies making claims of benefit for cancer patients.
However, the research methodology developed from these efforts never received adequate support for widespread application to CIM cancer therapies and so we are left with inadequate information on most practices. The Claims Assessment Profile (CAP) methodology utilized in this article is an attempt to continue to move these evaluations forward by systematizing and streamlining the ability to objectively evaluate CIM cancer treatment programs in the field. The CAP provides the primary descriptive and claims clarification of any integrative oncology treatment program, an evaluation readiness report, a detailed logic model explicating program theory, and a clinical outcomes path model for conducting prospective research. In short, the CAP process facilitates a collaborative process that enables the clinic to establish readiness for rigorous research on outcomes in order to demonstrate its value in cancer care. This article describes the CAP findings from one such CIM cancer center.
The integrative cancer care facility evaluated, InspireHealth, is an MD-led, comprehensive complementary cancer care center and an internationally recognized model in supportive cancer care. InspireHealth is funded through the British Columbia Ministry of Health Services, corporate and foundational support, as well as individual donations. Since 1997, the main clinical program in Vancouver, Canada, has provided integrative cancer care to over 6000 British Columbians. The second site in Victoria was is in its infancy at the time of this study with only 73 members and a growth objective of 10 to 12 members per month. A third site in Kelowna was slated to open doors later that year. The start-up for the Victoria and Kelowna locations were supported through a grant from the British Columbia Ministry of Health. Participants at InspireHealth generally receive their conventional cancer treatment at regional hospitals or at branches of the British Columbia Cancer Agency.
The central questions guiding this assessment were the following: What is the claim that InspireHealth makes about its impact on cancer patients, and what is the hypothesized process by which it may achieve its impacts on patients? Clarifying the objectives and hypotheses helps inform future research and demystifies the theories and practices that are embedded in such complementary treatment facilities.
The CAP evaluation was performed during site visits at InspireHealth clinics in Vancouver, British Columbia, and Victoria, British Columbia. This report details the methods, provides the results from the InspireHealth CAP, and concludes with a discussion of what these results mean in terms of practical applications.
Methods
Claim Assessment Profile Methodological Overview
The main objectives of the InspireHealth CAP were to (1) clarify, describe, and document the clinical practice in terms of care provided; (2) understand the implementation and delivery of services; (3) define expected changes in specific outcomes as a result of the program; and (4) determine readiness and ability of the practice to be involved in research. In order to explore these objectives, we utilize site visits, interviews, and observational data, as well as mind mapping exercises to create path and logic models.
The CAP method used here was further developed for CIM cancer care by building on the FIPA method described above. This began in 2003 under the Congressionally-mandated CAM Research for Military Operations and Health Care program run by Samueli Institute, and then as the Epidemiological Documentation Service (EDS) through a subcontract to the National Foundation of Alternative Medicine, with particular application to cancer. Perhaps the best examples from this phase were from Richardson and colleagues who collected descriptive and outcomes data from several oncology clinics that take a CIM approach to cancer therapy.5,6 They reported on both the feasibility and challenges of conducting outcomes research of CIM therapies in cancer clinics. Pfeifer and Jonas used a similar approach to investigate immuno-augmentative therapy, a CIM therapy used by thousands of cancer patients that had not been previously evaluated in a systematic fashion for either safety or efficacy.7 The EDS was later taken over by Samueli Institute where it was further developed and renamed SEaRCH, which contained the CAP as the initial descriptive phase of CAM evaluation.8
The current version of the CAP used here provides an in-depth “snapshot” of the characteristics of InspireHealth to determine whether the claims made by this program have a logical foundation in practice and whether it would be possible to collect data about the claim in the practice setting. The CAP draws on several established methodologies including program theory driven evaluation,9,10 rapid assessment procedures,11 and appreciative inquiry.12 The CAP produces a descriptive picture of the clinic. It explores clinical impact through a strengths-based evaluation approach by focusing the evaluation on positive impacts that clinic stakeholders believe to be results of program effects. The CAP is not intended to be an outcomes evaluation, but it is used for defining research questions, operationalizing variables, and as a first step toward determining the appropriate research designs.
This study gained approval for its protection of human subjects during research at the institutional review boards at Western IRB (WIRB).13 WIRB is compliant with US federal and state laws and regulations governing institutional review boards and research with human beings as well as with Canadian Tri-Council Policy Statement, Ethical Conduct for Research Involving Humans.
