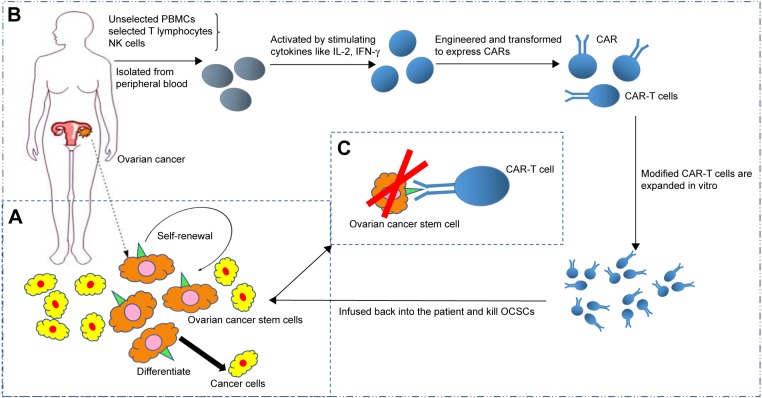
Figure 2.
The process diagram of CAR-T cellular immunotherapy targeting OCSCs.
Notes: This diagram describes how to design CAR-T cells which can recognize OCSCs and how CAR-T cells affect tumor as powerful weapon. (A) OCSCs have ability to self-renewal, asymmetrically divide, and differentiate into non-cancer stem cells in tumor architecture. The solid green triangle refers to the specific surface marker on OCSCs. (B) First, selected T cells are isolated from the patient’s peripheral blood (T cells with a higher ratio of CD4+/CD8+ are more effective, and some studies reported using unselected PBMC, NK cells, and so on). Second, the selected T cells are activated by cytokines like IFN-γ, IL-2 to enter an activated state for transduction. Third, the CAR is assembled on the T cell by lentiviral vectors or others (there are many methods to transfect CAR-T cells which are not narrated in brief here). Then, the modified T cells are expanded to a large amount to sacrifice the magnitude against tumor cells in vivo. Ultimately, CAR-T cells are infused back into the patient and a complete remission will be expected. (C) The CAR recognizes the specific surface marker of OCSCs, activates adoptive cellular immune defense, collects cytokines, and induces perforin/granzyme mechanism to kill the target cells. Notably, CAR-T therapy targeting OCSCs should be combined with other therapeutic methods.
Abbreviations: CAR, chimeric antigen receptor; OCSC, ovarian cancer stem cell; NK, natural killer; IFN, interferon; IL, interleukin; PBMC, peripheral blood mononuclear cell.