Characteristics of Key Informants
To obtain insights into the workings of InspireHealth and its readiness for evaluation, we interviewed administrators, providers, practitioners, staff, associates, and volunteers at two clinical sites. We interviewed staff in group collaborative conferences and through one-on-one interviews. We also spoke to participant members as they are key stakeholders who granted us insight into the most impactful elements of the care they received at InspireHealth.
At the Vancouver site (the parent integrative cancer care center that has been in operation since 1997), we interviewed 18 physicians, practitioners, staff, and members including the following:
Medical Director
Director of Healing
Director of Research
Director of Information Technology
Family practitioners (5 physicians in total)
Associates (work fee-for-service): Registered Holistic Nutritionist, Kinesiologist/Exercise Therapist, Registered Clinical Counselor, Integrated Body Worker, Registered Massage Therapist
Two participant members
At the Victoria site (the newer of the two sites), we interviewed the following 8 staff and patient members:
Medical Director
Physician
Office manager
Associates (work fee-for-service): Registered Holistic Nutritionist, Kinesiologist/Exercise Therapist, Yoga Instructor
Two participant members
Discussion Topics
We prepared discussion topics with semistructured questionnaires for focus groups and individual meetings with informants. We asked them about their patients, the care they provided, and how they conceptualized the causal links between this treatment and the positive outcomes they saw in patients. We also discussed research implementation issues to explore the feasibility of conducting different kinds of research and how each may have the least impact on clinical work. We further drilled into topics about specific measures or processes that providers believed should be captured and analyzed through evaluation research. We asked patients how they came to clinics, what kinds of impacts they were experiencing as a result of the care they received, and in order to gauge patient interest in research, we asked if they would consider participating in research if the clinic were to begin conducting studies.
We conducted brainstorming discussions with informants during focus groups about key outcomes that are most meaningful for patients. We drew on a white board diagramming a “mind map” of these concepts and drew causal links connecting them in order to understand their perspective on how and why the program works. The mind map is a diagrammatic method for recording knowledge and modeling systems whereby stakeholders identify keywords, concepts, and terms, sometimes starting with a main idea using size, color, shapes, and arrows to help reveal meaning to the words and concepts.14 The elements of the mind map diagram were used to inform a logic model and path model that are the initial steps toward designing research.
Data Collection and Analysis
A key component of rapid assessment processes is a constant interplay between the collection and analysis of the data. To address study objectives, we conducted site visits, focus groups, semistructured qualitative interviews, and surveys to capture descriptive data about the practice, and observational data on the implementation of the practice. Evaluation staff assessed readiness and resources of practice to engage in research by review of existing data collection capabilities with information technology and research staff. Interviews were conducted by a team of two professional staff using a protocol of semi-structured and open-ended questions and were digitally tape/web-recorded and archived. To reduce the costs of transcriptions, there was a note taker at each interview who archived field notes, which were reviewed during a debriefing sessions following the site visit. Data triangulation was utilized whereby concepts drawn by evaluation staff were reviewed with program staff and the medical director in order to gain multiple perspectives and confirm with staff and the director that we had adequately captured the concepts discussed.
Logic Modeling Process
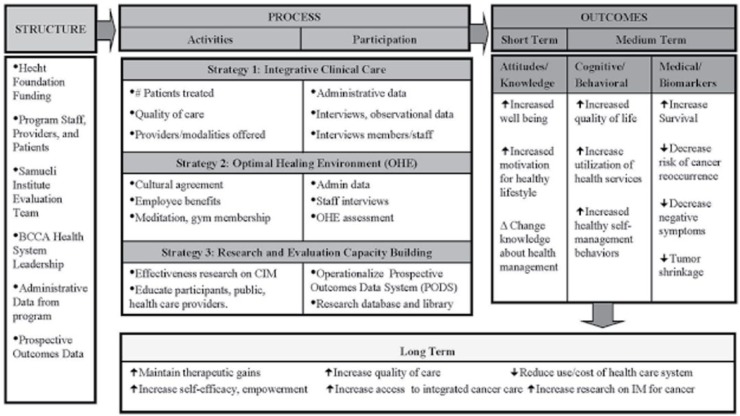
In order to operationalize the research methods described herein, a program theory-driven logic model of the clinic was utilized.10 This tool provides a snapshot of InspireHealth’s research plan and maps the program structure (such as funding for the work, partnerships, clinical mission, etc) to implementation components (strategies such as Integrative Clinical Care, Optimal Healing Environment, Research and Evaluation Capacity Building) and measures of outcomes to be analyzed (attitudes, knowledge, behaviors, cognitive, biomarkers). See Figure 1 for the InspireHealth program logic model.
Figure 1.
InspireHealth logic model.
Results
Description of the Program
InspireHealth clinics are integrative cancer care centers in Canada and are the only such clinics where the doctors are on salary from the British Columbia Ministry of Health. They were opened in 1997 by leaders in Canadian Integrative Medicine and were expanded in 2011 following a decision by the British Columbia Ministry of Health to provide additional funding for expansion.
Physician and Staff Information
At the time of the CAP there were 6 physicians working at InspireHealth; all of them licensed in family practice. In addition to the physicians, the program also employed two primary and three substitute yoga instructors and three additional holistic nutritionists to teach cooking classes. InspireHealth also included associate practitioners who work on a fee-for-service basis. Patients may be referred to associate practitioners by a medical doctor and patients can also choose to see associate practitioners independently of the physician referral. InspireHealth also involves volunteer providers, including a retired registered oncology nurse; a volunteer who teaches Emotional Freedom Technique; a shiatsu massage practitioner who teaches relaxation techniques to patients and their caregivers; prayer session facilitators; and a cancer patient who facilitates an advanced cancer support group. The ancillary personnel involved at the program include receptionists, an accountant, director of operations, director of research, director of healing environment, research associate, communications analyst, information technology specialist, events manager, human resources manager, and an executive assistant.
Locations and Details of Practice
InspireHealth has two primary locations. The clinics draw a majority of their patients from within a 50-mile radius. The Vancouver clinic is located within a large metropolitan area where the population is greater than one million people. The Victoria clinic is located on an island and draws from a population of approximately 350 000. Both clinics are located within urban settings and are stand-alone clinics operating independently of a hospital. A third site is in planning stages to be located in the more remote area of Kelowna, Canada.
Patient Demographics
Patients are referred to the clinics by word of mouth from current patients, family, or clinic staff. Some referrals come from providers at the local conventional cancer center. A small percentage of patients find it through advertisements and the program’s website. While gender and age information is collected, the clinic does not track patient demographics such as ethnicity, income, or education level. Referrals, gender, and age distributions of the caseload of current members are displayed in Table 1.
Table 1.
Patient Characteristics at Time of Evaluation (N = 588).
| Demographics | n | % |
|---|---|---|
| Referral type | ||
| Word of mouth | 347 | 59% |
| Family members | 106 | 18% |
| Referring providers | 53 | 9% |
| Clinic staff | 41 | 7% |
| Website | 29 | 5% |
| Advertisement | 12 | 2% |
| Gender | ||
| Female | 392 | 67% |
| Male | 196 | 33% |
| Age (years) | ||
| >17 | 0 | 0% |
| 17-44 | 123 | 21% |
| 45-64 | 353 | 60% |
| 65 and older | 112 | 19% |
The clinics are funded to treat primarily Canadian patients although there are some fee-for-service patients from outside of Canada. All patients receive outpatient care and pay an annual membership fee of $450; however, the total cost of care is estimated to be $2500. Since the Ministry of Health contributions do not fully cover the difference in cost of care, InspireHealth works to raise donations. Bursaries are also available for those who cannot afford the membership fee. Patients who join the program are referred to as “members” rather than patients. Additionally, a 30-minute consultation with a physician is free of charge and is available to non-members.
InspireHealth members have access to the following benefits:
A 90-minute visit with a physician. In this session the physician will address the patient’s questions and concerns that aids in the physician’s development of a personalized action plan specifically tailored to the patient. If needed, the patient will also have the option of 30-minute follow-up visits with the physician (in person or by phone).
A two-day educational and experiential “LIFE Program” is provided. Staff describe this as a life-changing experience facilitated by physicians and associate practitioners for cancer patients and their caregivers. The LIFE Program provides an introduction to what InspireHealth staff believes are the benefits and practical recommendations for self-care, including meditation and other mind-body practices, exercise, healthful nutrition, vitamins and supplements, and healthy communication.
Four two-hour group seminars titled “Body, Mind, Passion, and Spirit.”
Unlimited access to classes offered by the InspireHealth centers including relaxation, nutrition, group acupuncture (with the intent of reducing the side effects of chemo), meditation, hatha and laughter yoga, fitness, cooking classes, group support sessions, a specific support group for men, support groups for cancer patients and caregivers, Shiatsu, and Emotional Freedom Technique.
Consultations with naturopaths on supplements use.
Clinicians also document any concurrent conventional treatment the patient is receiving such as chemotherapy, radiation, and/or surgery. This is documented by including notes in the patients chart based on client self -report, records from conventional providers, and/or laboratory values such as blood tumor markers. The clinic does not provide conventional cancer treatments such a surgery, chemotherapy, and radiation, which are done by the local British Columbia Cancer Agency.
Types of Cancer and Other Conditions Treated
The types of cancer that patients present with at the program are listed in Table 2. The most common cancer diagnoses are breast, colon, prostate, and lung. All stages (Stage 0 to Stage IVB) and grades (Grade I-IV) of cancer are treated at InspireHealth. Currently, information about the stage and grade of cancer was not available in electronic records; however, stage and grade information is documented in patient charts. Additional comorbidities explicitly assessed at InspireHealth clinics through questionnaire are anxiety/depression, bowel problems or constipation, chronic pain, fatigue, neuropathy, problems sleeping, and weight problems.
Table 2.
Cancer Diagnoses for Current Patient Caseload During Evaluation Period (N = 588).
| Cancer Type | n | % |
|---|---|---|
| Breast | 192 | 32.7% |
| Colon | 48 | 8.2% |
| Prostate | 38 | 6.5% |
| Lung | 35 | 6.0% |
| Skin | 22 | 3.7% |
| Rectum | 21 | 3.6% |
| Brain | 17 | 2.9% |
| Leukemia | 17 | 2.9% |
| Urinary | 17 | 2.9% |
| Ovarian | 16 | 2.7% |
| Pancreas | 15 | 2.6% |
| Oropharynx | 14 | 2.4% |
| Thyroid | 10 | 1.7% |
| Multiple myeloma | 9 | 1.5% |
| Non-Hodgkin’s lymphoma | 9 | 1.5% |
| Stomach | 9 | 1.5% |
| Bladder | 8 | 1.4% |
| Hodgkin’s lymphoma | 8 | 1.4% |
| Lymphosarcoma | 8 | 1.4% |
| Uterus | 7 | 1.2% |
| Esophagus | 6 | 1.0% |
| Other types of cancera | 62 | 10.5% |
Other cancers include <1% of patients presenting with the following diagnoses: adenoid cystic, bile duct, biliary tract, bone, cervix, chronic lymphocytic leukemia, eye, gallbladder, kidney, larynx, liver, myelodysplastic syndromes, neuroendocrine, NH lymphoma, peritoneum, synovial sarcoma, testicle, tongue, tonsils, trachea, vulva cancer.
InspireHealth Program Philosophy
InspireHealth philosophy of care is centered on a concept refered to as “Transformational Medicine.” The clinicians and staff believe that by developing a deep rapport with each patient, they are able let go of judgments, projections, or assumptions surrounding the patient, and promote greater empathetic listening and patient-centered care. This allows the practitioners to provide individually focused suggestions for the patient’s healing journey that matches and encourages the patient’s own wisdom. Physicians and clinicians say they practice patient-centered and patient-empowered medicine with the goal of facilitating and igniting patient transformation. They believe in supporting patients in ways that can enhance their coping strategies and foster positive living and well-being.
InspireHealth providers believe that the clinic provides patients with a warm and welcoming healing environment and imparts cutting-edge information and direction about integrative cancer care that is evidence-based and wisdom-informed. This is accomplished in part though patient/physician collaborative co-creation of an individualized “Life Enhancing Health Plan.” They believe that through this process, patients gain a sense of confidence in their own inner resources and take charge of their lives. With that foundation, patients begin or grow in their capacity to take responsibility for their own healing and turn fear into hope and action.
Types of Treatment
The treatment modalities available at the clinic supporting the Life Enhancing Health Plan include the following: group and individual needle acupuncture, other acupuncture-based technologies (laser or other instrumentation), energy healing therapy, herbs/botanicals (recommendations made by physicians and naturopaths and purchased elsewhere), and manual therapies such as manipulation/massage, Reiki, meditation and other relaxation techniques, naturopathy, prayer/spiritual healing, yoga, laughter yoga classes, shiatsu classes, Emotional Freedom Technique classes, and nutrition and cooking classes for anti-inflammatory diets.
Patient and Clinician Reported Changes
InspireHealth clinicians report that the care has had a positive impact on mitigating conventional cancer treatment side effects and improving quality of life. They report that patients have informed them that the physical and psychological side effects from chemotherapy, radiation, and surgery are more manageable with less nausea, bowel issues, appetite problems, sweats and hot flushes, peripheral neuropathies, and skin changes. They say patients also report enhanced postoperative recovery.
Clinicians report that they have witnessed profound improvements in patient quality of life. They believe that this is a result of significant changes patients make in his/her life that has led to reduced stress and increased happiness. The changes they report witnessing include the following: setting clear and healthy professional and personal boundaries leading to healthier relationships and career choices; dietary changes and increased exercise that lead to healthier weights and higher self-esteem; relaxation practices that lead to more restful sleep and less daily stress. Patients reported that they experience an overall shift in attitude from “glass half empty” (cynicism and scarcity) to “glass half full” (curiosity, gratitude, and abundance).
Clinicians have documented the changes in patient symptoms and function including better sleep; appetite; mobility; activity; decreased pain, depression, and anxiety; better energy; increased happiness and joy in daily living; improved awareness and connection to innate passions and creativity; and improved relationships with self and others.
InspireHealth clinicians also report changes with respect to clinical response (eg, recurrence) as a result of treatment. They report observing improvement in patient survival and in managing cancer as a chronic disease. Increased completion of conventional therapy as a result of treatment at InspireHealth has also been reported. These improvements are due to increased tolerance to and compliance with chemotherapy cycles. Additionally, patients with advanced disease report that they have other options aside from conventional care and sometimes decline third-line palliative chemotherapy. InspireHealth clinicians also report that blood tests have shown stabilization or improvement in tumor markers, inflammatory markers, C-reactive protein, and blood cell counts. They report observing stabilization or reduction in tumors based on X-rays, computed tomography scans, magnetic resonance imaging, and colonoscopy reports. Physicians report cases of lung cancer patients whose disease stabilizes and disease stops progressing.
Side Effects
Side effects were reported as uncommon to InspireHealth treatments. At times patients have experienced gastrointestinal intolerance to particular supplements and in one case a patient experienced an allergic reaction. Participation in all the offerings at the clinic can be a challenge for some patients with advanced or painful cancer.
Data Capture
The following information on patients’ psychological health is collected and recorded through chart notes, verbal self-report, reports from associate practitioners, and consultation reports from conventional practitioners: psychological distress, anxiety, depression, fatigue, pain, other negative symptoms (eg, giving up hope), quality of life, positive affect, interpersonal functioning/social support, spiritual/religious practices, well-being, satisfaction with treatment, and other positive aspects. In addition to the information collected through verbal self-report are reports from associate practitioners and consultation reports from conventional practitioners, and biochemical and physiological markers. InspireHealth physicians typically receive information about endocrine markers and tumor markers reports from the patients’ conventional medical doctors but will occasionally order their own lab reports on tumor markers. Reports on immune markers and vitamin D 25-(OH) levels are regularly ordered by InspireHealth physicians.
Clarifying the Claim
In order to better clarify the precise nature of the claims and mechanisms at work, mind mapping focus group discussions were utilized to define outcome measures and operationalize variables.
Outcomes and Mechanisms of Action
An important facet of research feasibility is clarity on program goals and desired outcomes. At InspireHealth, a high level of evaluative thinking was displayed among staff, resulting in the creation of the logic and path models for the program. The ability of the practitioners to work together cohesively in their understanding of the program is a good sign of team care, research readiness, and development of appropriate and measurable outcomes. Our discussions with physicians, practitioners, staff, and patients elicited many ideas about which practices and/or processes were creating meaningful change and how that change might be measured. Improved quality of life, empowerment and self-efficacy, reduced cost of health care, and survival were commonly discussed as key outcomes. Other key outcomes mentioned were knowledge and behavioral changes, overall survival, recurrence rates, reduced side effects from conventional treatment, and tumor shrinkage. The group reached consensus on the types of activities they believe affect patients and defined short-, medium-, and long-term outcomes for the program logic model shown in Figure 1.
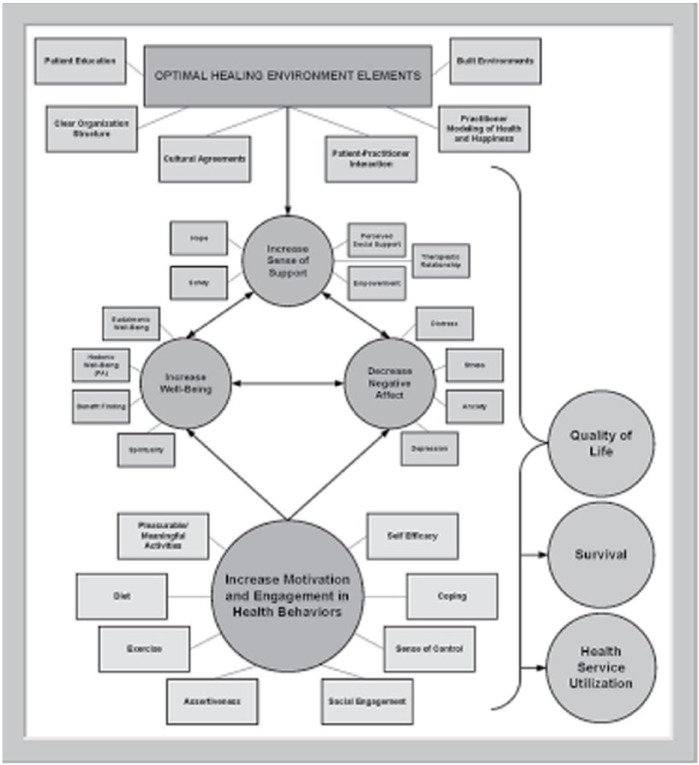
While the logic model shows a comprehensive picture of the structure, process, and anticipated outcomes, the causal path model focuses solely on outcomes and mechanisms of action. This tool can be used as an explanatory model for designing prospective research to test the anecdotal claims and mechanisms of action for resultant outcomes (quality of life, self-efficacy, and survival). The causal path model developed with the clinic during the CAP is shown in Figure 2.
Figure 2.
InspireHealth causal path model.
Future Research Capacity
The feasibility and capability of InspireHealth clinical staff to conduct research is an essential component in building a research program. Issues such as evaluative thinking, research resources, how and what outcomes should be studied, and other questions on research readiness were examined with the CAP.
Evaluative Thinking
As their mission statement suggests, InspireHealth wants to, “research effectiveness of an integrative approach on prevention, health, and healing.” The staff we interviewed embodied this message. From the Medical Director to front desk staff, enthusiasm and passion was apparent and their desire to have an evidence base behind their practices was clear. The Director of Research kept staff up to date on the latest findings in medical journals and how these findings apply to InspireHealth treatment protocols. There was an expressed desire by staff to create a research environment that propels their clinical work forward. This high level of evaluative thinking is an excellent foundation for continued research.
Research Readiness
Research was found to be feasible at InspireHealth. As stated above, part of the program’s mission is to research the effectiveness of an integrative approach to prevention, health, and healing. Past research efforts include retrospective studies, monitoring of health care utilization, and best case series. Current research involves investigating the efficacy of vitamin D in the management of late-stage colorectal cancer. There is a full-time research staff person to oversee these activities and others related to evidence-based medicine and practice. This research staff person also produces database updates for InspireHealth participants to access peer-reviewed literature, thereby building their evaluation capacity; An IT Director supports data elements of studies. InspireHealth has a staff and director who are motivated to enthusiastic about research. Therefore, evaluation capacity is high and research is feasible to conduct.
Discussion
InspireHealth is a well-established, thriving integrative oncology clinical practice. It encompasses two operational sites with one more site in the planning phase. There is a standardized treatment protocol, high patient throughput, federal funding, a high level of evaluative thinking, and good capacity for research.
The clinic also has a standardized protocol for the program, and newly hired physicians receive 3-week training to ensure that the values and practices of InspireHealth are incorporated similarly by all staff. While this process is highly structured, it would not be surprising to find variation in care between providers and between sites. There is currently not a process for monitoring quality or fidelity between sites. For instance, there is more focus on palliative care in Victoria and on adjunctive care in Vancouver. A provider with a stellar reputation in palliative care joined the Victoria site, which may explain the difference in care foci. This may affect propsective analysis of patient samples between the two sites. The limitations on future research may also include the limited space at the clinics. If a large-scale study were to be conducted, there needs to be increased space to support throughput of patients for study recruitment. While program staff highlighted expected outcomes such as better quality of life, higher levels of self-efficacy and empowerment, and survival, they did not mention characteristics like length of care in the program, which may also be a key variable influencing compliance, participation, and outcomes.
The anecdotal claims made by InspireHealth clinicians are bold and comprehensive, yet only if these are explicitly defined can they be rigorously researched. This was the first step in building clarity and understanding capacity for evaluation of this CIM program. The CAP for InspireHealth resulted in a subsequent prospective study being launched. In this case, the Claim Assessment Profile was an ideal first step to facilitate rigorous research on complementary and integrative oncology treatment.
Footnotes
Authors’ Note: We would like to acknowledge Drs. Hal Gunn and Janice Wright for collaborating by opening InspireHealth to external evaluation. The views expressed in this article are those of the authors and do not necessarily represent the official policy or position of the US Army Medical Command or the Department of Defense, nor those of the National Institutes of Health, Public Health Service, or the Department of Health and Human Services.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This project was partially supported by award number W81XWH-08-1-0615-P00001 (United States Army Medical Research and Materiel Command).
References
- 1. Adams M, Jewell AP. The use of complementary and alternative medicine by cancer patients. Int Semin Surg Oncol. 2007;4:10. doi: 10.1186/1477-7800-4-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. National Cancer Institute. PDQ® cancer information summaries: integrative, alternative, and complementary therapies. https://www.cancer.gov/publications/pdq/information-summaries/cam. Accessed October 7, 2016.
- 3. Cramer EH, Jones P, Keenan NL, Thompson BL. Is naturopathy as effective as conventional therapy for treatment of menopausal symptoms? J Altern Complement Med. 2003;9:529-538. [DOI] [PubMed] [Google Scholar]
- 4. Office of Cancer and Complementary Alternative Medicine. Case Review and Intramural Science Program. https://cam.cancer.gov/indentifying_novel_cam_therapies/default.htm. Accessed October 10, 2016.
- 5. Richardson MA, Russell NC, Sanders T, Barrett R, Salveson C. Assessment of outcomes at alternative medicine cancer clinics: a feasibility study. J Altern Complement Med. 2001;7:19-32. [DOI] [PubMed] [Google Scholar]
- 6. Richardson MA, Sanders T, Palmer JL, Greisinger A, Singletary SE. Complementary/alternative medicine use in a comprehensive cancer center and the implications for oncology. J Clin Oncol. 2000;18:2505-2514. [DOI] [PubMed] [Google Scholar]
- 7. Pfeifer BL, Jonas WB. Clinical evaluation of immunoaugmentative therapy (IAT): an unconventional cancer treatment. Integr Cancer Ther. 2003;2:112-113. [DOI] [PubMed] [Google Scholar]
- 8. Jonas WB, Crawford C, Hilton L, Elfenbaum P. Scientific evaluation and review of claims in health care (SEaRCH): A streamlined, systematic, phased approach for determining “what works” in healthcare. J Alter Complement Med. 2018.doi: 10.1089/acm.2016.0291 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Chen HT. Theory-Driven Evaluations. Newbury Park, CA: Sage; 1990. [Google Scholar]
- 10. Donaldson SI. Program Theory-Driven Evaluation Science: Strategies and Applications. New York, NY: Lawrence Erlbaum; 2007. [Google Scholar]
- 11. Beebe J. Rapid Assessment Process: An Introduction. Walnut Creek, CA: AltaMira; 2001. [Google Scholar]
- 12. Preskill H, Coghlan A. Appreciative Inquiry and Evaluation: New Directions for Program Evaluation. San Francisco, CA: Jossey-Bass; 2003. [Google Scholar]
- 13. Western IRB. https://www.wirb.com/Pages/Default.aspx. Accessed October 13, 2016.
- 14. Buzan T. The Mind Map Book. New York, NY: Penguin; 1996. [Google Scholar]